Abstract
Objective
The role of tumour thickness (TT), depth of invasion (DOI) from two different reference points (TT2 and TT3), perineural invasion (PNI) and lymphovascular invasion (LVI) were evaluated to predict lymph node metastasis (LNM) in oral squamous cell carcinoma (OSCC). Reference points for measuring the DOI were suggested.
Material and methods
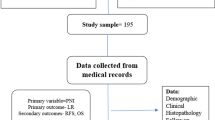
Paraffin-embedded tissues of excisional biopsy cases diagnosed as OSCC were sectioned and stained in haematoxylin and eosin to study variables like TT1, TT2, TT3, PNI and LVI. Out of total 150 cases collected for the study, 136, 123 and 149 cases were qualified for analysis of TT1, TT2 and TT3 respectively. The association with LNM was studied using chi square test of independence. A binary logistic regression model (BLC) was developed to indicate high-risk cases.
Results
Receiver operating curve analysis suggested an optimum cut-off value. A significant correlation of TT1 (> 8.64, RR = 1.642, p = 0.018) and TT2 (> 7.64, RR = 2.041, p = 0.016), PNI (p = 0.028) and LVI (p = 0.000) were found with LNM. A mathematical model was suggested as Z = − 1.866 + 0.101TT2 + 2.106VI + e, where Z = log [(p/(1 − p)] p = probability of the case experiencing the event of interest.
Conclusion
With the suggestion of a standardised reference point to measure DOI for the first time, this study has shown an association of TT1, TT2, PNI and LVI with LNM in Indian Population. The mathematical model can help in identifying high-risk cases in OSCC.
Clinical relevance
Such studies would offer avenues for the pre-surgery assessment of depth of invasion and tumour thickness before performing neck dissection, thereby decreasing morbidity.


Similar content being viewed by others
References
Bonifazi M, Malvezzi M, Bertuccio P, Edefonti V, Garavello W, Levi F, la Vecchia C, Negri E (2011) Age-period-cohort analysis of oral cancer mortality in Europe: the end of an epidemic? Oral Oncol 47(5):400–407
Byakodi R, Byakodi S, Hiremath S, Byakodi J, Adaki S, Marathe K, Mahind P (2012) Oral cancer in India: an epidemiologic and clinical review. J Community Health 37(2):316–319
Makitie AA, Koivunen P, Keski-Santti H, Tornwall J, Pukkila M, Laranne J et al (2007) Oral tongue carcinoma and its treatment in Finland. Eur Arch Otorhinolaryngol 264:263–267
Teichgraeber JF, Clairmont AA (1984) The incidence of occult metastases for cancer of the oral tongue and floor of the mouth: treatment rationale. Head Neck Surg 7:15–21
Ross GL, Soutar DS, MacDonald DG, Shoaib T, Camilleri IG, Robertson AG (2004) Improved staging of cervical metastases in clinically node-negative patients with head and neck squamous cell carcinoma. Ann Surg Oncol 11:213–218
Huang SF, Kang CJ, Lin CY, Fan KH, Yen TC, Wang HM et al (2008) Neck treatment of patients with early stage oral tongue cancer: comparison between observation, supraomohyoid dissection, and extended dissection. Cancer 1(112):1066–1075
Kelner N, Vartanian JG, Pinto CA, Coutinho-Camillo CM, Kowalski LP (2014) Does elective neck dissection in T1/T2 carcinoma of the oral tongue and floor of the mouth influence recurrence and survival rates? Br J Oral Maxillofac Surg 52:590–597
Thomas B, Stedman M, Davies L (2014) Grade as a prognostic factor in oral squamous cell carcinoma: a population-based analysis of the data. Laryngoscope 124:688–694
Ganly I, Patel S, Shah J (2012) Early stage squamous cell cancer of the oral tongue--clinicopathologic features affecting outcome. Cancer 1(118):101–111
El-Fol HA, Noman SA, Beheiri MG, Khalil AM, Kamel MM (2015) Significance of post-resection tissue shrinkage on surgical margins of oral squamous cell carcinoma. J Craniomaxillofac Surg 43:475–482
Mistry RC, Qureshi SS, Kumaran C (2005) Post-resection mucosal margin shrinkage in oral cancer: quantification and significance. J Surg Oncol 1(91):131–133
