Abstract
Background
An unintended dural tear (DT) is the most common intraoperative complication of lumbar spine surgery. The unilateral biportal endoscopic technique (UBE) has become increasingly popular for treating various degenerative diseases of the lumbar spine; however, the DT incidence and risk factors specific to UBE remain undetermined. Therefore, this study aimed to evaluate the incidence and risk factors of DTs in UBE.
Method
Data from all patients who underwent UBE for degenerative lumbar spinal diseases from November 2018 to December 2021 at our institution were used to assess the effects of demographics, diagnosis, and type of surgery on unintended DT risk.
Results
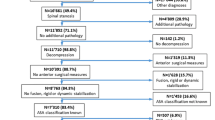
Overall, 24/608 patients (3.95%) experienced DTs and were treated with primary suture repair or bed rest. Although several patients experienced mild symptoms of cerebrospinal fluid (CSF) leaks, no serious postoperative sequelae such as nerve root entrapment, meningitis, or intracranial hemorrhage occurred. Additionally, no significant correlations were identified between DT and sex (P = 0.882), body mass index (BMI) (P = 0.758), smoking status (P = 0.506), diabetes (P = 0.672), hypertension (P = 0.187), or surgeon experience (P = 0.442). However, older patients were more likely to experience DT than younger patients (P = 0.034), and patients with lumbar spinal stenosis (LSS) were more likely to experience DT than patients with lumbar disc herniation (LDH) (P = 0.035). Additionally, DT was more common in revision versus primary surgery (P < 0.0001) and in unilateral laminotomy with bilateral decompression (ULBD) versus unilateral decompression (P = 0.031). Univariate logistic regression analysis revealed that age, LSS, ULBD, and revision surgery were significant risk factors for DT.
Conclusions
In this UBE cohort, we found that the incidence of DT was 3.95%. Additionally, older age, LSS, ULBD, and revision surgery significantly increased the risk of DT in UBE surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unintended dural tears (DTs) are frequent complications of lumbar spinal surgery. In previous studies, the incidence of DT has varied greatly and depended on various factors, including demographic characteristics, diagnosis, surgical history (primary versus revision), and invasiveness [2, 3, 5, 11, 13, 18, 19, 24, 26, 27, 30, 31, 33, 37,38,39]. Inappropriate tear management may result in persistent cerebrospinal fluid (CSF) leaks and the formation of pseudomeningoceles or cutaneous fistulas [3, 8], which, in turn, leads to symptoms of low CSF pressure such as headache and nausea. It is also possible for patients to experience more severe complications, including nerve root entrapment [21, 22], meningitis [16, 34], surgical site infections [1, 8], and intracranial hemorrhage [7, 17, 40]. In summary, the effects of DTs may result in increased healthcare costs and poor patient satisfaction [20, 25, 35].
In 2013, Soliman [28] used the unilateral biportal endoscopic (UBE) technique to treat lumbar disc herniation (LDH) according to the first technical description by Antoni and Claro from 1996 [4]. With the continuous optimization of surgical instruments and improvement of surgical techniques, UBE has gradually been implemented to treat various spinal degenerative diseases, including LDH, lumbar spinal stenosis (LSS) [10, 29], degenerative lumbar spondylolisthesis (DLS) [9, 14], and cervical radiculopathy [12, 23]. Compared with open surgery, UBE possesses the general merits of minimally invasive surgery, including less trauma, less blood loss, and faster recovery [15]. Furthermore, this technique is better than single-portal spinal endoscopic surgery because of the division, and thus, lack of interference, between its two percutaneous portals. Surgical instruments and endoscopes can therefore be moved freely without portal limitations, enabling convenient and flexible operations.
Although many previous studies have already reported the incidence of DTs associated with minimally invasive spine surgery, literature on DTs resulting from UBE is scarce [24]. Therefore, this study aimed to evaluate the incidence and risk factors of DTs in UBE.
Methods and materials
Patient population
We retrospectively evaluated the data of patients who experienced DTs from an initial cohort of 608 consecutive patients who had undergone UBE for degenerative lumbar spine disorders between November 2018 and December 2021 at our institution.
