Abstract
Purpose
Medial knee osteoarthritis can be treated with medial open wedge high tibial osteotomy (OWHTO). We sought to investigate osseous consolidation of the osteotomy with and without autologous bone grafts (ABG) to detect possible benefits of ABG in osseous healing and functional outcome.
Methods
In this prospective study, patients without graft transplantation were compared to those receiving ABG after medial OWHTO. They were followed up 6 weeks, 12 weeks, 6 months and 12 months postoperatively. Radiographic progress of consolidation, clinical scores, contrast-enhanced ultrasound (CEUS) and dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) were assessed at each appointment.
Results
A total of 35 patients were enrolled, 20 without and 15 with graft transplantation. Radiologic evaluation showed a significantly earlier consolidation of the osteotomy gaps (p = 0.012) in patients with ABG, resulting in a significantly higher rate of consolidation 12 months after surgery (60% without bone graft vs. 100% with bone graft, p = 0.006). At 6 weeks as well as 6-month follow-up, a tendency of earlier consolidation with ABG was apparent, but not statistically significant (6 weeks: 50% vs. 80%, p = 0.089; 6 months: 30% vs. 60%, p = 0.097). CEUS and DCE-MRI showed physiological perfusion of the osteotomy gaps in both groups. A tendency to better function and less pain in patients with ABG was recognizable.
Conclusion
In our study, autologous bone grafting evocated earlier osseous consolidation after medial OWHTO and showed a tendency to a better functional outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis affected 263 million people globally in 2017 [1]. In combination with genu varum deformities, the risk of knee osteoarthritis can even be aggravated [2]. The open wedge high tibial osteotomy (OWHTO) is a well-accepted treatment option for osteoarthritis with satisfying short- and long-term results in elderly as well as in young patients [3]. Advantages of OWHTO are the preservation of bone stock, an easy bone exposure and correction during surgery as there is no need to involve the fibula [4]. On the other hand, there are some possible and severe complications, e.g. loss of correction, delayed bone union or even non-union [4]. To potentially avoid these disadvantages, autologous bone grafts (ABG), allografts or synthetic bone grafts can be used to fill the osteotomy gap [5]. Previous studies reported better results of ABG compared to other graft types [5]. Nevertheless, bone grafting can potentially lead to pain and complications at the donor location e.g. infections, fractures and sensory disorders [4]. Therefore, grafting with ABG should be performed after careful considerations. Most studies could not prove an accelerated consolidation or better knee function by using a graft [4, 6, 7]. However, a prospective randomized study reported that using a graft expedites the radiographic healing of the osteotomy gap, but no advantages regarding knee function were found [8].
Contrast-enhanced ultrasound (CEUS) and dynamic magnetic resonance imaging (DCE-MRI) were used in previous trials to examine the perfusion of bone healing in fractures, non-unions and septic non-unions [9,10,11,12]. In this trial, these two modalities were integrated to control physiological consolidation beyond common x-rays and to secure the comparability of both groups as well as detecting risk factors like infections and impaired perfusion.
The aim of this prospective study was to evaluate the use of ABG in osteotomy gaps of medial OWHTO as well as the influence of grafting on the postoperative knee function.
Materials and methods
Patients
Between 2015 and 2018, a total of 41 patients with medial knee osteoarthritis undergoing medial OWHTO at our hospital were included. Inclusion criteria were a minimum age of 18 years, varus deformity with medial knee osteoarthritis and written informed consent.
Exclusion criteria were a follow-up period less than one year, clinical infection, contrast agent intolerance (SonoVue® [Bracco, Milan, Italy] or Dotarem® [Guerbet, Villepint, France]) as well as respiratory insufficiency and recent myocardial infarction.
All patients with planned OWHTO surgery were included, regardless of the severity of the varus alignment or risk factors for impaired consolidation.
This study was conducted in accordance with the current declaration of Helsinki and was approved by the local Ethics Committee (S-033/2014). All patients agreed with the study protocol and gave their written informed consent.
Out of 41 patients who met the inclusion criteria, six patients had to be excluded: Five were lost to follow-up and one was excluded because of a clinical infection (ABG group). The remaining 35 patients were divided into two groups after surgery regarding the use of graft transplantation: Twenty patients did not receive a graft (group A), whereas in fifteen patients autologous bone grafting was performed (group B). The decision of grafting was made by the surgeon intraoperatively considering the osteotomy gap size as well as existing risk factors for impaired bone healing. There were no other criteria regarding the use or origin of the grafts.
