Abstract
Aims
Correct genetic diagnosis of maturity-onset diabetes of the young (MODY) is beneficial for person’s diabetes management compared to no genetic testing. Aim of the present study was a search for optimal time- and cost-saving strategies by comparing two approaches of genetic testing of participants with clinical suspicion of MODY.
Methods
A total of 121 consecutive probands referred for suspicion of MODY (Group A) were screened using targeted NGS (tNGS), while the other 112 consecutive probands (Group B) underwent a single gene test based on phenotype, and in cases of negative findings, tNGS was conducted. The study was performed in two subsequent years. The genetic results, time until reporting of the final results and financial expenses were compared between the groups.
Results
MODY was confirmed in 30.6% and 40.2% probands from Groups A and B, respectively; GCK-MODY was predominant (72.2% in Group A and 77.8% in Group B). The median number of days until results reporting was 184 days (IQR 122–258) in Group A and 91 days (44–174) in Group B (p < 0.00001). Mean costs per person were higher for Group A (639 ± 30 USD) than for Group B (584 ± 296 USD; p = 0.044).
Conclusions
The two-step approach represented a better strategy for genetic investigation of MODY concerning time and costs compared to direct tNGS. Although a single-gene investigation clarified the diabetes aetiology in the majority of cases, tNGS could reveal rare causes of MODY and expose possible limitations of both standard genetic techniques and clinical evaluation.
Similar content being viewed by others
Introduction
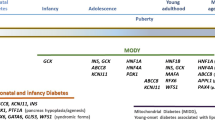
Maturity-onset diabetes of the young (MODY) implies rare forms of hyperglycaemia caused by a single gene defect that is transmitted to subsequent generations in an autosomal dominant manner [1]. Although disruptions in several genes have already been described as a cause of MODY, three subtypes prevail. GCK-MODY, clinically characterized as persistent, non-progressive hyperglycaemia, is caused by heterozygous variants in the glucokinase gene [2, 3]. Disruption of hepatocyte nuclear factor 1-alpha (HNF1A-MODY) [4] or 4-alpha (HNF4A-MODY) [5] leads to a progressive form of diabetes with a high risk of vascular complications and a requirement for pharmacological treatment [6].
Importantly, syndromic monogenic diabetes could be present in persons suspected to have MODY [7, 8]. The most prevalent causes of such diagnosis are disruption of the HNF1B gene leading to renal cysts and diabetes (RCAD) [9] and mitochondrial diabetes mellitus (mtDM), which could be accompanied by other comorbidities, such as hearing impairment, stroke, heart failure, myopathy and renal disease. [10].
The only possible confirmation of monogenic forms of diabetes is genetic testing. Dideoxy (Sanger) sequencing of the gene of interest (i.e., determination of a specific nucleotide in each position of the genetic region and comparison to the reference) [11] has represented the gold standard of molecular genetic testing of human disorders, including MODY, for decades. However, gross genetic rearrangements, such as whole HNF1B gene deletion, the most prevalent cause of RCAD [9], cannot be identified using this method. Multiplex ligation probe-dependent amplification (MLPA) is one of the possible approaches for the detection of these structural genetic changes. Moreover, traditional dideoxy sequencing is not able to precisely describe a proportion of altered variants in the mitochondrial DNA that cause mtDM [12]. The advent of next-generation sequencing (NGS) methods that allow massive parallel investigation of DNA are currently replacing the above-mentioned techniques in MODY diagnostics. Targeted next-generation sequencing (tNGS), which enables simultaneous detection of gene sequences of interest and could be designed and commercially prepared based on customer preference, represents a broadly used approach for genetic testing of persons susceptible to MODY or monogenic syndromic diabetes [13].