The inclusion criteria were as follows: (1) neurogenic claudication or radicular leg pain due to degenerative lumbar spine disorders that persisted longer than 6–8 weeks despite conservative treatment; (2) computed tomography and magnetic resonance imaging confirmation of a degenerative lumbar spine disorder including lumbar disc herniation, lumbar spinal stenosis, degenerative spondylolisthesis and spondylolisthesis; (3) UBE primary surgery performed to treat the degenerative lumbar spine disorder including the single-segment surgery and multi-segment surgery; (4) UBE revision surgery performed to treat the recidivate hernias and restenosis.
The exclusion criteria were as follows: (1) aged < 18 years; (2) concomitant issues such as traumatic injuries, primary infections, and tumors; and (3) other types of minimally invasive spine procedures, such as microendoscopic lumbar decompressive surgery, and percutaneous transforaminal endoscopic discectomy.
The study was approved by our institutional review board and informed consent was obtained from all patients (sl⁃xjs2019⁃001).
Surgical procedure
Patient preparation
All surgeries were performed under general endotracheal anesthesia. The patient was placed prone on a radiolucent frame with an H-shaped pillow placed underneath. Thus, the abdomen was suspended and increased abdominal pressure was avoided.
Skin incisions and making portals
Following target level confirmation under C-arm fluoroscopic guidance, the radiolucent frame was adjusted so that the operative intervertebral disc space was perpendicular to the floor. Two incision markers were placed at the inner margin of the pedicle, 1 cm above and below the midline of the intervertebral space. The skin and subcutaneous tissues were pierced perpendicularly according to the incision markings, and serial dilators were inserted into the two incisions to dissect the muscle and form two portals. For a left-sided approach, the left-hand portal was approximately 6 mm in diameter and used as the observation portal for endoscope placement, while the right portal was approximately 10 mm in diameter and was employed as the working portal to manipulate surgical instruments.
Creating an extraforaminal working space
Once the endoscope was inserted into the observation portal, a saline irrigation system was used to keep the operative field clean. The system was gravity-driven and hung 50–60 cm above the patient. The soft tissues covering the operative intervertebral disc space were dissected using a radiofrequency knife to create an initial extraforaminal working space.
Laminotomy and ligamentum flavum removal
When the inner edge of the facet joint, lower edge of the superior lamina, upper edge of the inferior lamina, and superficial layer of the ligamentum flavum were exposed, an endoscopic drill and Kerrison punches were used to perform laminotomy to expose the superior margin of the ligamentum flavum. The ligamentum flavum and dural sac were detached carefully using a curette. The ligamentum flavum was then peeled from the cranial end down to the caudal end using a Kerrison punch to expose the dural sac and traversing nerve root.
Decompression
After flavectomy, the nerve root adjacent to the dural sac was exposed, and a Kerrison punch and drills were used to enlarge the working space as needed.
Discectomy was required for cases of symptomatic LDH. The surgeon used pituitary forceps to remove the herniated disc, while the dural sac and nerve root were protected by an assistant using a retractor. If lateral recess decompression was required, the operator preferred medial facetectomy to decompress the transverse nerve root.
For patients with DLS requiring interbody fusion, we preferred to perform biportal endoscopic transforaminal lumbar interbody fusion (BETLIF). An endoscopic drill and a Kerrison punch were used to perform ipsilateral laminectomy, contralateral sublaminar decompression, and flavectomy. After the unilateral traversing root was completely exposed, a Kerrison punch was used to perform unilateral facetectomy, and the disc was removed using pituitary forceps. Curettes were then used to remove the cartilaginous endplate and expose the subchondral bone. Once the endplate preparation was sufficient under endoscopic visualization, autologous bone debris chips from the lamina and facet were introduced into the disc space, using a specialized cannula.
Finally, a cage packed with autologous bone was inserted under fluoroscopic guidance, with the nerve roots retracted by the operative assistant. Two ipsilateral pedicle screws were inserted into the two portals, and two contralateral pedicle screws were inserted into two new contralateral incisions.
Wound closure
After sufficient decompression and meticulous hemostasis, the endoscope and instruments were removed. Subsequently, a small drainage catheter was inserted through the working portal to prevent the epidural hematoma, followed by wound closure with two single stitches.
Unintended DTs
Unintended DTs were defined as the disruption of dural integrity with or without CSF leakage. If the arachnoid mater was visible during surgery, a DT was considered present, regardless of the presence of CSF leaks. CSF leakage was defined as the escape of CSF from the skin incision. The occurrence of unintended DTs was indicated by a presentation of low CSF pressure, including headache and nausea, after substantial postoperative drainage volume.