No significant differences between groups were seen in age (42 (IQR: 31–49) and 44 (IQR: 27–47) years in group A and B), sex (35% vs 47% female), BMI (27.2 (IQR: 21.7–31.4) and 28.9 (IQR: 23.8–31.4) kg/m2 in group A and B) or medical history. Surgeons decided to use ABG transplantation more often in smokers (Table 1).
Differences in surgical technique between groups
During medial OWHTO, group B received a gap filling with ABG from different sampling points including the ipsilateral proximal tibia or iliac crest. Both groups received the TomoFix® Medial High Tibial Plate (DePuy Synthes, Switzerland).
Postoperative assessment
Postoperatively, after increasing weight-bearing stepwise, most patients reached full load after 4 to 6 weeks. Range of knee motion was not limited. Physiotherapy and lymph drainage 2 to 3 times a week were recommended.
Follow-up appointments were performed at 6 weeks, 12 weeks, 6 months and 12 months after surgery. At each appointment, patients were asked to answer questionnaires including the Knee Society Score (KSS), the Lysholm Knee Score (LKS) and the SF12 [13,14,15]. Radiographic evaluation as well as a physical examination was performed by an experienced senior orthopedic surgeon.
Radiographic evaluation
Axis correction was measured with the hip-knee-ankle (HKA) angle before and after surgery on a full-length x-ray of the lower limb in anterior–posterior view. Furthermore, at each postoperative appointment, anteroposterior as well as lateral x-rays of the knee were performed. Those anteroposterior x-ray images were evaluated according to the radiologic index of Brosset et al. [16] (see Fig. 1).
Radiographic Evaluation of an anteroposterior x-ray of a patients’ knee three days postoperatively. A triangle form of the osteotomy gap was divided into fifths by vertical lines, counting from the lateral to the medial cortex, to display the progress of consolidation. A fifth was rated as successfully consolidated when more than 50% of it was filled with bone
Specific consolidation aims were determined at the following appointments: 3 fifths filled after 6 weeks, 4 fifths with radiologic bone healing 12 weeks after surgery and all fifths should display consolidation 6 and 12 months postoperatively. Evaluation was performed by an experienced senior orthopedic and trauma consultant. A slope for each patients’ consolidation was created with a linear regression, using the slopes’ gradient as an indicator for the acceleration of consolidation [17]. GNU Image Manipulation Program (Spencer Kimball, Peter Mattis and GIMP development team) was used for analysis.
Imaging evaluation
To control physiological bone healing and perfusion, CEUS and DCE-MRI examinations and evaluations of the osteotomy gap were implemented, following established protocols as used previously [10,11,12].
CEUS of the osteotomy gap was performed at every appointment. Therefore, we used established parameters: peak enhancement (PE in arbitrary units [a.u.]) as the maximum signal intensity of the enhancement curve, wash-in rate (WiR [a.u.]) as the steepest slope of the curve as well as wash-in perfusion index (WiPi [a.u.]) as the ratio between wash-in area under the curve and rise time [12]. CEUS examinations were assessed by the dedicated quantification software VueBox (Bracco Imaging, Milan, Italy).
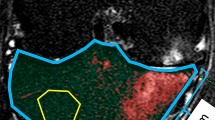
DCE-MRI evaluated bone perfusion of the osteotomy gap 12 weeks postoperatively. Images of the DCE-MRI were postprocessed by a dedicated quantification software (Tissue4D, Siemens Healthcare, Erlangen, Germany), and the ratios between the initial area under the enhancement curve of the osteotomy gap relative to the muscle tissue were assessed.
An example of an examination and evaluation of CEUS is illustrated in Fig. 2 and of DCE-MRI in Fig. 3.
Contrast-enhanced ultrasound (CEUS) examination and evaluation of an osteotomy gap (patient without ABG). Upper part: sonography of the osteotomy gap with the specific contrast-enhanced cadence mode (left) and the standard b-mode (right). Lower part: evaluation over time of both regions of interests (ROI) with the dedicated quantification software VueBox (Bracco Imaging). Green: ROI 1 in the osteotomy gap. Yellow: ROI 2 in adjacent tissue without fascia or vessels (colour figure online)
Dynamic magnetic resonance imaging (DCE-MRI) examination and evaluation of an osteotomy gap (patient without ABG). Left: DCE-MRI of the osteotomy gap. Right: evaluation over time of both regions of interests (ROI) with the dedicated quantification software Tissue4D (Siemens Healtcare). Red: ROI 1 in the osteotomy gap. Green: ROI 2 in adjacent muscle tissue (colour figure online)
Data analysis
Statistical analysis was performed using Stata statistical software (version 16.1, StataCorp, United States). Data were described by using means and standard deviations or medians and interquartile ranges (IQR), as appropriate. Microsoft® Excel® for Microsoft 365 MSO (16.0.14326.21008) was used to generate the graphs.