The correct genetic diagnosis for people with MODY represents a model example of a precision medicine approach: those with GCK-MODY do not require pharmacological treatment outside pregnancy, while low doses of sulfonylurea lead to better glycaemic control than insulin injections in subjects with HNF1A- and HNF4A-MODY [14, 15]. An important aspect of genetic testing is its cost. Several studies have already shown that biomarker testing followed by genetic diagnosis of MODY was cost-effective compared to no genetic testing [16]. However, an optimal cost-effective genetic testing strategy for persons with suspected MODY has not yet been established.
The aim of the present study was to compare the time and cost efficacy as well as the genetic and clinical findings of two approaches to molecular genetic testing commonly used for MODY diagnostics (tNGS alone versus single gene testing followed by tNGS).
Methods
Our centre serves as the country's leading institution for molecular-genetic investigation of genes related to monogenic diabetes. Samples are referred by diabetologists or other physicians, and the genetic test is financially covered by institutional and external grant sources and therefore free of charge for the persons. The required conditions for genetic testing are age at diabetes diagnosis between six months and 40 years, absence of pancreatic autoantibodies and at least one other factor: positive family history of diabetes (at least two consecutive generations with hyperglycaemia), absence of ketoacidosis at manifestation, detectable C-peptide and good metabolic control with diet, low doses of insulin or oral hypoglycaemic agents. Clinical and biochemical information collected for each proband included sex, current age, age at diagnosis of diabetes or hyperglycaemia, family history of diabetes, ketoacidosis at diagnosis, pancreatic autoantibody status, presence of diabetic complications and renal cysts, last HbA1c, BMI and current type of treatment. The blood samples of participants were collected into EDTA tubes, accompanied by signed informed consent for genetic testing, completed clinical questionnaires and sent via regular mail to the laboratory. On average, nine newly referred probands are investigated per month in our laboratory.
Study design and participants
Flow-chart of the study summarises Fig. 1.
Altogether, 233 samples from probands suspected of MODY were referred to our centre in two time periods (Group A: November 5th 2018–November 5th 2019 and Group B: November 6th 2019–December 31st 2020). Of note, the recruitment time of group B was extended for two months compared to Group A due to the pandemic of Covid-19; however, it did not significantly affect the clinical characteristics of the probands (Table 1) with the exception of age that had varied also in previous years in our registry (data not shown). Group A, consisting of 121 consecutive probands, was tested using tNGS (for details, please see below). If a plausible causal variant was observed, its presence was confirmed by dideoxy sequencing as described previously [17] with the exception of the m.3243A > G variant in the MT-TL1 gene in the mitochondrial DNA whose accurate detection and quantification was confirmed during initial validation process of the tNGS panel for monogenic forms of diabetes using several external positive controls provided by Kevin Colclough, Ph.D. from Medical School, University of Exeter, Exeter, United Kingdom. Group B consisted of 112 consecutive probands who underwent a single gene test that was selected by both geneticist and qualified diabetologist from the laboratory based on phenotypic questionnaire filled with referring health care professional of each proband and in cases of negative findings, this was followed by tNGS. If there was a positive finding using tNGS, the presence of a plausible causal variant was also confirmed by dideoxy sequencing. The majority of probands were initially tested for one gene by dideoxy sequencing: those with persistent, mild hyperglycaemia were first investigated for the GCK gene, and those with reported progressive hyperglycaemia requiring pharmacological treatment were first tested for the HNF1A gene. MLPA was performed first in three persons with diabetes and renal cysts. All patients from both groups included in this study were recruited from the same referring health care professionals across the whole country.
This study was approved by the institutional Ethics Committee of the 2nd Faculty of Medicine, Charles University and University Hospital Motol, Prague, the Czech Republic.
