Abstract
Objective
The objective of this in vitro study was to investigate fracture load, fracture types, and impact of chewing simulation of human molars restored with 3D printed indirect polyetheretherketone (PEEK) inlays and compare these with milled indirect PEEK inlays, direct resin composite fillings, and sound teeth.
Materials and methods
A total of 112 molars with form congruent class I cavities were restored with (n = 16/group) 3D printed indirect PEEK inlays via fused layer manufacturing (FLM): (1) Essentium PEEK (ESS), (2) KetaSpire PEEK MS-NT1 (KET), (3) VESTAKEEP i4 G (VES), (4) VICTREX PEEK 450G (VIC), (5) milled indirect PEEK inlays JUVORA Dental Disc 2 (JUV), and (6) direct resin composite fillings out of Tetric EvoCeram (TET). Sound teeth (7) acted as positive control group. Half of the specimens of each group (n = 8) were treated in a chewing simulator combined with thermal cycling (1.2 million × 50 N; 12,000 × 5 °C/55 °C). Fracture load and fracture types of all molars were determined. Statistical analyses using Kolmogorov-Smirnov test and two-way ANOVA with partial eta squared (ηp2) followed by Scheffé post hoc test, chi square test and Weibull modulus m with 95% confidence interval were computed (p < 0.05).
Results
ESS and TET demonstrated the lowest fracture load with a minimum of 956 N, whereas sound molars showed the highest values of up to 2981 N. Chewing simulation indicated no impact (p = 0.132). With regard to Weibull modulus, KET presented a lower value after chewing simulation than JUV, whereas TET had the highest value without chewing simulation. All indirect restorations revealed a tooth fracture (75–100%), direct resin composite fillings showed a restoration fracture (87.5%), and 50% of the sound teeth fractured completely or had cusp fractures.
Conclusions
All 3D printed and milled indirect PEEK inlays as well as the direct resin composite fillings presented a higher fracture load than the expected physiological and maximum chewing forces.
Clinical relevance
3D printing of inlays out of PEEK via FLM provided promising results in mechanics, but improvements in terms of precision and esthetics will be required to be practicable in vivo to represent an alternative dental material.
Similar content being viewed by others
Introduction
Additive manufacturing (AM), also known as rapid prototyping, includes the manufacturing by 3D printing and enables the development of new material classes with more efficient and material-saving fabrication processes. Already today, 3D printing has a wide range of applications, such as dental restorations, implants, surgical guides, orthodontic devices, and physical models [1]. AM is also applied successfully in dental research, education, and training [2].
There are many advantages of 3D printing in dentistry, which improve the daily work of a dentist or dental technician and also the quality of patient life [3]. One of the biggest advantages is that patient-individual parts can be developed and produced with a minimum of time, amount of material, and cost. The mostly required postprocessing (e.g., removal of support structures, surface polishing) and an anisotropic behavior (mechanical properties depend on the printing direction) have to be mentioned as disadvantages [4].
AM is used in a digital workflow since the 1980s and consists of data acquisition (e.g., intraoral scan of patient teeth), designing the desired object by a CAD (computer-aided-design) software, dividing the object into many layers by a slicing software, and finally computer-aided manufacturing (CAM) with a 3D printing machine [5]. There are several different 3D printing techniques in dentistry such as stereolithography (SLA), selective laser sintering (SLS), digital light processing (DLP), and fused layer manufacturing (FLM) [4]. Since 2013, FLM is suitable for processing high-performance polymers from the group of polyaryletherketone (PAEK) [6]. PAEKs are semi-crystalline linear aromatic thermoplastics, whereby the number of ether and ketone bindings provides different variants, such as polyetherketoneketone (PEKK) and polyetheretherketone (PEEK), which have slightly different mechanical and thermal properties. In dentistry, PEEK is most common since it has outstanding properties, such as excellent biocompatibility, non-cytotoxical and bio-inert behavior, favorable mechanical properties, radio translucency, bone-like Young’s modulus of 3–4 GPa and low plaque affinity and chemical stability [7]. Until now, PEEK has been used in dentistry for removable and fixed dental prostheses, implants, and implant abutments as well as orthodontic devices [8], whereas in literature, it is mostly mentioned in relation to prosthetics [9]. PEEK was predominantly processed out of industrially pre-pressed pellets or granular form and CAD/CAM-supported milled out of prefabricated blanks. Producing dental restorations additively via FLM out of PEEK is still hardly widespread. With the FLM technique, the solid PEEK filament is melted in a nozzle and placed layer by layer onto the building platform in a specific laydown pattern. Critical factors are the required continuously high temperatures of over 350 °C, a special heat management of the nozzle, building platform and chamber to avoid nozzle blockage or material degradation and to achieve firm layer bonding as well as low component warpage [10].