Shen WR, Wang YP, Chang JY, Yu SY, Chen HM, Chiang CP (2014) Perineural invasion and expression of nerve growth factor can predict the progression and prognosis of oral tongue squamous cell carcinoma. J Oral Pathol Med 43:258–264
Tai SK, Li WY, Yang MH, Chu PY, Wang YF (2013a) Perineural invasion in T1 oral squamous cell carcinoma indicates the need for aggressive elective neck dissection. Am J Surg Pathol 37:1164–1172
Jardim JF, Francisco AL, Gondak R, Damascena A, Kowalski LP (2015) Prognostic impact of perineural invasion and lymphovascular invasion in advanced stage oral squamous cell carcinoma. Int J Oral Maxillofac Surg 44:23–28
Michikawa C, Uzawa N, Kayamori K, Sonoda I, Ohyama Y, Okada N, Yamaguchi A, Amagasa T (2012) Clinical significance of lymphatic and blood vessel invasion in oral tongue squamous cell carcinomas. Oral Oncol 48:320–324
Chandler K, Vance C, Budnick S, Muller S (2011) Muscle invasion in oral tongue squamous cell carcinoma as a predictor of nodal status and local recurrence: just as effective as DOI? Head Neck Pathol 5:359–363
Aita G, da Costa WH, de Cassio Zequi S, da Cunha IW, Soares F, Guimaraes GC et al (2015) Pattern of invasion is the most important prognostic factor in patients with penile cancer submitted to lymph node dissection and pathological absence of lymph node metastasis. BJU Int 16:584–589
Karamitopoulou E (2012) Tumor budding cells, cancer stem cells and epithelial-mesenchymal transition-type cells in pancreatic cancer. Front Oncol 2:209
van Wyk HC, Park J, Roxburgh C, Horgan P, Foulis A, McMillan DC (2015) The role of tumour budding in predicting survival in patients with primary operable colorectal cancer: a systematic review. Cancer Treat Rev 41:151–159
Huang SH, Hwang D, Lockwood G, Goldstein DP, O’Sullivan B (2009) Predictive value of tumor thickness for cervical lymph-node involvement in squamous cell carcinoma of the oral cavity: a meta-analysis of reported studies. Cancer 1(115):1489–1497
O’Brien CJ, Lauer CS, Fredricks S, Clifford AR, McNeil EB, Bagia JS et al (2003) Tumor thickness influences prognosis of T1 and T2 oral cavity cancer--but what thickness. Head Neck 25:937–945
Asakage T, Yokose T, Mukai K, Tsugane S, Tsubono Y, Asai M et al (1998) Tumor thickness predicts cervical metastasis in patients with stage I/II carcinoma of the tongue. Cancer 15(82):1443–1448
Ebrahimi A, Gil Z, Amit M, Yen TC, Liao CT, Chaturvedi P et al (2014) Primary tumor staging for oral cancer and a proposed modification incorporating DOI: an international multicenter retrospective study. JAMA Otolaryngol Head Neck Surg 140(12):1138–1148
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK et al (2017) The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67:93–99
Fukano H, Matsuura H, Hasegawa Y, Nakamura S (1997) DOI as a predictive factor for cervical lymph node metastasis in tongue carcinoma. Head Neck 19:205–210
Sparano A, Weinstein G, Chalian A, Yodul M, Weber R (2004) Multivariate predictors of occult neck metastasis in early oral tongue cancer. Otolaryngol Head Neck Surg 131:472–476
Lim SC, Zhang S, Ishii G, Endoh Y, Kodama K, Miyamoto S et al (2004) Predictive markers for late cervical metastasis in stage I and II invasive squamous cell carcinoma of the oral tongue. Clin Cancer Res 1(10):166–172
Ambrosch P, Kron M, Fischer G, Brinck U (1995) Micrometastases in carcinoma of the upper aerodigestive tract: detection, risk of metastasizing, and prognostic value of DOI. Head Neck 17:473–479
Giacomarra V, Tirelli G, Papanikolla L, Bussani R (1999) Predictive factors of nodal metastases in oral cavity and oropharynx carcinomas. Laryngoscope 109:795–799
Gonzalez-Moles MA, Esteban F, Rodriguez-Archilla A, Ruiz-Avila I, Gonzalez-Moles S (2002) Importance of TT measurement in prognosis of tongue cancer. Oral Oncol 38:394–397