Patients with DTs measuring less than 10 mm were treated with bed rest and inpatient observation for 3–5 days, while primary suture repair was attempted for tears measuring more than 10 mm.
Study measures
The following four categories of potential factors were examined: (1) the patients’ demographic characteristics, including age, sex, body mass index (BMI), smoking, diabetes, and hypertension; (2) preoperative diagnosis, e.g., LDH, LSS, and DLS; (3) revision versus primary surgery; and (4) surgical type, including unilateral decompression (UD), unilateral laminotomy for bilateral decompression (ULBD), and transforaminal lumbar interbody fusion using the UBE technique (BETLIF). Following the surgery, the surgeon documented the occurrence and details of the DT, as well as management or repair techniques.
BMI was defined based on the BMI classification of Asian people by WHO and that of Chinese people by the Chinese Medical Association [36]. Accordingly, weight was classified as normal when the BMI was < 24, overweight when the BMI was > 24, and obese if the BMI was > 28.
Statistical analysis
The relationship between DTs and potential risk factors was subsequently analyzed. Pearson’s chi-square test was used to evaluate categorical differences between the two groups, while univariate logistic regression analyses were used to calculate the relative risk (RR) and 95% confidence intervals (CI). All statistical analyses were performed using SPSS Statistics version 26 (IBM Corporation, Armonk, NY, USA), and statistical significance was determined at a P value of 0.05.
Results
Demographic characteristics of the patients are provided in Table 1. Between November 2018 and December 2021, 608 consecutive patients (295 women, 313 men) underwent UBE. The mean patient age was 54 years, and LDH was the most common preoperative diagnosis (385 cases), followed by LSS (144 cases) and DLS (71 cases).
The incidence of unintended DTs is reported in Table 2. DTs were observed in 24 patients (ten women, 12 men; 3.95%). Compared to patients without DTs, those with DTs were significantly older (mean age, 61 years); however, sex distribution did not differ between patients with and without DT. In addition, BMI, smoking status, and diabetes did not significantly increase the risk of DTs during UBE surgery (Fig. 1). In this study, patients with LSS and DLS were more likely to experience DTs, with rates of 6.85% and 4.35%, respectively, compared to patients with LDH (2.86%). Furthermore, unintended DTs occurred in 2.93% and 6.72% of patients who had undergone bilateral decompression and UD, respectively, and unintended DTs were significantly more common in patients who underwent revision surgery (28.57%) than in those who underwent primary surgery (3.37%).
All procedures were performed by a senior spine surgeon with extensive experience who received UBE-associated training at several spinal centers. To investigate the influence of the surgeon’s experience on the risk of DT, we analyzed the incidence of dural tears in the first 100 patients and last 100 patients separately. Moreover, to avoid the influence of other factors, 200 patients who underwent primary UBE for LDH treatment were also analyzed. The incidence of tears was 5% among the first 100 LDH patients and 2% among the last 100 LDH patients. However, the difference in tear incidence between the groups was not significant (P = 0.465).
An overview of the univariate analysis of DT risk factors is presented in Table 3. The results indicated that age (odds ratio [OR] = 2.384, P = 0.039), LSS (OR = 2.500, P = 0.041), ULBD (OR = 2.224, P = 0.088), and revision surgery (OR = 11.480, P < 0.0001) were significant risk factors. Additionally, unintended DTs were recognized during surgery in 18/24 patients, and postoperatively in the remaining six. Only one of the 18 patients whose DT was identified during the primary surgery received suturing during surgery, and the remaining 23 patients received careful observation. Of the 24 patients, eight experienced headaches and nausea due to low CSF pressure, which recovered gradually within a few days with bed rest. Furthermore, one patient developed postoperative delirium, which may have been caused by spinal cord hypertension due to intraoperative saline irrigation; however, no wound infections or subcutaneous fluid collections occurred, and revision surgery was not required.
Discussion
An unintended DT is a common intraoperative complication of degenerative lumbar spine surgery, with an incidence ranging from 1.6 to 15.8% [2, 3, 5, 8, 11, 13, 18, 19, 24, 26, 27, 30,31,32,33, 37,38,39]. In this current study, 3.95% of patients undergoing UBE experienced DT, and this value is consistent with those from previous studies. Several factors affect the incidence of DT, including diagnosis and surgical history (revision versus primary), as well as surgical type.