Most restorative procedures involve massive reductions of tooth structure as the teeth have to be prepared. For example, when preparing class II cavities for an indirect restoration, more tooth structure is lost compared with preparations for direct restorations, which results in a lower tooth fracture strength [11]. Thus, occlusal preparations with a width of one-third of the intercuspal distance weaken the strength of a tooth by 60% [12]. However, indirect restorations offer some advantages over direct ones, such as better proximal and occlusal designs, higher wear resistance, superior mechanical properties, and more precise marginal adaptation, resulting in reduced microleakage [13].
Weibull statistics is particularly suitable in dental material research to characterize the failure and reliability of brittle materials such as ceramics and polymers [14]. The Weibull modulus m is a parameter for the dispersion of the strength values and provides information about the structural homogeneity of one material [15].
Besides this parameter, fracture load and durability to thermal stress are important factors that should be investigated before applying a new dental material in order to achieve an optimal clinical performance and a high long-term success.
Therefore, measuring fracture load and using a chewing simulator are proven in vitro methods to simulate mechanical properties of the material under masticatory movement and force effectively [16].
The aim of this study was to investigate the impact of chewing simulation combined with thermocycling on the fracture load of different 3D printed class I inlay materials compared with one milled PEEK material, one conventional direct resin composite material, and sound teeth. The null hypotheses tested were (1) the various restoration materials show no differences in the fracture load and (2) the fatigue process of chewing simulation has no impact on the fracture load of the restored teeth.
Materials and methods
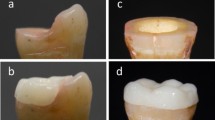
A total number of 112 human maxillary and mandibular extracted molars free of visible cracks, carious lesions, or restorative materials were collected for this study, which were stored in 0.5% chloramine T trihydrate (Carl Roth, Karlsruhe, Germany, CAS-No: 7080-50-4; Lot-No: 285228116) at room temperature (23 °C) for a maximum of 1 week after extraction and then in distilled water at 5 °C. All teeth were thoroughly cleaned, and their roots were embedded up to the cemento-enamel junction (CEJ) in a self-cured acrylic resin (ScandiQuick A and B, ScanDia, Hagen, Germany, Lot-No: 09201 and 09202) in round metal molds (Fig. 1a). Before measurement, the embedded molars were stored in distilled water at 37 °C in an incubator (HeraCell 150, Heraeus, Hanau, Germany), which was changed every week. All molars were randomly divided into seven groups (n = 16 teeth) with different restoration materials (Table 1). Occlusal class I cavities (vestibular-oral width of 3.0 mm, distal-mesial width of 6.5 mm, occlusal reduction of 4.0 mm, convergence angle of 6°) were prepared, except one group that served as an unprepared and unrestored control group. The preparations were made under permanent water cooling at 40,000 min−1/rpm with a conical diamond bur (6848.314.031, Gebr. Brasseler, Lemgo, Germany) in a high-speed handpiece (Perfecta 900, W&H, Laufen, Germany), which was mounted in a dental parallel surveyor (F4 basic, DeguDent GmbH, Hanau, Germany). Care was taken to always prepare cavities of the same size and depth, which was ensured with markings on tooth and bur (Fig. 1a). The molars were subsequently restored with indirect and direct restorations.