Because of the sample size of each group, we assumed data not to be normal distributed, so the Wilcoxon sign rank test was used to compare both groups. Categorical data were analyzed by using the Fisher exact test. A p-value < 0.05 was considered to be statistically significant.
A binomial logistic regression was performed to determine the effect of the gap size and age on the consolidation.
A priori sample size calculation
An a priori sample size estimation was conducted. G*Power 3 [18] was used for all sample size estimations. Considering a difference of 1 fifths in consolidation with a standard deviation of 0.8 fifths between the two groups as a clinically relevant change, an effect size (Cohen’s d) of 1.25 can be assumed. To detect a significant difference between the mean of two independent groups, a sample size of 15 subjects per group is needed to achieve a power of > 90%. Recruitment was continued until at least 15 subjects in each group successfully finished one year of follow-up.
Results
Radiographic evaluation
Radiologically, 97.1% of all osteotomy gaps consolidated within the one-year follow-up. Only one patient without ABG developed a radiographic non-union without clinical symptoms. Radiologic evaluation showed a significantly better consolidation of the osteotomy gaps in patients with ABG 12 months after surgery: Only 60% of group A had all fifths filled with osseous tissue compared to 100% in group B (p = 0.006). Regarding the x-ray evaluation at 6 weeks and 6 months postoperatively, a tendency of faster bone healing with ABG was apparent but could not be proven with statistical significance (6 weeks (3 fifths filled): 50% in group A vs. 80% in group B, p = 0.089; 6 months (all fifths filled): 30% vs. 60%, p = 0.097) (Table 2). While patients without ABG had in general a slower consolidation in radiographic imaging, patients with graft transplantation experienced rapid progress of bone consolidation resulting in a steeper slope. Concerning the gradient of the consolidation slopes over time, a significantly increased bone healing of the osteotomy gaps with graft transplantation could be detected (p = 0.012).
The pre- and postoperatively measured HKA angles showed a tendency that patients with larger correction angles received ABG (6.0 vs. 8.0 degrees; p = 0.053).
Using the binominal logistic regression, we found a non-significant correlation between the gap size and those from Group A who did not reach the consolidation goal after one year with odds ratio (OR) = 0.733 and p = 0.070. After adjustment for age, the OR was 0.699 with p = 0.052.
Imaging evaluation
CEUS and DCE-MRI did not show any significant differences regarding the perfusion of the osteotomy gaps between the two groups as well as physiological bone healing without indication of an infection or impaired perfusion (p > 0.05 for all parameters).
Functional assessment
There were no significant differences regarding the functional tests of patients with or without grafting, but there was a tendency of better function and less pain in patients receiving ABG (p = 0.290 after one year) (Fig. 4). Part 1 of the KSS is the knee score section and includes range of motion, stability, pain, alignment, flexion contractures and extension lag.
Part 2 of the KSS is the functional score section and includes walking, stair climbing as well as the necessity and type of walking aids. In Part 2, patients receiving ABG also showed a tendency of better function without significant results (p = 0.170 after one year) (Fig. 5).
Concerning the LKS, group A scored a median of 65.5 points (IQR: 48.5–74) and group B of 43 points (IQR: 30–66) preoperatively (p = 0.071). One year after surgery, the median of group A was 72 points (IQR: 71–84) and the median of group B 89 points (IQR: 71–95) (p = 0.640).
In the mental part of the SF12, there were no significant differences between patients with or without graft transplantation before and one year after surgery (preoperative: p = 0.61; 1 year postoperative: p = 0.46).
Regarding the physical part of the SF12, group A scored preoperatively a median of 39.5 points (IQR: 29.0–46.2) and group B of 31.6 points (IQR: 26.9–38.8) (p = 0.170). At the one-year follow-up, group B reached slightly better results with a median of 48.4 points (IQR: 38.9–54.5) than group A with 43.8 points (IQR: 37.6–51.7) (p = 0.640).