Preoperative diagnosis determines the surgical goals and surgical type selected, thus affecting the degree of surgical invasiveness and complexity, which, in turn, impacts the risk of DTs [2]. Previously, Smorgick et al. [27] conducted a prospective study of 523 patients undergoing spine surgery and found DT rates of 4.6% for LDH, 12.8% for LSS, and 4.18% for DLS. Furthermore, Du et al. [5] reviewed data from 4822 patients and found that the diagnosis of LSS was a significant preoperative risk factor. Our study numbers were comparable to those of these previous studies, and DT was more common in patients with LSS than in patients with LDH.
Compared to LDH patients, patients with LSS presented with more severe degenerative changes in the lumbar spine, including hypertrophy of the laminae, facet joints, and ligamentum flavum, as well as instability of lumbar spine. These degenerative changes may account for the adherence of the joint capsule and ligamentum flavum to the dura mater, increasing the risk of DTs when the facet joints and ligamentum flavum are removed. Patients with LSS have severe degenerative changes and often require multi-segmental or bilateral decompression to completely decompress and relieve symptoms. This increases the invasiveness and complexity of the required procedure and prolongs operative time. Thus, the likelihood of DT occurrence also increases. Additionally, patients with LSS tend to be older than those with LDH. As a result, the dura mater is more fragile and is more easily torn.
BETLIF would seem more likely to cause DTs due to its greater surgical invasiveness and technical demands. However, many previous studies have shown that the incidence of DTs among patients who underwent laminectomy with instrumented fusion appears to be comparable to that seen among patients who underwent laminectomy alone [5, 27, 38]. This outcome is similar to our results. However, we were unable to identify a significant difference between the incidence of DT related to laminectomy without instrumented fusion and DT incidence related to BETLIF. Compared with laminectomy without instrumented fusion, the BETLIF procedure requires the exposure of a broader surgical field. This improves visualization and reduces the DT risk. Moreover, postoperative drainage volumes are increased in BETLIF, which can obfuscate the presence of CSF leaks and result in failure in identification of DTs.
Previously, Tsutsumimoto [33] collected prospective data from 555 patients and found DT rates of 3.78% for UD and 12.5% for ULBD. Similarly, a higher DT rate in patients who underwent ULBD was also observed in our current study. However, most patients underwent ULBD for relief of neurogenic claudication symptoms due to LSS, which is considered a risk factor for DT, as previously described. To exclude the influence of preoperative diagnosis on DTs, we analyzed the incidence of DTs in patients with LSS who underwent ULBD and UD and found no significant difference between the two groups. Therefore, it appears that LSS is the reason for the high incidence of DTs in ULBD. In our study, out of 73 patients with LSS who underwent ULBD, only two patients experienced DTs. However, any conclusion drawn from this small sample size is unreliable and requires further study with larger sample size.
A significantly increased DT risk has been reported with revision procedures [2, 5, 11, 27, 30,31,32, 38]. In a study of 1549 cases, Tafazal and Sell [32] found DT rates of 3.5% and 13.2% in primary and revision discectomy, respectively. Additionally, using multivariate analysis of detailed data from 4652 patients, Ishikura et al. [11] identified revision surgery as a vital risk factor for DTs. In our study, we also found that unintentional DTs were significantly more common among patients who had previously undergone surgery. Therefore, revision surgery may cause scar formation at the surgical site, leading to dural adhesion to adjacent tissue and thus affecting the recognition of normal tissue structure, which may be responsible for the high incidence of DTs in revision surgery.
Aging is also known to adversely affect outcomes in spinal surgery. Challenges related to this include poor surgical wound healing, surgical site infections, failure to fusion, and more reoperations. Numerous studies have demonstrated that unintended DT is common in older patients [2, 5, 11, 26, 27, 31, 33, 38, 39]. In fact, one previous study found that patients with DTs were older than those without [33]. Therefore, there is no doubt that when the patient group is more advanced in age, LSS, and DLS predominate. In contrast, LDH is more prevalent in younger patients. Pathological variations alter the goal of surgery and procedure selection, and these variables may affect DT incidence.