Genetic testing and bioinformatics evaluation
Genomic DNA was extracted from peripheral blood using the QIAmp DNA Blood Mini system (Qiagen, Hilden, Germany). Based on our previous experience with the investigation of monogenic forms of diabetes as well as hyperinsulinism and according to a literature review conducted in 2018, a set of 52 genes associated with pancreatic beta cell dysfunction was compiled (Online Resource 1). The respective protein coding sequences as well as adjacent genetic regions were targeted using a SureSelect Custom kit (Agilent Technologies, Santa Clara, CA, USA). The NGS library was prepared according to the manufacturer’s instructions, and indexed products were sequenced by synthesis on a MiSeq platform (Illumina, San Diego, CA, USA) with 200 × average coverage. Forty DNA samples were pooled and sequenced simultaneously per run.
Our bioinformatics pipeline is based on the Genome Analysis Toolkit (GATK) [18]. The first step of the protocol is performed by the Burrows–Wheeler Aligner [19] that maps the sequence reads from input FASTQ files to the human reference genome h19. The mitochondrial variant of interest (m.3243A > G) was called using the samtools mpileup command. A frequency of a variant allele (mutational heteroplasmy) at the position of interest exceeding 1% (of at least 200 reads) was considered diagnostic of mtDM. Subsequently, filtering of variants using the VarAFT tool [20] was performed, mainly based on (a) frequencies in the databases of variants (gnomAD—European, non-Finish population), (b) in silico online tools predicting the functional impact of the variant on the protein, (c) presence in the Human Gene Mutation Database or ClinVar, and then, if possible, (d) segregation of the variant with diabetes in the family. American College of Medical Genetics and Genomics (ACMG) standards and guidelines [21] implemented in VarSome software [22] were used for final evaluation and classification of the detected variants in the GCK gene while recommendations by the Monogenic Diabetes Variant Curation Expert Panel have been followed for the HNF1A and HNF4A gene variants (https://www.clinicalgenome.org/affiliation/50016). Finally, variants have been divided into five groups: pathogenic, likely pathogenic, benign, likely benign or as variants of uncertain significance (VUS).
Time and financial costs of genetic testing
The time expressed in days from the sample evidence until finalization of the genetic results report was compared between Groups A and B.
The financial costs include expenses for chemicals and expendable supplies from broadly used and reputable manufacturers as well as personal costs for laboratory work according to the tariff salary of our institution. The total cost of tNGS for one sample was 620 USD (400 USD for materials and 220 USD for laboratory work per 20 h). Dideoxy sequencing of all protein-coding regions and the promoter of the GCK or HNF1A gene (ten fragments were investigated for both genes) as well as MLPA cost 166 USD (111 USD for materials and 55 USD for laboratory work per 5 h). The price of dideoxy sequencing of one genetic region was 64 USD (9 USD for materials and 55 USD for laboratory work per 5 h). Concerning all types of methods, the 64.7% of total costs are attributed to supplies and 35.3% of total costs are attributed to the institutional salary.
Statistics analyses
Data are summarized as medians with interquartile ranges (IQRs) for continuous variables and as absolute and relative frequencies in the case of categorical variables. Differences between confirmed/rejected cases of MODY within Groups A and B were explored using nonparametric Wilcoxon’s two-sample test for continuous characteristics and Fisher’s exact test for categorical variables. In the time and cost comparison between Group A and Group B, both Wilcoxon’s two-sample test and the two-sample t-test were used, as the latter compares mean costs per person. Cost estimates are hence also expressed as the means ± SD (standard deviation). The level of statistical significance was set to 0.05. Statistical language and environment R, version 4.1.0, were used throughout the analysis [23].
Results
The median number of days from obtaining samples until reporting of the final genetic testing results (with or without a detected causal variant) was 184 days (IQR 122–258 days) in Group A and 91 days (IQR 44–174 days) in Group B (p < 0.00001, Fig. 2). The median financial expenses for genetic testing of MODY in Group A reached 620 USD (IQR 620–684), while the median cost in Group B was 786 USD (IQR 166–786, p < 0.00001). However, mean expenses per person were calculated to be higher for Group A (639 USD ± 30 USD) than for Group B (584 USD ± 296 USD, p = 0.044).