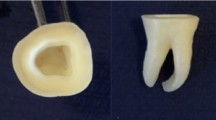
For this purpose, the prepared teeth for the indirect restorations were scanned with an optical 3D camera (CEREC Omnicam, Dentsply Sirona, Bensheim, Germany), inlays were designed by a CAD software (CEREC SW 4.6.1, Dentsply Sirona), and files were created in STL format (inLab CAD SW 18.1, Dentsply Sirona) (Fig. 1b). From each printable PEEK material (Essentium PEEK (ESS), KetaSpire PEEK MS-NT1 (KET), VESTAKEEP i4 G (VES), and VICTREX PEEK 450G (VIC)) (Table 1), 16 inlays were additively manufactured out of a filament (diameter 1.75 mm) via FLM with the printer HTRD1.2 (KUMOVIS, Munich, Germany) (Fig. 1c). Before manufacturing, the filament was dried in an oven (Heraeus RT 360, Heraeus) at 120 °C for 12 h in order to extract moisture and avoid artefacts such as air inclusions [6]. For better comparability, all materials were printed with the same parameters (Table 2). After the printing process was finished, the inlays were immediately removed from the building platform and cooled down at room temperature. Thus, support structures had to be removed with milling instruments (H73EF.104.014 and H136EF.104.016, Gebr. Brasseler) in a handpiece (KaVo EWL K9, KaVo Dental, Biberach/ Riß, Germany), the inlay had to be adapted individually to its cavity, and the occlusal surface had to be re-contoured (Fig. 2). Such postprocessing also had to be performed on the milled inlays made out of JUVORA Dental Disc 2 (JUV) (Table 1). These were milled out of a disc with a CAD/CAM milling machine (ZENOTEC 4030, Wieland Dental + Technik, Pforzheim, Germany).
After all inlays had been adequately adapted, they were adhesively inserted into the cavities. All inlays were air-abraded with 50-μm Al2O3 powder under 0.2 MPa for 10 s at a distance of 10 mm and in an angle of 45° (basic Quattro IS; Renfert, Hilzingen, Germany), conditioned with a thin film of visio.link (bredent, Senden, Germany) and light-cured for 30 s (bre. Lux LED N, bredent). The tooth-hard tissues were pre-treated using total etch technique, in which the enamel was etched for 30 s and the dentin for 15 s with a 35% phosphoric acid (H3PO4) (Total Etch, Ivoclar Vivadent, Schaan, Liechtenstein). Thereafter, according to the manufacturer’s instructions, Syntac Primer (Ivoclar Vivadent) was applied for at least 15 s, Syntac Adhesive (Ivoclar Vivadent) for 10 s, and both were gently air-dried. Subsequently, a thin layer of Heliobond (Ivoclar Vivadent) was applied in all cavities and light-cured for 10 s (Elipar S10, 3M, Seefeld, Germany) only for the direct composite fillings. The dual-curing Variolink Esthetic (shade warm+, Ivoclar Vivadent) was used as luting resin composite for the inlays, which was light-cured occlusally for at least 20 s (Elipar S10, 3 M) after the inlay was inserted. Finally, the bonded inlays were polished to high gloss with goat hair brushes (bredent) and polishing paste (Abraso Starglanz, bredent) for 1 min at 3000 min−1/rpm (KaVo EWL K9, KaVo Dental) (Fig. 1d).
The direct restorations were performed with the nanohybrid resin composite Tetric EvoCeram (TET) (shade A3, Ivoclar Vivadent) (Table 1). The cavities were filled using an incremental filling technique, where each layer (max. 2 mm) was light-cured for 20 s (Elipar S10, 3M). The polishing was carried out with a two-step polishing system (94028M.204.130 and 94028F.204.130, Gebr. Brasseler) for 1 min at 6000 min−1/rpm under permanent water cooling.
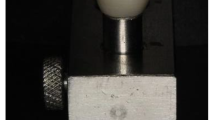
Eight teeth were selected from each of the seven groups. They were mounted in a chewing simulator (CS-4.8, SD Mechatronics, Feldkirchen-Westerham, Germany) for 1.2 million masticatory cycles with a frequency of 1.20 Hz and force of 50 N (Fig. 1e). The chambers were filled alternately for 12,000 cycles for 30 s each with 5 and 55 °C distilled water, so that in addition to mechanical loading, thermal cycling also took place simultaneously. Stainless steel balls out of chromium-nickel 1.4301 (diameter: 4.5 mm; SD Mechatronics) were used as antagonists and were aimed at a three-point occlusal contact. They moved in vertical (1.0 mm) and lateral (0.7 mm) directions as it occurs during physiological chewing. Subsequently, each single tooth was examined under a light microscope (Leica DM2700 M, Leica Microsystems GmbH, Wetzlar, Germany) for fractures that might have occurred during mechanical and thermal exposure. After this simulation, fracture load measurements were performed in a universal testing machine (Zwick 1445, ZwickRoell, Ulm, Germany). The embedded tooth was fixed into the holding device of the machine, and a tin foil (thickness 0.5 mm; DENTAURUM, Ispringen, Germany, Lot-No: 469721) was placed between the stamp and the tooth to ensure a homogenous force distribution and to avoid local force peaks (Fig. 1f). Then, an increasing load was applied perpendicularly to the central fossa with a stamp of hemispherical shape (diameter 6 mm) until failure occurred (crosshead speed 1 mm/min). Force values were recorded automatically in Newton (N) as soon as the maximum fracture load decreased by 50% until an initial crack or total fracture was detected (testXpert II V3.6, ZwickRoell). The fracture types were classified as follows: tooth fracture (a), cusp fracture (b), and restoration fracture (c) (Table 5).
