Abstract
Objective
The aim of this in vitro study was to evaluate the mechanical behavior and bacterial microleakage at the implant/abutment-tapered interface following mechanical cycling.
Materials and methods
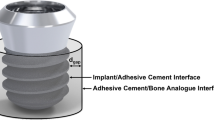
Two groups of screwless (Morse taper) implants (G1 and G2) and two groups of prosthetic screwed implants (G3 and G4) were tested. One group from each model (G2 and G4) were submitted to mechanical cycling, 500,000 cycles per sample, at a load of 120 N at 2 Hz prior to analysis. Microbiological analysis was performed via immersion of all samples in an Escherichia coli-containing suspension, incubated at 37 °C. After 14 days, the abutments were removed from their respective implants, registering the removal force (G1 and G2) or reverse torque (G3 and G4), and the presence of bacterial leakage was evaluated. Scanning electron microscopy (SEM) was performed to analyze the tapered surfaces of the selected samples. The Student t, binomial, and G tests were used for statistical analysis at a 5 % significance level.
Results
The results showed no significant difference between removal force, reverse torque, and contamination values when comparing implants of the same type. However, when the four groups were compared, contamination differed significantly (p = 0.044), with G1 having the least number of contaminated samples (8.3 %). SEM analysis showed superficial defects and damage.
Conclusions
The abutment removal force or torque was not affected by mechanical cycling. Bacterial sealing of the implant/abutment tapered interface was not effective for any condition analyzed. Imprecise machining of implant parts does not allow a sufficient contact area between surfaces to provide effective sealing and prevent bacterial leakage.
Clinical relevance
The microscopic gap caused by unsatisfactory implant/abutment adaptation, surface irregularities, and plastic deformation of all parts enabled bacterial contamination of the oral implants.






Similar content being viewed by others
References
Nascimento C, Miani PK, Pedrazzi V, et al. (2012) Leakage of saliva through the implant-abutment interface: in vitro evaluation of three different implant connections under unloaded and loaded conditions. Int J Oral Maxillofac Implants 27:551–560
Silva-Neto JP, Nóbilo MAA, Penatti MPA, PC S Jr, Neves FD (2012) Influence of methodologic aspects on the results of implant-abutment interface microleakage tests: a critical review of in vitro studies. Int J Oral Maxillofac Implants 27:793–800
Mombelli A, Muller N, Cionca N (2012) The epidemiology of peri-implantitis. Clin Oral Implants Res 23(Suppl. 6):67–76
Heitz-Mayfield LJA, Mombelli A (2014) The therapy of peri-implantitis: a systematic review. Int J Oral MaxiIlofac Implants 29(suppl):325–345
Mombelli A, Decaillet F (2011) The characteristics of biofilms in peri-implant disease. J Clin Periodontol 38(Suppl. 11):203–213
Baggi L, Di Girolamo M, Mirisola C, Calcaterra R (2013) Microbiological evaluation of bacterial and mycotic seal in implant systems with different implant-abutment interfaces and closing torque values. Implant Dent 22:344–350
Zipprich H, Weigl P, Lange B, Lauer HC (2007) Erfassung, ursachen und folgen von mikrobewegungen am implantat- abutment-interface. Implantol 15:31–46
Romanos GE, Biltucci MT, Kokaras A, Paster BJ (2014) Bacterial composition at the implant-abutment connection under loading in vivo. Clin Implant Dent Relat Res. doi:10.1111/cid.12270[Epub ahead of print]
Harder S, Quabius ES, Ossenkop L, Kern M (2012) Assessment of lipopolysaccharide microleakage at conical implant-abutment connections. Clin Oral Invest 16:1377–1384
Bozkaya D, Muftu S (2005) Mechanics of the taper integrated screwed-in (TIS) abutments used in dental implants. J Biomech 38:87–97
Aguirrebeitia J, Abasolo M, Vallejo J, Ansola R (2013) Dental implants with conical implant-abutment interface: influence of the conical angle difference on the mechanical behavior of the implant. Int J Oral Maxillofac Implants 28:e72–e82
Nentwig HG (2004) The Ankylos Implant System: concept and clinical application. J Oral Implantol 30(3):171–177
Bozkaya D, Muftu S (2004) Efficiency considerations for the purely tapered interference fit (TIF) abutments used in dental implants. J Biomech 126:393–401
Sannino G, Barlattani A (2013) Mechanical evaluation of an implant-abutment self-locking taper connection: finite element analysis and experimental tests. Int J Oral MaxiIlofac Implants 28:e17–e26
Ricomini Filho AP, Fernandes FSF, Straioto FG, Silva WJ, Del Bel Cury AA (2010) Preload loss and bacterial penetration on different implant-abutment connection systems. Braz Dent J 21(2):123–129
