Abstract
Background
There are multiple approaches to reach the sellar region using microscope or endoscope, which are the old sublabial, with its post-operative morbidities, or the uni-nostril transseptal, which has a limited working field. Another technique is the direct transnasal, which is associated with tissue sacrifice, and lastly the bi-nostril (one side transseptal-other side transnasal), aiming to preserve one of the septal flaps.
Method
We have 27 case studies using a new technique in which we access the sphenoid endoscopicaly through the nasal septum from both nostrils under the mucoperichondrial-periosteal flap.
Conclusion
This new technique provides easy way of wide exposure to the sphenoidal gate, with easier closure of the operative field.
Similar content being viewed by others
Introduction
Many surgical approaches have been advocated to reach the sphenoidal gate. Schloffer H. was the first to describe reaching the pituitary gland through the sphenoidal gate via lateral rhinotomy approach [8]. There is also the old sublabial approach as described by Halstead and Cushing [3, 5]. Hirsch advocates reaching the sphenoidal gate through the nasal septum [6], which evolved later after the innovation of the endoscope to the transseptal endoscopic approach [10], then the direct transnasal (uni-nostril or bi-nostril approaches) [7], and lastly the bi-nostril approach (one side transseptal with other side transnasal) to preserve one side of the sepal flaps [9].
The new bi-nostril transseptal approach uses both nostrils to enter through the septum with preservation of the anterior, middle septal cartilage and bone to reach the sphenoid sinus from both sides in relatively less vascular spaces with preservation of both septal flaps for later reconstruction.
This approach has been used in our institute (The Neuroscience Hospital in Baghdad\Iraq) since 2011. We have performed 27 cases with this approach in comparison to 42 cases performed by the uni-nostril transseptal endoscopic approach and 35 cases by the direct transnasal approach (Fig. 1).
Relevant surgical anatomy
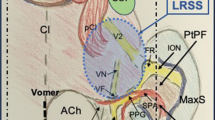
The nasal septum composed of an anterior cartilaginous and a posterior bony structure, perpendicularly oriented wall splitting the nasal cavity into two spaces covered by thick partly mucoperichondrial and partly mucoperiosteal layer covering the cartilaginous and the boney parts respectively from both sides as one continuous layer, giving oxygenation and nutrition to the underlying cartilage and bone. They take their rich blood supply anteriorly from the four arteries which form the Kiesselbach’s vascular plexus and posteriorly from the posterior ethmoid artery and the posterior nasal branch of the sphenopalatine artery, which run on the anterior face of the sphenoid sinus running below the sinus orifice (Fig. 2). This thick septal mucosal layer can be separated from both sides away from the underlying cartilage and bone as one continuous layer.
Description of the technique
The new technique involves applying decongestant to the nasal cavity then saline infiltration of the septal submucosal space followed by non-opposing anterior septal incisions. Then the mucosal flaps are elevated to the anterior wall of the sphenoid sinus and carrying on just lateral to the sphenoid ostium preserving their posterior pedicle with its vascular supply and stop elevation superiorly 1 cm below the level of the cribriform.
On the floor of the nose we could extend our dissection to a limit that gives enough space for the insertion of the speculum hence creating a bilateral sub mucosal tunnel spaces (Fig. 3).
The silastic sheets are fashioned to take the shape of the tunnel to prevent overriding of the septal flaps in the field of our work and protect the flaps from any damage could be caused by the speculum blades, which slide between the silastic sheets and the septum (Fig. 4).
The next step would be removal of the most posterior bony nasal septum and the bony rostrum between both sphenoidal ostei (Fig. 5).
This permits the introduction of the endoscope from one nostril and the surgical instruments through the other nostril with different viewing and working angles (Fig. 6, Videos 1 and 2).
At the end of the operation, a proper nasal hemostasis must be achieved then a coaptation absorbable sutures and/or a bilaterally silicon septal airway splints applied to hold both septal flaps together (Fig. 7).
In certain cases of a big sphenoidal roof or posterior sphenoidal wall defects, the above method of septal mucosal flap closure repair can be used. We start by stripping off all mucosa of the sphenoid sinus then filling the sphenoid cavity by material of repair like fat, fascia, cartilage or bone before applying the above flap closure technique illustrated in Fig. 7, keeping it in a well vascularized closed space, permitting a better healing of our reconstruction post operatively.
The new technique provides wide access with different viewing and working angles from both nostrils (Fig. 5, Videos 1 and 2), less bleeding and easier to perform. It also offers enough space for work using a four hands technique [1]. This is specifically important during the control of active bleeding during surgery [2].
The bi-nostril transseptal working angles allows an extended transsphenoidal work without the need to do ethmoidectomy and middle turbinate lateralisation.
This approach also permits preservation of the anterior cartilaginous septum when working on both sides of the cartilage without the need to remove or push the cartilage to the other side. In conditions where there is no marked posterior bony septal deviation requiring extensive removal, only 2 cm from the posterior part of the bony septum with the sphenoidal bony rostrum needs to be removed.
