Abstract
Background
Although previous studies have described the clinical features of the nervus intermedius (NI), no attempt has yet been made to describe the relationship between the ultrastructural and electrophysiological characteristics of the nervus intermedius and its motor competence.
Objective
In this study, we analyzed the intraoperative electrophysiological response obtained during vestibular schwannoma surgery. The ultrastructure was studied using electron microscopy.
Materials and Methods
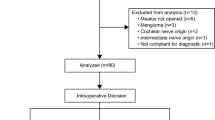
Thirty-six consecutive patients underwent microsurgery for vestibular schwannoma with cerebellopontine angle tumors. The patients were extensively monitored intraoperatively. Selective stimulation of the nervus intermedius was attempted in all cases. The patients were then examined postoperatively and followed for a minimum of 1 year. Forty-three isolated human brainstems were analyzed to collect the ultrastructural NI data.
Results
We found a correlation between the NI motor responses in the perinasal and perioral regions and the ultrastructure characteristics, with few (0.5 %) but large myelinated motor fibers (diameters >12 μm). Both characteristics are consistent with the clinical observation of transient weakness of the levator anguli oris muscle. These observations indicate a relationship between the intraoperative electrophysiological identification of the NI nervus intermedius and its clinical and ultrastructural characteristics.
Conclusions
Identifying the NI in the deformed anatomy of tumors could provide a fixed landmark during cerebellopontine surgery and help prevent damage of the facial nerve.





Similar content being viewed by others
References
Alfieri A, Fleischhammer J, Peschke E, Strauss C (2012) The nervus intermedius as a variable landmark and critical structure in cerebellopontine angle surgery: an anatomical study and classification. Acta Neurochir 154(7):1263–1268
Alfieri A, Fleischhammer J, Prell J (2011) The functions of the nervus intermedius. AJNR 32(7):E144
Alfieri A, Strauss C, Prell J, Peschke E (2010) History of the nervus intermedius of Wrisberg. Ann Anat 192(3):139–144
Ashram YA, Jackler RK, Pitts LH, Yingling CD (2005) Intraoperative electrophysiologic identification of the nervus intermedius. Otol Neurotol 26(2):274–279
Irving RM, Viani L, Hardy DG, Baguley DM, Moffat DA (1995) Nervus intermedius function after vestibular schwannoma removal: clinical features and pathophysiological mechanisms. Laryngoscope 105(8 Pt 1):809–813
Manzano GM, Giuliano LM, Nobrega JA (2008) A brief historical note on the classification of nerve fibers. Arq Neuropsiquiatr 66(1):117–119
Myrseth E, Moller P, Pedersen PH, Lund-Johansen M (2009) Vestibular schwannoma: surgery or Gamma knife radiosurgery? A prospective, nonrandomized study. Neurosurgery 64(4):654–661
Ozer FD, Duransoy YK, Camlar M (2009) Atypic geniculate neuralgia: atypic anatomic correlation of cranial nerve roots and AICA. Acta Neurochir 151(8):1003–1004
Park SH, Lee KY, Hwang SK (2013) Nervus intermedius dysfunction following Gamma Knife surgery for vestibular schwannoma. J Neurosurg 118(3):566–570
Prell J, Rampp S, Rachinger J, Scheller C, Naraghi R, Strauss C (2008) Spontaneous electromyographic activity during microvascular decompression in trigeminal neuralgia. J Clin Neurophysiol 25(4):225–232
Prell J, Rachinger J, Scheller C, Alfieri A, Strauss C, Rampp S (2010) A real-time monitoring system for the facial nerve. Neurosurgery 66(6):1064–1073
Prell J, Rampp S, Romstock J, Fahlbusch R, Strauss C (2007) Train time as a quantitative electromyographic parameter for facial nerve function in patients undergoing surgery for vestibular schwannoma. J Neurosurg 106(5):826–832
Rampp S, Rachinger J, Scheller C, Alfieri A, Strauss C, Prell J (2012) How many electromyography channels do we need for facial nerve monitoring? J Clin Neurophysiol 29(3):226–229
Rhoton AL Jr, Kobayashi S, Hollinshead WH (1968) Nervus intermedius. J Neurosurg 29(6):609–618
Sachs E Jr (1968) The role of the nervus intermedius in facial neuralgia. Report of four cases with observations on the pathways for taste, lacrimation, and pain in the face. J Neurosurg 28(1):54–60
Samii M, Gerganov VM, Samii A (2010) Functional outcome after complete surgical removal of giant vestibular schwannomas. J Neurosurg 112(4):860–867
Scheller C, Rachinger J, Prell J, Kornhuber M, Strauss C (2008) Schwannoma of the intermediate nerve. J Neurosurg 109(1):144–148
Stripf T, Braun K, Gouveris H, Stripf EA, Mann WJ, Amedee RG (2007) Influence of different approaches to the cerebellopontine angle on the function of the intermediate nerve. J Neurosurg 107(5):927–931
Tubbs RS, Mosier KM, Cohen-Gadol AA (2012) Geniculate neuralgia: clinical, radiologic, and intraoperative correlates. World Neurosurg 79(5–6):763–767
Acknowledgments
Drs. Alfieri and Rampp contributed equally to the study. We are grateful to Mr. Heine and Dr. Litvak for their remarkable contribution to this study. The patient authorized the publication of the images.
Conflicts of interest
None.
Funding
Wilhelm Roux Foundation, Martin Luther University Halle-Wittenberg, Germany
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alfieri, A., Rampp, S., Strauss, C. et al. The relationship between nervus intermedius anatomy, ultrastructure, electrophysiology, and clinical function. Usefulness in cerebellopontine microsurgery. Acta Neurochir 156, 403–408 (2014). https://doi.org/10.1007/s00701-013-1952-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1952-1