All measured data were analyzed with the SPSS statistic program (version 25.0.0.1, IBM, Armonk, NY, USA). The assumption of normality was tested using Kolmogorov-Smirnov test. Two-way ANOVA with partial eta squared (ηp2) followed by Scheffé post hoc test was computed to verify the impact of chewing simulation on fracture load. Weibull distribution parameter (Weibull modulus m) was calculated using the maximum likelihood estimation method and 95% confidence interval (95% CI) [17]. Chi square (chi2) test and Ciba-Geigy tables were used to analyze the relative frequencies of fracture types together with the corresponding 95% confidence intervals (CI) [18]. In all analyses, the level of significance was set to p < 0.05.
Results
The descriptive statistics is shown in Table 3. The Kolmogorov-Smirnov test indicated no violation of normal distribution, so data were analyzed parametrically. According to two-way ANOVA, the restoration material showed an influence on the fracture load (p < 0.001), whereas chewing simulation had no impact (p = 0.132) (Table 4).
ESS and TET showed the significant lowest fracture load down to a minimum of 956 N (Fig. 3). VIC was together with VES, KET, and JUV in the same value range. The sound molars presented the highest fracture load values of up to 2981 N (p < 0.001).
The microscopic examinations showed that the chewing simulation combined with thermal cycling did not cause any fractures in all investigated teeth.
Regarding Weibull modulus, KET had a significantly lower value than JUV for the groups with performed chewing simulation, whereas TET showed for the groups without chewing simulation the significant highest Weibull modulus (Table 3).
With respect to fracture types, differences between the groups were observed (chi2 test p < 0.001). All indirect restorations and sound molars, regardless of the fatigue process, showed a significantly higher tooth fracture rate (75–100%) than TET (Table 5). All 3D printed inlays remained intact after the fracture load test (100%). Only one milled inlay out of JUV failed due to a restoration fracture (12.5%). TET showed a significantly higher restoration fracture rate than all the other groups (87.5%). With regard to cusp fractures, the untreated molars presented the significantly highest relative frequencies (50%).
Discussion
This study investigated the fracture load of 3D printed indirect PEEK inlays in comparison with milled ones, conventionally direct composite fillings, and sound human molars under the influence of chewing simulation with combined thermal cycling. In general, all tested indirect and direct restorations demonstrated a higher fracture load compared with the expected physiological chewing forces of 110–125 N [19, 20] and maximum bite forces in the molar region of up to 909 N [21, 22]. However, the first null hypothesis had to be rejected, since the various materials indicated differences in fracture load. ESS and TET showed the lowest fracture load of all tested groups. Although ESS was processed like all the other filaments as well as the inlays were inserted according to the same procedure, the low fracture load might be explained by the material composition, like lower filler degree or different filler types for example. Unfortunately, this is difficult to state due to a lack of information by the manufacturer. It might also be possible that each filament needs individual printing parameters to achieve better mechanics. Since the printed components have an anisotropic behavior, the printing direction and thus the position of the support structure can decisively influence the mechanical properties. In the present study, the support structure was attached to the occlusal surface of the inlay, whereby the printing direction was parallel to the direction of measurement of the fracture load, which is supposed to lead to optimal mechanics [23].
TET also had the lowest fracture load, because direct composite fillings placed in a cavity in several layers often exhibit a degree of inhomogeneity in form of small voids, insufficiently polymerized parts, and polymerization shrinkage stress, resulting in lower mechanics [24]. Also, because of a higher polymer content than the semi-crystalline PEEK materials, the water absorption is higher. This might explain that the resin composite reacted sensitively to the water storage and chewing simulation with thermal cycling [25].