Strömqvist et al. [31] classified 64,431 patients into three diagnostic groups: LDH, LSS, and DLS. They found that older patients were more likely to experience DTs, regardless of the diagnosis [31]. This is due to the fragile dura mater that occurs with aging, as well as adhesions between the dura sac and surrounding tissue. Comparably, in the current study, we found that patients with DTs were significantly older than those without DTs.
In addition to aging, preoperative diagnosis, and surgical type, other variables such as concomitant chronic diseases (diabetes, hypertension, or obesity) and harmful habits like smoking may also influence the occurrence of DTs during spinal surgery. However, none of these factors significantly affected DT risk in our study.
Regarding the surgeon’s surgical experience, it remains controversial whether it affects the incidence of DTs. Some studies suggest that surgical experience does not significantly affect the incidence of DTs [18, 19]; however, other studies have reported that less experienced surgeons cause more DTs [26, 33, 37]. In this current study, we did not identify any significant correlations between the incidence of DTs and the experience of the surgeon.
Primary suture repair is the gold standard for the management of intraoperative DTs [6]. However, UBE offers limited working space; therefore, suturing the dura can be challenging. Additionally, the decreased operative space in UBE reduces the risks of persistent CSF leak and pseudo-meningocele formation. We found that most DTs did not require primary suture repair and healed spontaneously. We believe that if the dural tear was identified during the operation, the operation should be terminated as soon as possible to avoid adverse consequences such as intracranial hypertension caused by long-term intradural water pressure perfusion. Dural tears < 10 mm in size are usually treated with 72 h of bed rest and in-hospital observation while those > 10 mm in size need to be sutured. Although a few patients experienced headaches and nausea, the symptoms of low CSF pressure were relieved with a few days of bed rest. Moreover, we did not observe any serious sequelae in patients who were conservatively managed.
This study had several limitations. First, as a single-center study, selection bias may have occurred during patient enrollment and resulted in either overestimations or underestimations. Second, since most data points were categorical rather than continuous, potential covariates could not be assessed. For example, smoking history was recorded as “yes” or “no,” without details regarding the timeframe or longevity involved. Similarly, average glucose levels were not recorded, and diabetes severity was not considered as a risk factor. Finally, the major weakness of this study was the lack of detailed information regarding the unintended DTs themselves, such as the location of the dural tear in each case, the size of the dural tear, the operation performed at the time, and the instruments used.
Conclusion
In this study, based on univariate analysis results from 608 patients, age, revision surgery, LSS, and ULBD were found to be significant risk factors for DT. By understanding these risk factors, surgeons may be better prepared for this kind of complication and should ensure that patients are appropriately informed prior to surgery.
Data availability
The datasets used in this study are available from the corresponding author on reasonable request.
Abbreviations
- BETLIF:
-
Biportal endoscopic transforaminal lumbar interbody fusion
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- CSF:
-
Cerebrospinal fluid
- DLS:
-
Degenerative lumbar spondylolisthesis
- DT:
-
Dural tear
- LDH:
-
Lumbar disc herniation
- LSS:
-
Lumbar spinal stenosis
- RR:
-
Relative risk
- UBE:
-
Unilateral biportal endoscopic
- UD:
-
Unilateral decompression
- ULBD:
-
Unilateral laminotomy for bilateral decompression
References
Apisarnthanarak A, Jones M, Waterman BM, Carroll CM, Bernardi R, Fraser VJ (2003) Risk factors for spinal surgical-site infections in a community hospital: a case-control study. Infect Control Hosp Epidemiol 24:31–36