Discussion
The most important finding of the present study was that bone grafting resulted in an earlier consolidation of the osteotomy gap. Moreover, grafting seemed to increase the complete osseous union of the gap and showed a tendency to a better functional outcome after one year.
Among others, grafts were typically used to fill open wedge osteotomy gaps to stabilize the osteotomy and to secure bone consolidation [4]. Nowadays, it is controversially discussed when to perform grafting as there are several studies with good results without grafts [19,20,21].
Zorzi et al. [4] conducted a randomized, controlled study to investigate the advantages of using grafts. In this study with 46 patients, they discovered a complete consolidation after 12 weeks regardless of grafting. No statistical differences between the two groups according to the consolidation of the osteotomy gap were evident. However, no consolidation status over time was contained and no evaluation tools like the triangle tool by Brosset et al. [16] were used to assess consolidation semi-objectively. In line, a systematic review of Slevin et al. [7] found the same consolidation rates and no clinically significant advantage of using bone void fillers. Likewise, no chronological sequences of consolidation rates were evaluated. Similar, the meta-analysis of Han et al. [6] reported the same time for consolidation, union rate or complications independent of grafting. Furthermore, Silboni et al. [22] also did not recommend the use of grafts in OWHTO with locking plates or corrections smaller than 10° because they did not find any statistically significant differences between both groups.
In contrast to these studies, Fucentese et al. [8] observed in a prospective, randomized study an increased bone healing rate in patients with ABG 3 and 12 months after surgery. Performing a computed tomography, they found that 91.5% of the osseous gaps were healed at one-year follow-up in patients with graft compared to 59.1% in patients without bone void fillers. These results were confirmed by Ulucaköy et al. [23]. In their study with 25 patients, a faster healing of the osteotomy gap in patients with graft and a prolonged consolidation time in larger gaps were observed. This is in line with our data that also indicated an accelerated bone union in patients with bone transplantation, especially after one year (100% vs. 60%).
Furthermore, Pornrattanamaneewong et al. [24] assumed that a remaining medial gap of larger than 5 mm could lead to a higher risk for proximal tibia fractures when there is a need to remove the osteosynthesis. Our results show that a completely filled gap is more likely achieved with ABG and therefore might hold future benefits if a removal of the osteosynthesis is necessary, for example due to implant-related pain or implantation of a knee endoprosthesis.
Looking at the functional scores, Fucentese et al. [8] and Ulucaköy et al. [23] could not find significant differences between patients receiving grafts and patients without bone transplantation. Therefore, both did not recommend the routine use of grafts. We also detected no statistically significant differences in the functional scores, but we assume the data not to be statistically significant due to the limited number of patients. Nevertheless, we found a clear tendency toward better functional results with grafts. 6 weeks postoperative, patients with graft transplantation achieved lower functional scores, possibly caused by pain of the ipsilateral donor location. These patients with bone grafts had initially worse values in both parts of the KSS and in the LKS before surgery but ended up with higher values than patients without grafting one year later.
Additionally, ABG were used significantly more often in patients with nicotine abuse. According to the operation reports, the surgeons often decided intraoperatively to use bone grafting depending on their patients’ smoking status. Although smoking has an inhibiting effect on bone healing and can lead to delayed bone union, non-union [25, 26] or to a subjective worse outcome [27], the osteotomy gaps consolidated significantly faster with the use of bone grafts. These patients also had better functional outcomes compared to the group without ABG and less smokers. Aryee et al. [28] also suggested to use ABG in patients with heavy smoking or other risk factors like obesity or a large opening gap with more than 10 mm. Silboni et al. [22] agreed with those recommendations without regard to nicotine abuse but to lateral cortex hinge fractures.
In this study, CEUS and DCE-MRI were used as control examinations of physiological osseous healing and did not show any significant differences regarding graft transplantation. Compared with the results of previous studies published by Fischer et al. [9,10,11], a normal perfusion for bone healing processes could be detected. Accordingly, the endpoint of bone healing could be investigated specifically regarding ABG while controlling for other potentially confounding risk factors such as infection or impaired perfusion.