The sound molars presented by far the highest fracture load. Unfortunately, cavity preparations usually lead to an extended loss of enamel and dentin. As a consequence, the tooth loses considerable stability and becomes more vulnerable to fractures. Mondelli et al. have found out that a class I cavity reduces the strength of the tooth less than a class II preparation with equal width, so marginal ridges provide a tooth stability [26]. The buccolingual width is also an influential factor on flexural strength. In the present investigation, the width was maximum one-third of the intercuspal distance. However, even with this narrow occlusal cavity, the tooth is already weakened compared with an uncavitated tooth [12]. The etiology of a tooth fracture is complex and multifactorial. While intact teeth therefore rarely fracture under chewing load, teeth weakened by preparation of cavities, caries, endodontic treatments, genetic disorders like amelo-/dentinogenesis imperfecta or molar-incisor hypomineralization (MIH) and periodontal lesions may spontaneously fracture under physiological mastication load, so that far lower forces are sufficient for failure of the tooth to occur [27]. Consequently, a major restoration or a root canal therapy is indicated or even in the worst case, the affected tooth must be extracted. Also, occlusal overloading due to bruxism, accidental trauma, adverse cusp-fossa relationship, inadequate restoration planning, manufacturing defects, or material fatigue can cause a fracture [28].
To be able to predict and prevent material failure, Weibull statistics is a convenient tool in dentistry for comparing the flaw size distribution as well as flexural strength of different specimen sizes, stress configurations, and testing conditions [14]. The Weibull modulus m indicates the spread of the distribution, so the higher the value, the smaller the dispersion and better the structural reliability of the material. In this study, for the groups with performed chewing simulation, the 3D printed material KET showed the lowest Weibull modulus, whereas the milled material JUV had the highest one. This could be explained by a manufacturing process of JUV under controlled industrial conditions that provides a homogeneous structure and high reliability. It is unclear why KET presented such a low Weibull modulus and thus the lowest reliability and fatigue resistance. This might be explained by a high water absorption during water storage in the incubator or chewing simulator. Unfortunately, again, data about the water absorption capacity, for example, by the manufacturer is missing.
TET showed the highest m value for the groups without chewing simulation, which is remarkable, as it is a direct filling material, which, due to the incremental application, always shows minimal inhomogeneities, and therefore, a low m value could be expected. Apparently, it was processed homogeneously in this investigation.
In terms of fracture types, all indirect restorations as well as sound molars showed tooth fractures, indicating a strong coherent connection within the restoration material respectively hard tooth tissue. The single layers of the 3D printed inlays seemed to be solidly fused due to the high melting temperatures. The high forces applied during the test were instantly transmitted to the tooth, resulting in a fracture. As PEEK has a lower Young’s modulus than dentin (13 GPa, [29]) and enamel (72.7–87.5 GPa, [30]), tensile stress is concentrated and transmitted to the tooth under axial compressive stress, which leads to fracture [31]. Although TET also has a lower Young’s modulus than the tooth structure, the fillings fractured during the measurements. One explanation might be that a fracture can spread more easily between the single polymerized parts due to unavoidable minimal inhomogeneities [32].
The teeth of this study fractured completely as well as cusp fractures occurred, which is rather explained by the irregular anatomical shapes of the used molars. Each natural tooth is individual with regard to the configuration of the occlusal surface, the size of the cusps, level of calcification, and location of the pulp chamber, which all have a decisive influence on the fracture type and fracture load, also represented by a high standard deviation in this investigation. Sheen et al. observed a higher fracture load for teeth of young men and no significant differences between mandibular and maxillary teeth [33]. In future studies, teeth of almost the same size, gender, and age range should be selected for enhanced comparability.
As the results presented, there were no major differences in fracture load values between printed and milled inlays. However, the printed inlays required an intensive postprocessing care. After removing the support structures, the final occlusal surface differed from the designed one and had to be re-contoured. The basal surface and the sides of the inlay had to be adapted in quite an intensive manner for being able to insert it into the cavity. As a result, a quite large cement gap was mostly created, which is susceptible to microleakage in vivo [34]. On the other hand, it was found that the fracture load is not affected by the thickness of the cement gap and internal fit, only by the quality of the margin [35]. Apart from the good mechanical properties, the poor esthetics of the PEEK inlays has to be criticized with regard to a brownish-gray color. In order to achieve a tooth-colored translucent appearance, veneering is necessary, whereas a digital veneering method presented the highest fracture load [36].