Koutouzis T, Wallet S, Calderon N, Lundgren T (2011) Bacterial colonization of the implant–abutment interface using an in vitro dynamic loading model. J Periodontol 82(4):613–618
Alves DCC, Carvalho PSP, Martinez EF (2014) In vitro microbiological analysis of bacterial seal at the implant- abutment interface using two Morse taper implant models. Braz Dent J 25(1):48–53
Jansen VK, Conrads G, Richter E (1997) Microbial leakage and marginal fit of the implant/abutment interface. Int J Oral Maxillofac Implants 12(4):527–540
Aloise JP, Curcio R, Laporta MZ, Rossi L, Silva AMA, Rapoport A (2010) Microbial leakage through the implant–abutment interface of Morse taper implants in vitro. Clin Oral Implant Res 21:328–335
International Organization for Standardization (2007) International Standard ISO 14801–Dentistry–Implants–Dynamic Fatigue Test for Endosseous Dental Implants. International Organization for Standardization, Geneva
Cibirka RM, Nelson SK, Lang BR, Rueggeberg FA (2001) Examination of the implant-abutment interface after fadigue testing. J Prosthet Dent 85(3):268–275
Waal YC, Winkel EG, Meijer HJ, Raghoebar GM, Winkelhoff AJ (2014) Differences in peri-implant microflora between fully and partially edentulous patients: a systematic review. J Periodontol 85:68–82
Steinebrunner L, Wolfart S, Bössmann K, Kern M (2005) In vitro evaluation of bacterial leakage alonng the implant-abutment interface of different implant systems. Int J Oral Maxillofac Implants 20(6):875–881
Saidin S, Kadir MRA, Sulaiman E, Kasim NHA (2012) Effects of different implant–abutment connections on micromotion and stress distribution: prediction of microgap formation. J Dent 40:467–474
Zabler S, Rack T, Rack A, Nelson K (2012) Fatigue-induced deformation of taper connections in dental titanium implants. Int J Mater Res 103:207–216
Dibart S, Warbington M, Su MF, Skobe Z (2005) In vitro evaluation of the implant abutment bacterial seal: the locking taper system. Int J Oral Maxillofac Implants 20(5):732–737
Merz BR, Hunenbart S, Belser UC (2000) Mechanics of the implant abutment connection: an 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants 15(4):519–526
Elias CN, Figueira DC, Rios PR (2006) Influence of the coating material on the loosing of dental implant abutment screw joints. Mater Sci Eng C26:1361–1366
Coppedê AR, Mattos MGC, Rodrigues RCS, Ribeiro RF (2009) Effect of repeated torque/mechanical loading cycles on two different abutment types in implants with internal tapered connections: an in vitro study. Clin Oral Implant Res 20:624–632
Semper W, Heberer S, Mehrhof J, Schink T, Nelson K (2010) Effects of repeated manual disassembly and reassembly on the positional stability of various implant-abutment complexes: an experimental study. Int J Oral Maxillofac Implants 25(1):86–94
Rack T, Zabler S, Rack A, Riesemeier H, Nelson K (2013) An in vitro pilot study of abutment stability during loading in new and fatigue-loaded conical dental implants using synchrotron-based radiography. Int J Oral Maxillofac Implants 28:44–50
Coelho PG, Sudack P, Suzuki M, Kurtz KS, Romanos GE, Silva NRFA (2008) In vitro evaluation of the implant abutment connection sealing capability of different implant systems. J Oral Rehabil 35:917–924
Bernardes SR, Mattos MGC, Hobkirk J, Ribeiro RF (2014) Loss of preload in screwed implant joints as a function of time and tightening/untightening sequences. Int J Oral Maxillofac Implants 29:89–96
D’Ercole S, Tripodi D, Ravera L, Perrotti V, Piattelli A, Iezzi G (2014) Bacterial leakage in Morse cone internal connection implants using different torque values: an in vitro study. Implant Dent 23:175–179
Acknowledgments
The authors would like to thank Gilca Lacerda Saba and Tatiana Ricci da Silva for their excellent technical expertise.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Deceles Cristina Costa Alves declares that she has no conflict of interest. Paulo Sérgio Perri de Carvalho declares that he has no conflict of interest. Carlos Nelson Elias declares that he has no conflict of interest. Eduardo Vedovatto declares that he has no conflict of interest. Elizabeth Ferreira Martinez declares that she has no conflict of interest.
Funding
The work was supported by the authors.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This is not applied in this in vitro study.
Rights and permissions
About this article
Cite this article
Alves, D.C.C., de Carvalho, P.S.P., Elias, C.N. et al. In vitro analysis of the microbiological sealing of tapered implants after mechanical cycling. Clin Oral Invest 20, 2437–2445 (2016). https://doi.org/10.1007/s00784-016-1744-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1744-0