Baker GA, Cizik AM, Bransford RJ, Bellabarba C, Konodi MA, Chapman JR, Lee MJ (2012) Risk factors for unintended durotomy during spine surgery: a multivariate analysis. Spine J 12:121–126
Cammisa FP Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS (2000) Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 25:2663–2667
De Antoni DJ, Claro ML, Poehling GG, Hughes SS (1996) Translaminar lumbar epidural endoscopy: anatomy, technique, and indications. Arthroscopy 12:330–334
Du JY, Aichmair A, Kueper J, Lam C, Nguyen JT, Cammisa FP, Lebl DR (2014) Incidental durotomy during spinal surgery: a multivariate analysis for risk factors. Spine (Phila Pa 1976) 39(22):E1339-45
Epstein NE (2013) A review article on the diagnosis and treatment of cerebrospinal fluid fistulas and dural tears occurring during spinal surgery. Surg Neurol Int 4(Suppl 5):S301–S317
Graffeo CS, Perry A, Wijdicks EF (2017) Subarachnoid hemorrhage and spinal subdural hematoma due to acute CSF hypotension. Neurocrit Care 26:109–114
Guerin P, El Fegoun AB, Obeid I, Gille O, Lelong L, Luc S, Bourghli A, Cursolle JC, Pointillart V, Vital JM (2012) Incidental durotomy during spine surgery: incidence, management and complications A retrospective review. Injury 43:397–401
Heo DH, Son SK, Eum JH, Park CK (2017) Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus 43:E8
Hwa Eum J, Hwa Heo D, Son SK, Park CK (2016) Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neurosurg Spine 24:602–607
Ishikura H, Ogihara S, Oka H, Maruyama T, Inanami H, Miyoshi K, Matsudaira K, Chikuda H, Azuma S, Kawamura N, Yamakawa K, Hara N, Oshima Y, Morii J, Saita K, Tanaka S, Yamazaki T (2017) Risk factors for incidental durotomy during posterior open spine surgery for degenerative diseases in adults: a multicenter observational study. PLoS ONE 12:e0188038
Kang T, Park SY, Lee SH, Park JH, Suh SW (2020) Assessing changes in cervical epidural pressure during biportal endoscopic lumbar discectomy. J Neurosurg Spine 1–7
Khan MH, Rihn J, Steele G, Davis R, Donaldson WF 3rd, Kang JD, Lee JY (2006) Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976) 31:2609–2613
Kim JE, Choi DJ (2018) Biportal endoscopic transforaminal lumbar interbody fusion with arthroscopy. Clin Orthop Surg 10:248–252
Kim S, Kang S, Hong Y, Park S, Lee S (2018) Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: a multicenter, retrospective analysis. J Orthop Surg Res 13:22
Lin TY, Chen WJ, Hsieh MK, Lu ML, Tsai TT, Lai PL, Fu TS, Niu CC, Chen LH (2014) Postoperative meningitis after spinal surgery: a review of 21 cases from 20,178 patients. BMC Infect Dis 14:220
Lu CH, Ho ST, Kong SS, Cherng CH, Wong CS (2002) Intracranial subdural hematoma after unintended durotomy during spine surgery. Can J Anaesth 49:100–102
McMahon P, Dididze M, Levi AD (2012) Incidental durotomy after spinal surgery: a prospective study in an academic institution. J Neurosurg Spine 17:30–36
Murray NJ, Demetriades AK, Rolton D, Nnadi C (2014) Do surgeon credentials affect the rate of incidental durotomy during spine surgery. Eur Spine J 23:1767–1771
Nandyala SV, Elboghdady IM, Marquez-Lara A, Noureldin MN, Sankaranarayanan S, Singh K (2014) Cost analysis of incidental durotomy in spine surgery. (Spine Phila Pa 1976) 39:E1042–E1051
Nishi S, Hashimoto N, Takagi Y, Tsukahara T (1995) Herniation and entrapment of a nerve root secondary to an unrepaired small dural laceration at lumbar hemilaminectomies. Spine (Phila Pa 1976) 20:2576–2579
Oterdoom DL, Groen RJ, Coppes MH (2010) Cauda equina entrapment in a pseudomeningocele after lumbar schwannoma extirpation. Eur Spine J 19(Suppl 2 (Suppl 2)):S158-161
Park JH, Jun SG, Jung JT, Lee SJ (2017) Posterior percutaneous endoscopic cervical foraminotomy and diskectomy with unilateral biportal endoscopy. Orthopedics 40:e779–e783
Park HJ, Kim SK, Lee SC, Kim W, Han S, Kang SS (2020) Dural tears in percutaneous biportal endoscopic spine surgery: anatomical location and management. World Neurosurg 136:e578–e585
Schroeder GD, Kepler CK, Alijanipour P, Kurd MF, Hollern D, Kumar P, Radcliff KE, Rihn JA, Anderson DG, Hilibrand AS, Vaccaro AR (2016) The economic implications of an incidental durotomy. Spine (Phila Pa 1976) 41:1548–1553