Overall, a genetic diagnosis of MODY was established in 81/233 (34.8%) and mitochondrial diabetes in 1/233 (0.4%) probands referred to our laboratory during the study. The diagnosis of MODY was confirmed in 36 out of 121 (29.8%) probands from Group A. Specifically, GCK MODY was revealed in 26/36 (72.2%), HNF4A-MODY in 6/36 (16.7%), and HNF1A-MODY in 4/36 (11.1%). One proband from Group A had mtDM (Table 2). Altogether, 45/112 (40.2%) probands from Group B were genetically confirmed to have MODY. Similar to Group A, the diagnosis of GCK-MODY prevailed (35/45, 77.8%). The second most prevalent subtype of MODY was HNF1A-MODY (6/45, 13.3%), followed by HNF4A-MODY (3/45, 6.7%) and KCNJ11-MODY (1/45, 2.2%) (Table 3). Out of 45 positive findings from Group B, 36 (80.0%) were detected after the first step of genetic testing by a single gene analysis using dideoxy sequencing. Seven persons were initially tested for other major MODY genes than the causal one. In addition, the pathogenic variant p.Val182Met in GCK was missed in one case. In one proband, who was negative for the GCK gene, tNGS revealed a pathogenic variant in the KCNJ11 gene. Online Resource 2 lists the observed variants classified as VUS in both groups.
Statistically significant differences between MODY and non-MODY probands (calculated for all included persons) were observed for the following clinical characteristics: sex (65.1% of women among MODY versus 50.7% of women among non-MODY; p = 0.039), age at study (median 20 years (IQR 14–36) versus median 35 years (IQR 20–43), p = 0.0008), age at diabetes diagnosis (median 14 years (IQR 10–24) versus median 28 years (IQR 15–35), p < 0.0001) and BMI (median 21.3 (18.3–24.2) versus median 25.2 (21.8–29.5), p < 0.0001). Moreover, probands with confirmed MODY were significantly more often without pharmacologic treatment compared to non-MODY subjects (p < 0.000001), which is in line with the fact that the GCK-MODY diagnosis dominated. Differences between MODY and non-MODY probands for the remaining studied clinical and biochemical parameters did not reach statistical significance (data not shown).
Discussion
We present the first study comparing the time- and cost-effectiveness of two currently available genetic testing strategies of participants susceptible to MODY. The results of the present study revealed that the two-step approach of genetic testing (Group B) was more time- and cost-saving compared to the direct performance of tNGS (Group A). Taking both studied groups together, (likely) pathogenic variants in one of the major MODY genes (GCK, HNF1A, HNF4A) were observed in 80/82 (97.6%) of all probands with a confirmed diagnosis of monogenic diabetes. This is one of the highest proportions reported thus far [24, 25], indicating that a single-gene investigation (with the acknowledged limitations discussed below) should represent a first genetic step on a journey to a correct diagnosis of MODY. Importantly, this strategy would be advisable for populations with a high prevalence of major subtypes of MODY, such as our European, non-Finish population. In populations where major subtypes of MODY are less frequently observed the initial performance of tNGS might be more suitable. The described strategy of single-gene testing in well clinically characterized persons followed by parallel sequencing techniques has also been recommended for other monogenic disorders, such as systemic auto-inflammatory diseases (SAID) in which three genes are recommended to test by dideoxy sequencing if clinical and biochemical prerequisites are met [26]. Recent study showed that out of 196 probands tested, 20.9% obtained genetic diagnosis of SAID of whom 78.0% carried pathogenic variant in the same gene [27].