The fact that the fracture load values exceeded the chewing forces can also be explained by the materials used for adhesive luting in this study. Thus airborne particle abrasion increases the surface area, which enables better penetration of the adhesive and ensures a solid micro-retentive bonding [37]. Due to the fact that visio.link is MMA (methyl methacrylate)-based and contains PETIA (pentaerythritol triacrylate), it has superior properties compared with other adhesive systems for PEEK [38]. The application of Syntac with Variolink is also a proven combination for adhesive luting of indirect restorations, which have achieved excellent results [39].
Fatigue resistance of dental materials is a very important factor when selecting a suitable material for a restoration, which was examined in the present study by chewing simulation. In order to increase the clinical relevance, chewing simulation with combined thermal cycling was used as an aging process in order to carry out a simultaneous mechanical and thermal stress test of the restored teeth. The 1.2 million chewing cycles applied correspond to 5 years of clinical practice and offer sufficient clinical relevance with regard to the survival rate of dental restorations [16]. Surprisingly, this fatigue process had no impact on the fracture load of the tested molars, so all materials revealed sufficient chewing resistance and the second null hypothesis had to be accepted. However, the teeth were only loaded with 50 N during the simulation, whereby physiologically higher chewing forces should rather be used. To develop a chewing simulator with a stable function using such high weights is quite a challenge. Teeth are constantly in contact with salvia in the oral environment, which was not practiced in this study. Storage and chewing simulation with physiological saliva could have yielded even better values [40].
Compared with other indirect materials, inlays out of yttrium-stabilized zirconia ceramic showed comparable fracture resistance to intact teeth of up to 1646 N due to the high compressive strength and transformation toughening of this ceramic [41]. Inlays made out of resin composite and lithium disilicate glass ceramic revealed lower values than intact teeth, whereas composite ones had the lowest fracture strength due to a minor Young’s modulus of elasticity and rigidity [31].
The present investigation demonstrated the first steps towards AM of dental restorations out of PEEK via FLM and has shown promising results regarding mechanics and chewing resistance. Therefore, a huge potential in future applications can be expected. However, technical improvements on the printer side with regard to accuracy, detailed information about the filament composition to explain and predict the mechanical behavior, and in vivo clinical studies are mandatory.
Conclusion
Within the limitations of this investigation, the following conclusions can be made:
-
All 3D printed and milled indirect PEEK inlays as well as the direct resin composite fillings showed a higher fracture load than the expected physiological and maximum chewing forces in the molar region, whereas sound molars demonstrated the highest fracture load of up to 2981 N.
-
Chewing simulation with combined thermal cycling had no impact on the fracture load of the tested specimens.
-
A quite extensive post-processing had to be executed especially for the printed inlays.
-
All 3D printed PEEK indirect inlays stayed intact after the fracture load test.
References
Dawood A, Marti Marti B, Sauret-Jackson V, Darwood A (2015) 3D printing in dentistry. Br Dent J:521-529. https://doi.org/10.1038/sj.bdj.2015.914
Reymus M, Fotiadou C, Kessler A, Heck K, Hickel R, Diegritz C (2019) 3D printed replicas for endodontic education. Int Endod J 1:123–130. https://doi.org/10.1111/iej.12964
Javaid M, Haleem A (2019) Current status and applications of additive manufacturing in dentistry: a literature-based review. J Oral Biol Craniofac Res 3:179–185. https://doi.org/10.1016/j.jobcr.2019.04.004
