Abstract
Purpose
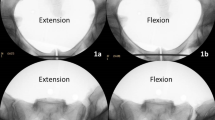
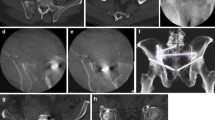
Reduction of AO/OTA 61-B2.3 (APC2) pelvic fractures is challenging in the setting of anterior ring comminution. The anterior ring is visually much simpler to evaluate for flexion or extension hemipelvis deformity than the posterior ring, except in the setting of comminution, necessitating some other visual reference to judge hemipelvis reduction. We sought to test whether pelvic inlet and outlet fluoroscopy of the contours of the sacroiliac joint could be used in isolation to judge hemipelvis flexion or extension.
Methods
Symphyseal and anterior SIJ ligaments were cut (6 cadaveric pelvis). The symphysis was held malreduced to produce one centimeter flexion and extension deformity: 1 cm was selected to mimic a maximum clinical scenario. The SIJ was assessed using inlet and outlet fluoroscopy. The scaled width of the SIJ was assessed at the joint apertures and midjoint on both inlet and outlet views. Joint widths in flexion and extension were compared against joint widths measured on the reduced SIJ using paired t-tests.
Results
There was no statistical difference in the superior (p = 0.227, 0.675), middle (p = 0.203, 0.693), and inferior (p = 0.232, 0.961) SIJ widths between hemipelvis flexion or extension models against reduced SIJ on outlet views. There was no statistical difference in the anterior (p = 0.731, 0.662), middle (p = 0.257, 0.655), and posterior (p = 0.657, 0.363) SIJ widths between flexion or extension models against reduced SIJ on inlet views.
Conclusion
Inspection of SIJ width on inlet and outlet fluoroscopy cannot detect up to one centimeter of hemipelvis flexion or extension malreduction in the setting of AO/OTA 61-B2.3 (APC2) pelvic fractures with complex anterior injuries.


Similar content being viewed by others
References
Lindsay A, Tornetta P, Diwan A, Templeman D (2016) Is closed reduction and percutaneous fixation of unstable posterior ring injuries as accurate as open reduction and internal fixation? J Orthop Trauma 30:29–33. https://doi.org/10.1097/BOT.0000000000000418
Tornetta P, Matta JM (1996) Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop 329:186–193
Matta JM, Saucedo T (1989) Internal fixation of pelvic ring fractures. Clin Orthop. https://doi.org/10.1097/00003086-198905000-00009
Templeman D, Goulet J, Duwelius PJ et al (1996) Internal fixation of displaced fractures of the sacrum. Clin Orthop 329:180–185
Verbeek DO, Routt ML (2018) High-energy pelvic ring disruptions with complete posterior instability: contemporary reduction and fixation strategies. J Bone Jt Surg 100:1704–1712. https://doi.org/10.2106/JBJS.17.01289
Dujardin FH, Hossenbaccus M, Duparc F et al (1998) Long-term functional prognosis of posterior injuries in high-energy pelvic disruption. J Orthop Trauma 12:145
Letournel E (1981) Surgical fixation of displaced pelvic fractures and dislocations of the symphysis pubis (excluding acetabular fractures) (author’s transl). Rev Chir Orthop Reparatrice Appar Mot 67:771–782
McLaren AC, Rorabeck CH, Halpenny J (1990) Long-term pain and disability in relation to residual deformity after displaced pelvic ring fractures. Can J Surg J Can Chir 33:492–494
Majeed SA (1990) External fixation of the injured pelvis. The functional outcome. J Bone Joint Surg Br 72:612–614
Semba RT, Yasukawa K, Gustilo RB (1983) Critical analysis of results of 53 Malgaigne fractures of the pelvis. J Trauma 23:535–537
Tile M (1988) Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br 70:1–12
Slätis P, Huittinen VM (1972) Double vertical fractures of the pelvis. A report on 163 patients. Acta Chir Scand 138:799–807
Simpson LA, Waddell JP, Leighton RK et al (1987) Anterior approach and stabilization of the disrupted sacroiliac joint. J Trauma 27:1332–1339
Gardner MJ, Routt MC Jr (2011) Transiliac–transsacral screws for posterior pelvic stabilization. J Orthop Trauma 25:378–384
Routt ML, Kregor PJ, Simonian PT, Mayo KA (1995) Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma 9:207–214
Giannoudis PV, Tzioupis CC, Pape H-C, Roberts CS (2007) Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br 89:145–154. https://doi.org/10.1302/0301-620X.89B2.18551
Avilucea FR, Whiting PS, Mir H (2016) Posterior fixation of APC-2 pelvic ring injuries decreases rates of anterior plate failure and malunion. J Bone Jt Surg 98:944–951. https://doi.org/10.2106/JBJS.15.00723
Avilucea FR, Archdeacon MT, Collinge CA et al (2018) Fixation strategy using sequential intraoperative examination under anesthesia for unstable lateral compression pelvic ring injuries reliably predicts union with minimal displacement. J Bone Jt Surg 100:1503–1508. https://doi.org/10.2106/JBJS.17.01650
Takeba J, Umakoshi K, Kikuchi S et al (2018) Accuracy of screw fixation using the O-arm® and StealthStation® navigation system for unstable pelvic ring fractures. Eur J Orthop Surg Traumatol Orthop Traumatol 28:431–438. https://doi.org/10.1007/s00590-017-2075-9
Ghisla S, Napoli F, Lehoczky G et al (2018) Posterior pelvic ring fractures: Intraoperative 3D-CT guided navigation for accurate positioning of sacro-iliac screws. Orthop Traumatol Surg Res 104:1063–1067. https://doi.org/10.1016/j.otsr.2018.07.006
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no further conflicts of interest relevant to this work.
Ethical approval
The enclosed work was performed in compliance with modern ethical standards of publishing. The work was performed unfunded. The authors received no funding for the submitted work. [Corresponding/senior author] serves in a volunteer manner as a section editor at the Journal of Orthopaedic Trauma. The enclosed research was performed after ethical approval was obtained from the local institutions IRB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Working, Z.M., El Naga, A.N., Hoogervorst, P. et al. Fluoroscopic images of the sacroiliac joint alone are unable to identify simulated flexion or extension malreduction of the anterior pelvic ring in AO/OTA 61-B2.3 pelvic injuries. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-03841-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-03841-w