Morton RP, Ferguson CM, Lambie NK, Whitlock RM (1994) Tumor thickness in early tongue cancer. Arch Otolaryngol Head Neck Surg 120:717–720
Arora A, Husain N, Bansal A, Neyaz A, Jaiswal R, Jain K (2017) Development of a new outcome prediction model in early-stage squamous cell carcinoma of the oral cavity based on histopathologic parameters with multivariate analysis: the ADITI-nuzhat lymph-node prediction score (ANLPS) system. Am J Surg Pathol 41:950–960
Brockhoff HC, Kim RY, Braun TM et al (2017) Correlating the DOI at specific anatomic locations with the risk for regional metastatic disease to lymph nodes in the neck for oral squamous cell carcinoma. Head Neck 39:974–979
Haksever M, Inancli HM, Tuncel U, Kurkcuoglu SS, Uyar M, Genc O et al (2012) The effects of tumor size, degree of differentiation, and DOI on the risk of neck node metastasis in squamous cell carcinoma of the oral cavity. Ear Nose Throat J 91:130–135
Kane SV, Gupta M, Kakade AC, D’Cruz A (2006) DOI is the most significant histological predictor of subclinical cervical lymph node metastasis in early squamous carcinomas of the oral cavity. Eur J Surg Oncol 32:795–803
Melchers LJ, Schuuring E, van Dijk BA, de Bock GH, Witjes MJ, van der Laan BF et al (2012) Tumour infiltration depth ≥4 mm is an indication for an elective neck dissection in pT1cN0 oral squamous cell carcinoma. Oral Oncol 48:337–342
Suresh TN, Hemalatha A, Harendra Kumar ML, Azeem Mohiyuddin SM (2015) Evaluation of histomorphological and immunohistochemical parameters as biomarkers of cervical lymph node metastasis in squamous cell carcinoma of oral cavity: a retrospective study. J Oral Maxillofac Pathol 19:18–24
Shingaki S, Suzuki I, Nakajima T, Kawasaki T (1988) Evaluation of histopathologic parameters in predicting cervical lymph node metastasis of oral and oropharyngeal carcinomas. Oral Surg Oral Med Oral Pathol 66:683–688
Wilkinson EJ (1985) Superficial invasive carcinoma of the vulva. Clin Obstet Gynecol 28:188–195
Moore C, Kuhns JG, Greenberg RA (1986) Thickness as prognostic aid in upper aerodigestive tract cancer. Arch Surg 121:1410–1414
van den Einden LC, Massuger LF, Jonkman JK, Bult P, de Hullu JA, Bulten J (2015) An alternative way to measure the DOI of vulvar squamous cell carcinoma in relation to prognosis. Mod Pathol 28:295–302
Tai SK, Li WY, Yang MH, Chu PY, Wang YF, Chang PM (2013b) Perineural invasion as a major determinant for the aggressiveness associated with increased tumor thickness in t1-2 oral tongue and buccal squamous cell carcinoma. Ann Surg Oncol 20:3568–3674
Tai SK, Li WY, Yang MH, Chang SY, Chu PY, Tsai TL, Wang YF, Chang PMH (2012) Treatment for T1-2 oral squamous cell carcinoma with or without perineural invasion: neck dissection and postoperative adjuvant therapy. Ann Surg Oncol 19:1995–2002
Steinhart H, Kleinsasser O (1993) Growth and spread of squamous cell carcinoma of the floor of the mouth. Eur Arch Otorhinolaryngol 250:358–361
Varsha BK, Radhika MB, Makarla S, Kuriakose MA, Kiran GS, Padmalatha GV (2015) Perineural invasion in oral squamous cell carcinoma: case series and review of literature. J Oral Maxillofac Pathol 19:335–341
Bundgaard T, Bentzen SM, Wildt J, Sorensen FB, Sogaard H, Nielsen JE (1996) Histopathologic, stereologic, epidemiologic, and clinical parameters in the prognostic evaluation of squamous cell carcinoma of the oral cavity. Head Neck 18:142–152
Karas DE, Baredes S, Chen TS, Karas SF (1995) Relationship of biopsy and final specimens in evaluation of tumor thickness in floor of mouth carcinoma. Laryngoscope 105:491–493
de Visscher JG, Schaapveld M, Grond AJ, van der Waal I (1999) Relationship of tumor thickness in punch biopsy and subsequent surgical specimens in stage I squamous cell carcinoma of the lower lip. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88:141–144