Ngo TD, Kashani A, Imbalzano G, Nguyen KTQ, Hui D (2018) Additive manufacturing (3D printing): a review of materials, methods, applications and challenges. Compos B Eng:172–196. https://doi.org/10.1016/j.compositesb.2018.02.012
van Noort R (2012) The future of dental devices is digital. Dent Mater 1:3–12. https://doi.org/10.1016/j.dental.2011.10.014
Valentan B, Kadivnik Z, Brajlih T, Anderson A, Igor D (2013) Processing poly (ether etherketone) on a 3d printer for thermoplastic modelling. Mater Tehnol 6:715–721
Kurtz SM, Devine JN (2007) PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 32:4845–4869. https://doi.org/10.1016/j.biomaterials.2007.07.013
Haleem A, Javaid M (2019) Polyether ether ketone (PEEK) and its manufacturing of customised 3D printed dentistry parts using additive manufacturing. Clin Epidemiol Glob Health. https://doi.org/10.1016/j.cegh.2019.03.001
Bathala L, Majeti V, Rachuri N, Singh N, Gedela S (2019) The role of polyether ether ketone (Peek) in dentistry-a review. J Med Life 1:5–9. https://doi.org/10.25122/jml-2019-0003
Vaezi M, Yang S (2015) Extrusion-based additive manufacturing of PEEK for biomedical applications. Virtual and Physical Prototyping 3:123–135. https://doi.org/10.1080/17452759.2015.1097053
Mondelli J, Sene F, Ramos RP, Benetti AR (2007) Tooth structure and fracture strength of cavities. Braz Dent J 2:134–138
Larson TD, Douglas WH, Geistfeld RE (1981) Effect of prepared cavities on the strength of teeth. Oper Dent 1:2–5
Coelho-de-Souza FH, Camacho GB, Demarco FF, Powers JM (2008) Fracture resistance and gap formation of MOD restorations: influence of restorative technique, bevel preparation and water storage. Oper Dent 1:37–43. https://doi.org/10.2341/07-27
Quinn JB, Quinn GD (2010) A practical and systematic review of Weibull statistics for reporting strengths of dental materials. Dent Mater 2:135–147. https://doi.org/10.1016/j.dental.2009.09.006
Weibull W (1951) A statistical distribution function of wide applicability. J Appl Mech 3:293–297
Rosentritt M, Behr M, van der Zel JM, Feilzer AJ (2009) Approach for valuating the influence of laboratory simulation. Dent Mater 3:348–352. https://doi.org/10.1016/j.dental.2008.08.009
Bütikofer L, Stawarczyk B, Roos M (2015) Two regression methods for estimation of a two-parameter Weibull distribution for reliability of dental materials. Dent Mater 2:e33–e50. https://doi.org/10.1016/j.dental.2014.11.014
Geigy WT, Statistik T (1980) vol 8. CIBA-GEIGY Limited, Basel
Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, Van THMA, Witter DJ, Kalk W, Jansen JA (2000) Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res 7:1519–1524. https://doi.org/10.1177/00220345000790071501
Helkimo E, Carlsson G, Helkimo M (1977) Bite force and state dentition. Acta Odontol Scand 6:297–303. https://doi.org/10.3109/00016357709064128
Waltimo A, Könönen M (1995) Maximal bite force and its association with signs and symptoms of craniomandibular disorders in young Finnish non-patients. Acta Odontol Scand 4:254–258. https://doi.org/10.3109/00016359509005982
Ahlberg JP, Kovero OA, Hurmerinta KA, Zepa I, Nissinen MJ, Könönen MH (2003) Maximal bite force and its association with signs and symptoms of TMD, occlusion, and body mass index in a cohort of young adults. Cranio 4:248–252. https://doi.org/10.1080/08869634.2003.11746258
Rinaldi M, Ghidini T, Cecchini F, Brandao A, Nanni F (2018) Additive layer manufacturing of poly (ether ether ketone) via FDM. Compos B Eng:162–172. https://doi.org/10.1016/j.compositesb.2018.03.029
Aggarwal V, Logani A, Jain V, Shah N (2008) Effect of cyclic loading on marginal adaptation and bond strength in direct vs. indirect class II MO composite restorations. Oper Dent 5:587–592. https://doi.org/10.2341/07-152
Liebermann A, Wimmer T, Schmidlin PR, Scherer H, Loffler P, Roos M, Stawarczyk B (2016) Physicomechanical characterization of polyetheretherketone and current esthetic dental CAD/CAM polymers after aging in different storage media. J Prosthet Dent 3:321-328.e2. https://doi.org/10.1016/j.prosdent.2015.09.004