Comparison of the time and financial demands of the two strategies
The significantly longer median time since sample receipt until results reporting in Group A was mainly caused by the fact that 40 DNA samples are processed simultaneously per run of tNGS, leading to longer waiting for the fulfilment of each batch. The tNGS procedure was selected based on our previous experience with NGS library preparation using Agilent technology [28], available NGS analysers at our institution and the need for optimizing financial expenses per sample. Concerning published reports of tNGS for MODY, several different platforms for custom tNGS library gene preparations as well as sequencing analysers are used in clinical practice [29, 30]. Although the number of DNA samples tested per run is lacking in almost all published studies, based on the average number of tested genes and dominate sequencing platforms, we can assume a similar or higher number of required samples per sequencing run. NGS analysers with lower capacity would increase the speed of obtaining NGS data. The sooner the correct diagnosis is established and treatment is optimized, the better the clinical and metabolic outcomes [31, 32]. Therefore, although monogenic diabetes is not an acute life-threatening condition, the speed of obtaining results matters.
While the median costs of a single-step approach of genetic testing (Group A) were significantly lower compared to expenses for a two-step genetic procedure (Group B), the average costs per person were higher for Group A than Group B. This putative discrepancy was caused by the fact that the financial costs of negative (620 USD for tNGS) and positive (620 USD for tNGS + 64 USD for dideoxy sequencing confirmation) genetic findings in Group A ranged within a narrow spectrum of values. On the other hand, detection of (likely) pathogenic variants in one of the prevalent MODY genes using dideoxy sequencing is relatively cheap (166 USD), while the costs of a final negative finding (no causal variant found using single gene testing: 166 USD and tNGS: 620 USD) are similar to genetic investigation in Group A (786 USD). Although financial expenses for genetic testing as well as the types of coverage vary in different countries, we believe that in general, these calculations and their conclusions could also be applied to other laboratories.
Pitfalls of initial single-gene testing
Interestingly, tNGS revealed an overlooked causal variant p.Val182Met in the GCK gene originally analysed using dideoxy sequencing in our study. A possible explanation could be the presence of a single nucleotide variant under one of the primers leading to amplification of only one allele [33].
The initial single gene testing did not reveal the causal variant in nine persons from Group B. While the overlooked variant in the GCK gene has been discussed above, other cases pointed out that the clinical presentation of persons could be overlapping among subtypes of MODY. For example, one proband with GCK-MODY carrying p.Gly294Asp was initially screened for the HNF1A gene because the oral glucose tolerance test increment reached 5 mmol/L, which is not in accordance with international recommendations for GCK gene testing [34]. Moreover, when all relevant clinical data are not available for correct assignment of the first gene analysis or when a causal variant is present in one of the very rare MODY genes, follow-up tNGS represents a good strategy to establish a correct diagnosis.
Variants in rare genes related to monogenic diabetes
Beyond (likely) pathogenic variants in the three most prevalent MODY genes, two additional DNA changes were classified as causative for diabetes in both groups. In one proband, tNGS showed m.3243A > G in the gene for tRNALeu in the mitochondrial DNA, an altered variant present in 28% of the sequence reads. Only diabetes was reported for this proband (diagnosed at 33 years of age, HbA1c 58 mmol/mol (7.5%), insulin treatment), as well as in her mother and maternal grandmother. The prevalence of mtDM among the genetically confirmed cases of monogenic diabetes was 1.2% (1/82), which is significantly lower than that in recent studies searching for syndromic monogenic diabetes among MODY in the United Kingdom [7] or France [8].
In persons from Group B, a pathogenic variant c.137A > C (p. His46Pro) in the KCNJ11 gene has been revealed. Heterozygous activating variants at the same nucleotide position c.137A > G (p. His46Arg) and c.137A > T (p. His46Leu) as well as the nearby variant c.136C > T (p. His46Tyr) has been repeatedly observed in persons with permanent neonatal diabetes. In vitro functional studies demonstrated that p. His46Tyr significantly decreased the K-ATP channel sensitivity to inhibition by MgATP and enhanced whole-cell KATP currents [35]. The person from our study was diagnosed with diabetes at the age of 38 years. His current HbA1c was 46 mmol/mol (6.4%) and he was treated with insulin. Multiple family members also displayed diabetes (not neonatal); however, they were not available for genetic testing at the time of the study. We speculate that the functional impact of the histidine to proline substitution is milder than that of other described variants or that this DNA change represents a low-penetrance variant.