McLaughlin RB Jr, Montone KT, Wall SJ, Chalian AA, Weinstein GS, Roberts SA et al (1999) Nerve cell adhesion molecule expression in squamous cell carcinoma of the head and neck: a predictor of propensity toward perineural spread. Laryngoscope. 109(5):821–826
Maruya SI, Myers JN, Weber RS, Rosenthal DI, Lotan R, El-Naggar AK (2005) ICAM-5 (telencephalin) gene expression in head and neck squamous carcinoma tumorigenesis and perineural invasion. Oral Oncol 41(6):580–588
Lourenco SV, Coutinho-Camillo CM, Buim ME, Pereira CM, Carvalho AL, Kowalski LP et al (2010) Oral squamous cell carcinoma: status of tight junction claudins in the different histopathological patterns and relationship with clinical parameters. A tissue-microarray-based study of 136 cases. J Clin Pathol 63(7):609–614
Anderson TD, Feldman M, Weber RS, Ziober AF, Ziober BL (2001) Tumor deposition of laminin-5 and the relationship with perineural invasion. Laryngoscope. 111(12):2140–2143
Suzuki M, Suzuki T, Asai M, Ichimura K, Nibu K, Sugasawa M et al (2007) Clinicopathological factors related to cervical lymph node metastasis in a patient with carcinoma of the oral floor. Acta Otolaryngol Suppl 12:129–135
Chen YW, Yu EH, Wu TH, Lo WL, Li WY, Kao SY (2008) Histopathological factors affecting nodal metastasis in tongue cancer: analysis of 94 patients in Taiwan. Int J Oral Maxillofac Surg 37:912–926
Fagan JJ, Collins B, Barnes L, D’Amico F, Myers EN, Johnson JT (1998) Perineural invasion in squamous cell carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg 124:637–640
Wallwork BD, Anderson SR, Coman WB (2007) Squamous cell carcinoma of the floor of the mouth: TT and the rate of cervical metastasis. ANZ J Surg 77:761–764
Gil Z, Carlson DL, Gupta A, Lee N, Hoppe B, Shah JP, Kraus DH (2009) Patterns and incidence of neural invasion in patients with cancers of the paranasal sinuses. Arch Otolaryngol Head Neck Surg 135:173–179
Close LG, Burns DK, Reisch J, Schaefer SD (1987) Microvascular invasion in cancer of the oral cavity and oropharynx. Arch Otolaryngol Head Neck Surg 113:1191–1195
Woolgar JA, Scott J (1995) Prediction of cervical lymph node metastasis in squamous cell carcinoma of the tongue/floor of mouth. Head Neck 17:463–472
Shieh YS, Lee HS, Shiah SG, Chu YW, Wu CW, Chang LC (2004) Role of angiogenic and non-angiogenic mechanisms in oral squamous cell carcinoma: correlation with histologic differentiation and tumor progression. J Oral Pathol Med 33:601–606
Shintani S, Li C, Ishikawa T, Mihara M, Nakashiro K, Hamakawa H (2004) Expression of vascular endothelial growth factor A, B, C, and D in oral squamous cell carcinoma. Oral Oncol 40:13–20
Martinez-Gimeno C, Rodriguez EM, Vila CN, Varela CL (1995) Squamous cell carcinoma of the oral cavity: a clinicopathologic scoring system for evaluating risk of cervical lymph node metastasis. Laryngoscope 105:728–733
Goldson TM, Han Y, Knight KB, Weiss HL, Resto VA (2010) Clinicopathological predictors of lymphatic metastasis in HNSCC: implications for molecular mechanisms of metastatic disease. J Exp Ther Oncol 8:211–221
Seki S, Fujiwara M, Matsuura M, Fujita S, Ikeda H, Asahina I, Ikeda T (2011) Prediction of outcome of patients with oral squamous cell carcinoma using vascular invasion and the strongly positive expression of vascular endothelial growth factors. Oral Oncol 47:588–593
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was conducted after the approval of the Institutional Ethical Committee, Siksha ‘O’ Anusandhan Deemed to be University (Ref No./DMR/IMS-SH/SOA/16054.dtd:22 JULY 2016). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee.
Informed consent
For this type of study, formal consent was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sahoo, A., Panda, S., Mohanty, N. et al. Perinerural, lymphovascular and depths of invasion in extrapolating nodal metastasis in oral cancer. Clin Oral Invest 24, 747–755 (2020). https://doi.org/10.1007/s00784-019-02921-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02921-0