Mondelli J, Steagall L, Ishikiriama A, de Lima Navarro MF, Soares FB (1980) Fracture strength of human teeth with cavity preparations. J Prosthet Dent 4:419–422. https://doi.org/10.1016/0022-3913(80)90213-9
Reeh ES, Messer HH, Douglas WH (1989) Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod 11:512–516. https://doi.org/10.1016/S0099-2399(89)80191-8
Lubisich EB, Hilton TJ, Ferracane J (2010) Cracked teeth: a review of the literature. J Esthet Restor Dent 3:158–167. https://doi.org/10.1111/j.1708-8240.2010.00330.x
Watts DC (1994) Elastic moduli and visco-elastic relaxation. J Dent 3:154–158
Habelitz S, Marshall SJ, Marshall GW, Balooch M (2001) Mechanical properties of human dental enamel on the nanometre scale. Arch Oral Biol 2:173–183. https://doi.org/10.1016/S0003-9969(00)00089-3
Costa AKF, Xavier TA, Noritomi PY, Saavedra G, Borges ALS (2014) The influence of elastic modulus of inlay materials on stress distribution and fracture of premolars. Oper Dent 4:E160–E170. https://doi.org/10.2341/13-092-l
Melo RA, Bispo AdSL, Barbosa GAS, Galvão MR, de Assunção IV, Souza ROdA, Borges BCD (2019) Morphochemical characterization, microhardness, water sorption, and solubility of regular viscosity bulk fill and traditional composite resins. Microsc Res Tech 9:1500–1506. https://doi.org/10.1002/jemt.23315
Sheen C-Y, Dong J-K, Brantley WA, Han DS (2019) A study of fracture loads and fracture characteristics of teeth. J Adv Prosthodont 3:187–192. https://doi.org/10.4047/jap.2019.11.3.187
Shetty M, Rajalakshmi S, Krishna Prasad D (2014) Comparison of marginal gap and microleakage in copy-milled and cad-milled zirconia copings bonded using light cure and chemical cure resin bonding systems. J Indian Prosthodont Soc 1:37–45. https://doi.org/10.1007/s13191-014-0359-x
Okutan M, Heydecke G, Butz F, Strub JR (2006) Fracture load and marginal fit of shrinkage-free ZrSiO4 all-ceramic crowns after chewing simulation. J Oral Rehabil 11:827–832. https://doi.org/10.1111/j.1365-2842.2006.01637.x
Taufall S, Eichberger M, Schmidlin PR, Stawarczyk B (2016) Fracture load and failure types of different veneered polyetheretherketone fixed dental prostheses. Clin Oral Investig 9:2493–2500. https://doi.org/10.1007/s00784-016-1777-4
Uhrenbacher J, Schmidlin PR, Keul C, Eichberger M, Roos M, Gernet W, Stawarczyk B (2014) The effect of surface modification on the retention strength of polyetheretherketone crowns adhesively bonded to dentin abutments. J Prosthet Dent 6:1489–1497. https://doi.org/10.1016/j.prosdent.2014.05.010
Stawarczyk B, Taufall S, Roos M, Schmidlin PR, Lümkemann N (2018) Bonding of composite resins to PEEK: the influence of adhesive systems and air-abrasion parameters. Clin Oral Investig 2:763–771. https://doi.org/10.1007/s00784-017-2151-x
Frankenberger R, Krämer N, Appelt A, Lohbauer U, Naumann M, Roggendorf MJ (2011) Chairside vs. labside ceramic inlays: effect of temporary restoration and adhesive luting on enamel cracks and marginal integrity. Dent Mater 9:892–898. https://doi.org/10.1016/j.dental.2011.05.007
Liebermann A, Ilie N, Roos M, Stawarczyk B (2017) Effect of storage medium and aging duration on mechanical properties of self-adhesive resin-based cements. J Appl Biomater Funct Mater 3:e206–e214. https://doi.org/10.5301/jabfm.5000362
Wafaie RA, Ibrahim Ali A, Mahmoud SH (2018) Fracture resistance of prepared premolars restored with bonded new lab composite and all-ceramic inlay/onlay restorations: laboratory study. J Esthet Restor Dent 3:229–239. https://doi.org/10.1111/jerd.12364
Acknowledgments
The authors would like to acknowledge KUMOVIS for providing the 3D printer HTRD1.2 and the PEEK filaments. We are also grateful to Ivoclar Vivadent and Gebr. Brasseler for material support of this study.
Funding
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Prechtel, A., Stawarczyk, B., Hickel, R. et al. Fracture load of 3D printed PEEK inlays compared with milled ones, direct resin composite fillings, and sound teeth. Clin Oral Invest 24, 3457–3466 (2020). https://doi.org/10.1007/s00784-020-03216-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03216-5