Summary
Taken together, the two-step genetic approach represented a better strategy for the molecular genetic investigation of MODY concerning time and financial expenses compared to tNGS performance only. Although the first step (a single-gene investigation) clarified the diabetes aetiology in the majority of cases, tNGS could reveal rare causes of monogenic diabetes and also expose possible limitations of both standard genetic techniques and clinical evaluation. This strategy could be successfully applied to other monogenic disorders with a well-defined clinical phenotype and only a few dominant genetic causes.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Tattersall RB (1974) Mild familial diabetes with dominant inheritance. Q J Med 43:339–357
Froguel P, Vaxillaire M, Sun F, Velho G, Zouali H et al (1992) Close linkage of glucokinase locus on chromosome 7p to early-onset non-insulin-dependent diabetes mellitus. Nature 356:162–164. https://doi.org/10.1038/356162a0
Hattersley AT, Turner RC, Permutt MA, Patel P, Tanizawa Y et al (1992) Linkage of type 2 diabetes to the glucokinase gene. Lancet 339:1307–1310. https://doi.org/10.1016/0140-6736(92)91958-b
Yamagata K, Oda N, Kaisaki PJ, Menzel S, Furuta H et al (1996) Mutations in the hepatocyte nuclear factor-1alpha gene in maturity-onset diabetes of the young (MODY3). Nature 384:455–458. https://doi.org/10.1038/384455a0
Yamagata K, Furuta H, Oda N, Kaisaki PJ, Menzel S et al (1996) Mutations in the hepatocyte nuclear factor-4alpha gene in maturity-onset diabetes of the young (MODY1). Nature 384:458–460. https://doi.org/10.1038/384458a0
Barbetti F, Rapini N, Schiaffini R, Bizzarri C, Cianfarani S (2022) The application of precision medicine in monogenic diabetes. Expert Rev Endocrinol Metab 17:111–129. https://doi.org/10.1080/17446651.2022.2035216
Colclough K, Ellard S, Hattersley A, Patel K (2021) Syndromic monogenic diabetes genes should be tested in patients with a clinical suspicion of MODY. Diabetes. https://doi.org/10.2337/db21-0517
Saint-Martin C, Bouvet D, Bastide M, Chantelot CB, Monogenic Diabetes Study Group of the Societe Francophone du D (2021) Gene panel sequencing of patients with monogenic diabetes brings to light genes typically associated with syndromic presentations. Diabetes. https://doi.org/10.2337/db21-0520
Bellanne-Chantelot C, Clauin S, Chauveau D, Collin P, Daumont M et al (2005) Large genomic rearrangements in the hepatocyte nuclear factor-1beta (TCF2) gene are the most frequent cause of maturity-onset diabetes of the young type 5. Diabetes 54:3126–3132. https://doi.org/10.2337/diabetes.54.11.3126
Murphy R, Turnbull DM, Walker M, Hattersley AT (2008) Clinical features, diagnosis and management of maternally inherited diabetes and deafness (MIDD) associated with the 3243A>G mitochondrial point mutation. Diabet Med 25:383–399. https://doi.org/10.1111/j.1464-5491.2008.02359.x
Sanger F, Nicklen S, Coulson AR (1977) DNA sequencing with chain-terminating inhibitors. Proc Natl Acad Sci USA 74:5463–5467. https://doi.org/10.1073/pnas.74.12.5463
Singh R, Ellard S, Hattersley A, Harries LW (2006) Rapid and sensitive real-time polymerase chain reaction method for detection and quantification of 3243A>G mitochondrial point mutation. J Mol Diagn 8:225–230. https://doi.org/10.2353/jmoldx.2006.050067
Ellard S, Lango Allen H, De Franco E, Flanagan SE, Hysenaj G et al (2013) Improved genetic testing for monogenic diabetes using targeted next-generation sequencing. Diabetologia 56:1958–1963. https://doi.org/10.1007/s00125-013-2962-5