Sin AH, Caldito G, Smith D, Rashidi M, Willis B, Nanda A (2006) Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. J Neurosurg Spine 5:224–227
Smorgick Y, Baker KC, Herkowitz H, Montgomery D, Badve SA, Bachison C, Ericksen S, Fischgrund JS (2015) Predisposing factors for dural tear in patients undergoing lumbar spine surgery. J Neurosurg Spine 22:483–486
Soliman HM (2013) Irrigation endoscopic discectomy: a novel percutaneous approach for lumbar disc prolapse. Eur Spine J 22:1037–1044
Soliman HM (2015) Irrigation endoscopic decompressive laminotomy. A new endoscopic approach for spinal stenosis decompression. Spine J 15:2282–2289
Strömqvist F, Jönsson B, Strömqvist B (2010) Dural lesions in lumbar disc herniation surgery: incidence, risk factors, and outcome. Eur Spine J 19:439–442
Strömqvist F, Sigmundsson FG, Strömqvist B, Jönsson B, Karlsson MK (2019) Incidental durotomy in degenerative lumbar spine surgery - a register study of 64,431 operations. Spine J 19:624–630
Tafazal SI, Sell PJ (2005) Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J 14:287–290
Tsutsumimoto T, Yui M, Uehara M, Ohta H, Kosaku H, Misawa H (2014) A prospective study of the incidence and outcomes of incidental dural tears in microendoscopic lumbar decompressive surgery. Bone Joint J 96-B:641–645
Wang JC, Bohlman HH, Riew KD (1998) Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. J Bone Joint Surg Am 80:1728–1732
Weber C, Piek J, Gunawan D (2015) Health care costs of incidental durotomies and postoperative cerebrospinal fluid leaks after elective spinal surgery. Eur Spine J 24:2065–2068
WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157–163
Wiese M, Krämer J, Bernsmann K, Willburger RE (2004) The related outcome and complication rate in primary lumbar microscopic disc surgery depending on the surgeon’s experience: comparative studies. Spine J 4:550–556
Williams BJ, Sansur CA, Smith JS, Berven SH, Broadstone PA, Choma TJ, Goytan MJ, Noordeen HH, Knapp DR Jr, Hart RA, Zeller RD, Donaldson WF 3rd, Polly DW Jr, Perra JH, Boachie-Adjei O, Shaffrey CI (2011) Incidence of unintended durotomy in spine surgery based on 108,478 cases. Neurosurgery 68:117–123 (discussion 123-124)
Yoshihara H, Yoneoka D (2014) Incidental dural tear in spine surgery: analysis of a nationwide database. Eur Spine J 23:389–394
Zimmerman RM, Kebaish KM (2007) Intracranial hemorrhage following incidental durotomy during spinal surgery. A report of four patients. J Bone Joint Surg Am 89:2275–2279
Acknowledgements
The authors thank Editage for providing language help and proofreading assistance.
Funding
This research was supported by the Research Fund of Anhui Institute of Translational Medicine (No. 2022zhyx-C49); the Translational Medicine Research Foundation of the Second Hospital of Anhui Medical University (2022ZHYJ13); and by the Key Projects of Natural Science Research in Colleges and Universities in Anhui Province (2022AH040102).
Author information
Authors and Affiliations
Contributions
Hang Yu: Methodology, Writing-Original, Review, & Editing, Funding Acquisition. Qingzhong Zhao: Methodology, Investigation. Jianwei Lv: Conceptualization, Methodology. Jianjun Liu: Data Curation, Formal Analysis. Bin Zhu: Investigation, Formal Analysis. Lei Chen: Data Curation, Formal Analysis. Juehua Jing: Resources, Supervision, Project Administration. Dasheng Tian: Resources, Supervision, Writing- Review & Editing, Funding Acquisition.
Corresponding author
Ethics declarations
Research involving human participants
The study was approved by the ethics committee of the Second Hospital of Anhui Medical University (sl⁃xjs2019⁃001) and was performed in accordance with the ethical standard laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients prior to their inclusion in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, H., Zhao, Q., Lv, J. et al. Unintended dural tears during unilateral biportal endoscopic lumbar surgery: incidence and risk factors. Acta Neurochir 166, 95 (2024). https://doi.org/10.1007/s00701-024-05965-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-05965-8