This method permits the preservation of both septal mucosal vascularized flaps for future reconstruction [4].
Follow up of patients whom underwent this approach after 4–8 weeks revealed well healed and near normal looking nasal cavities (Video 3).
Indications
In our practice the bi nostril transseptal approach is the preferred technique to be performed for removal of small sellar tumors, which previously used to be removed by the uni-nostril transseptal approach as it gives a better exposure.
It is also preferred for less extensive giant sellar tumors, which were previously removed by the bi-nostril direct transnasal approach, due to its shorter operative anesthesia time and the easiness of the reconstruction (Fig. 1).
Limitations
The bi-nostril transseptal approach could not be applied in cases of extensive sellar tumor with marked lateral extension of the tumor were more lateral exposure needed due to limitations in the lateral extension of the surgical field, in addition to the inability to add the trans-pterygoid exposure to the surgical field.
How to avoid complications
There is a possibility of a mucosal flap tear during flap elevation and silastic sheath advancement. This complication happened in 4 out of 28 cases and managed by coaptation absorbable sutures with application of a silicone septal airway splints for 2 weeks to hold both septal flaps against the underlying septum.
This complication can be avoided by meticulous flap elevation with gentle silastic sheets and nasal speculum blades advancement.
Specific perioperative consideration
The nasal septum should be assessed for conditions like septal perforation or adhesions, which make elevation of the septal mucosal flaps more difficult.
Postoperative care includes frequent use of saline with sodium-bicarbonate nasal douche, with scheduled endoscopic local nasal debridement in the office. The silicone septal airway splints should be removed 7–14 days post operatively.
Specific information
Patients need to be informed about the possibility of cribriform plate injury during removal of the posterior bony septum or if the surgeon misdirects the level of the sphenoid sinus through the bony septum to an upward direction, which might ends up with CSF rhinorrhea. Fortunately this has not happened in our practice.
Summary
This technique is preferable due to the following reasons:
-
Easy to perform.
-
Less operative anesthesia time.
-
Provides wide exposure.
-
The possibility of using four hands.
-
Less tissue sacrifice with less damage to the nasal mucosa
-
Less bleeding at the surgical site, which in turn results in less incidence of post op hemorrhage.
-
Protection, preservation and easier harvestation of the nasoseptal flaps [10], to be used for reconstruction if needed.
-
No nasal packing required.
-
Easier operative field closure and defects reconstruction.
-
Post op near normal nasal cavity.
References
Arnholt JL, Mair EA (2002) A ‘third hand’ for endoscopic skull base surgery. Laryngoscope 112:2244–2249
Briner HR, Simmen D, Jones N (2005) Endoscopic sinus surgery: advantages of the bimanual technique. Am J Rhinol 19:269–273
Cushing H (1914) Surgical experience with pituitary disorders. JAMA 63:1515–1525
Hadad G, Bassagasteguy L, Carrau RL et al (2006) A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 116:1882–1886
Halstead AE (1910) Remarks on the operative treatment of tumors of the hypophysis: with a report of two cases operated on by an oronasal method. Trans Am Surg Assoc 28:73–93
Hirsch O (1910) Endonasal method of removal of hypophyseal tumors. With report of two successful cases. JAMA 55:772–774
Jho HD, Carrau RL (1996) Endoscopy assisted transsphenoidal surgery for pituitary adenoma. Technical note. Acta Neurochir 138:1416–1425
Schloffer H (1907) Erfolgreich operation eines Hypophysentumors auf nasalem wage. Wien Klin Wochenschr 20:621–624
Stamm AC, Pignatari S, Vellutini E, Harvey RJ, Nogueira JF Jr (2008) A novel approach allowing binostril work to the sphenoid sinus. Otolaryngology Head Neck surg 138:531–532
Yaniv E, Rappaport ZH (1997) Endoscopic transseptal transsphenoidal surgery for pituitary tumors. Neurosurgery 40:944–946
Acknowledgements
I would like to thank Dr. Moneer k. Faraj MB CHB, FICMS, FACS, FICS, IFAANS, Consultant neurosurgeon who shared the work on the patients, we worked as a team in managing all the patients involved in this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest statement
The author certify that he has no affiliation with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultations, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendment or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study, with any possible risks and complications which might happen with this new procedure.
Electronic supplementary material
Intra operative video shows working from both nostrils within the nasal septum (MP4 2903 kb)
Video 2
Intra operative video shows control of active bleeding (MPG 8335 kb)
25 days post op reveals near normal nasal cavity (MP4 14,516 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Al-Baldawi, I.A. Bi-nostril transseptal endoscopic approach to the sphenoidal gate. A new technique. Acta Neurochir 159, 1247–1252 (2017). https://doi.org/10.1007/s00701-017-3193-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3193-1