Pearson ER, Liddell WG, Shepherd M, Corrall RJ, Hattersley AT (2000) Sensitivity to sulphonylureas in patients with hepatocyte nuclear factor-1alpha gene mutations: evidence for pharmacogenetics in diabetes. Diabet Med 17:543–545. https://doi.org/10.1046/j.1464-5491.2000.00305.x
Stride A, Shields B, Gill-Carey O, Chakera AJ, Colclough K et al (2014) Cross-sectional and longitudinal studies suggest pharmacological treatment used in patients with glucokinase mutations does not alter glycaemia. Diabetologia 57:54–56. https://doi.org/10.1007/s00125-013-3075-x
Peters JL, Anderson R, Shields B, King S, Hudson M et al (2020) Strategies to identify individuals with monogenic diabetes: results of an economic evaluation. BMJ Open 10:e034716. https://doi.org/10.1136/bmjopen-2019-034716
Pruhova S, Dusatkova P, Sumnik Z, Kolouskova S, Pedersen O et al (2010) Glucokinase diabetes in 103 families from a country-based study in the Czech Republic: geographically restricted distribution of two prevalent GCK mutations. Pediatr Diabetes 11:529–535. https://doi.org/10.1111/j.1399-5448.2010.00646.x
Van der Auwera GA, O'Connor BD (2020) Genomics in the cloud: using Docker, GATK, and WDL in Terra, 1st edn. O'Reilly Media, Newton, Massachusetts, United States
Li H, Durbin R (2009) Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25:1754–1760. https://doi.org/10.1093/bioinformatics/btp324
Desvignes JP, Bartoli M, Delague V, Krahn M, Miltgen M et al (2018) VarAFT: a variant annotation and filtration system for human next generation sequencing data. Nucleic Acids Res 46:W545–W553. https://doi.org/10.1093/nar/gky471
Richards S, Aziz N, Bale S, Bick D, Das S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17:405–424. https://doi.org/10.1038/gim.2015.30
Kopanos C, Tsiolkas V, Kouris A, Chapple CE, Albarca Aguilera M et al (2019) VarSome: the human genomic variant search engine. Bioinformatics 35:1978–1980. https://doi.org/10.1093/bioinformatics/bty897
R Core team (2021) R: A language and environment for statistical computing. https://www.R-project.org/
Passanisi S, Salzano G, Bombaci B, Lombardo F (2021) Clinical and genetic features of maturity-onset diabetes of the young in pediatric patients: a 12-year monocentric experience. Diabetol Metab Syndr 13:96. https://doi.org/10.1186/s13098-021-00716-6
Zmyslowska A, Jakiel P, Gadzalska K, Majos A, Ploszaj T et al (2022) Next- generation sequencing is an effective method for diagnosing patients with different forms of monogenic diabetes. Diabetes Res Clin Pract 183:109154. https://doi.org/10.1016/j.diabres.2021.109154
Shinar Y, Ceccherini I, Rowczenio D, Aksentijevich I, Arostegui J et al (2020) ISSAID/EMQN best practice guidelines for the genetic diagnosis of monogenic autoinflammatory diseases in the next-generation sequencing era. Clin Chem 66:525–536. https://doi.org/10.1093/clinchem/hvaa024
Karacan I, Balamir A, Ugurlu S, Aydin AK, Everest E et al (2019) Diagnostic utility of a targeted next-generation sequencing gene panel in the clinical suspicion of systemic autoinflammatory diseases: a multi-center study. Rheumatol Int 39:911–919. https://doi.org/10.1007/s00296-019-04252-5
Plachy L, Strakova V, Elblova L, Obermannova B, Kolouskova S et al (2019) High prevalence of growth plate gene variants in children with familial short stature treated with GH. J Clin Endocrinol Metab 104:4273–4281. https://doi.org/10.1210/jc.2018-02288
Ploszaj T, Antosik K, Jakiel P, Zmyslowska A, Borowiec M (2021) Screening for extremely rare pathogenic variants of monogenic diabetes using targeted panel sequencing. Endocrine 73:752–757. https://doi.org/10.1007/s12020-021-02753-7
Tatsi EB, Kanaka-Gantenbein C, Scorilas A, Chrousos GP, Sertedaki A (2020) Next generation sequencing targeted gene panel in Greek MODY patients increases diagnostic accuracy. Pediatr Diab 21:28–39. https://doi.org/10.1111/pedi.12931
Shepherd MH, Shields BM, Hudson M, Pearson ER, Hyde C et al (2018) A UK nationwide prospective study of treatment change in MODY: genetic subtype and clinical characteristics predict optimal glycaemic control after discontinuing insulin and metformin. Diabetologia 61:2520–2527. https://doi.org/10.1007/s00125-018-4728-6
Delvecchio M, Salzano G, Bonura C, Cauvin V, Cherubini V et al (2018) Can HbA1c combined with fasting plasma glucose help to assess priority for GCK-MODY vs HNF1A-MODY genetic testing? Acta Diabetol 55:981–983. https://doi.org/10.1007/s00592-018-1179-y
Ellard S, Bulman MP, Frayling TM, Allen LI, Dronsfield MJ et al (1999) Allelic drop-out in exon 2 of the hepatocyte nuclear factor-1alpha gene hinders the identification of mutations in three families with maturity-onset diabetes of the young. Diabetes 48:921–923. https://doi.org/10.2337/diabetes.48.4.921
Ellard S, Bellanne-Chantelot C, Hattersley AT, European Molecular Genetics Quality Network Mg (2008) Best practice guidelines for the molecular genetic diagnosis of maturity-onset diabetes of the young. Diabetologia 51:546-53. https://doi.org/10.1007/s00125-008-0942-y
Girard CA, Shimomura K, Proks P, Absalom N, Castano L et al (2006) Functional analysis of six Kir6.2 (KCNJ11) mutations causing neonatal diabetes. Pflugers Arch 453:323–332. https://doi.org/10.1007/s00424-006-0112-3
Acknowledgements
We would like to acknowledge the Czech diabetologists who sent samples from people with diabetes for molecular genetic testing. Michael Svaton, Ph.D. (Department of Paediatric Haematology and Oncology, 2nd Faculty of Medicine, Charles University, Prague, Czech Republic) helped with bioinformatics at the beginning of the project. Kevin Colclough, Ph.D. (Medical School, University of Exeter, Exeter, United Kingdom) is thanked for providing positive samples carrying the m.3243A>G variant in the MT-TL1 gene in the mitochondrial DNA and Prof. Ondrej Cinek, Ph.D. (Department of Paediatrics, 2nd Faculty of Medicine, Charles University, Prague, Czech Republic) assisted with bioinformatics evaluation of heteroplasmy of the respective mitochondrial variant.
Funding
Supported by Ministry of Health of the Czech Republic grant number NV18-01–00078. All rights reserved.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants
This study was approved by the institutional Ethics Committee of the 2nd Faculty of Medicine, Charles University and University Hospital Motol, Prague, the Czech Republic and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
All study participants or their legal guardians have signed the informed consent with the genetic testing.
Additional information
Managed By Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dusatkova, P., Pavlikova, M., Elblova, L. et al. Search for a time- and cost-saving genetic testing strategy for maturity-onset diabetes of the young. Acta Diabetol 59, 1169–1178 (2022). https://doi.org/10.1007/s00592-022-01915-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-022-01915-x