Some findings of this study did not reach statistical significance, which may be due to the small sample size and different donor locations. Furthermore, these results cannot be generalized for a larger population due to the limited number of patients in our trial. More well-powered randomized controlled trials are needed to differentiate the impact of the donor site on functional results. Another limitation of this study is the evaluation of consolidation only by x-ray. Although the radiographic assessment was highly standardized, the risk of the appearance of the osteotomy gap, the bone graft or the position of the ABG in the osteotomy gap influencing the corresponding results cannot be fully excluded. For a more accurate evaluation of consolidation, a computed tomography would be necessary, but for reasons of radiation protection cannot be performed four times within a year for research purposes. Thus, CEUS and DCE-MRI were performed to gather more indications for a physiological bone healing process.
In conclusion, we assume that autologous bone grafting induces earlier osseous consolidation after medial OWHTO. We see a tendency toward better functional results without reaching significance. ABG was used significantly more often in patients with nicotine abuse in this study and showed good 1-year outcomes. We hypothesize that these high-risk patients may benefit from complete and timely consolidation. Thus the use of ABG may be useful in those cases.
References
James SL et al (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159):1789–1858
Brouwer GM et al (2007) Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum 56(4):1204–1211
Jin C et al (2020) Survival and risk factor analysis of medial open wedge high tibial osteotomy for unicompartment knee osteoarthritis. Arthroscopy 36(2):535–543
Zorzi AR et al (2011) Opening-wedge high tibial osteotomy with and without bone graft. Artif Organs 35(3):301–307
Lash NJ et al (2015) Bone grafts and bone substitutes for opening-wedge osteotomies of the knee: a systematic review. Arthroscopy 31(4):720–730
Han JH et al (2015) Is bone grafting necessary in opening wedge high tibial osteotomy? A meta-analysis of radiological outcomes. Knee Surg Relat Res 27(4):207–220
Slevin O et al (2016) The role of bone void fillers in medial opening wedge high tibial osteotomy: a systematic review. Knee Surg Sports Traumatol Arthrosc 24(11):3584–3598
Fucentese SF et al (2019) Bone autografting in medial open wedge high tibial osteotomy results in improved osseous gap healing on computed tomography, but no functional advantage: a prospective, randomised, controlled trial. Knee Surg Sports Traumatol Arthrosc 27(9):2951–2957
Doll J et al (2019) The AMANDUS project-advanced microperfusion assessed non-union diagnostics with contrast-enhanced ultrasound (CEUS) for the detection of infected lower extremity non-unions. Ultrasound Med Biol 45(9):2281–2288
Fischer C et al (2020) Contrast-enhanced ultrasound (CEUS) identifies perfusion differences between tibial fracture unions and non-unions. Ultraschall Med 41(01):44–51
Fischer C et al (2016) Dynamic contrast-enhanced sonography and dynamic contrast-enhanced magnetic resonance imaging for preoperative diagnosis of infected nonunions. J Ultrasound Med 35(5):933–942
Fischer C et al (2020) Contrast-enhanced ultrasound for musculoskeletal applications: a world federation for ultrasound in medicine and biology position paper. Ultrasound Med Biol 46(6):1279–1295
Briggs KK et al (2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 37(5):890–897
Asif S, Choon DS (2005) Midterm results of cemented Press Fit Condylar Sigma total knee arthroplasty system. J Orthop Surg (Hong Kong) 13(3):280–284
Ware J Jr, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Brosset T et al (2011) Opening wedge high tibial osteotomy performed without filling the defect but with locking plate fixation (TomoFix™) and early weight-bearing: prospective evaluation of bone union, precision and maintenance of correction in 51 cases. Orthop Traumatol Surg Res 97(7):705–711
Hammer M et al (2020) Functional mobility recovery predicts readmission to the surgical intensive care unit. Intensive Care Med 46(5):1054–1056
Faul F et al (2007) G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39(2):175–191
Kolb W et al (2009) Opening-wedge high tibial osteotomy with a locked low-profile plate. J Bone Joint Surg Am 91(11):2581–2588
Staubli AE, Jacob HA (2010) Evolution of open-wedge high-tibial osteotomy: experience with a special angular stable device for internal fixation without interposition material. Int Orthop 34(2):167–172
El-Assal MA et al (2010) Opening-wedge high tibial osteotomy without bone graft. Knee Surg Sports Traumatol Arthrosc 18(7):961–966
Siboni R et al (2018) Opening-wedge high tibial osteotomy without bone grafting in severe varus osteoarthritic knee. Rate and risk factors of non-union in 41 cases. Orthop Traumatol Surg Res 104(4):473–476
Ulucaköy C et al (2020) Is iliac autogenous graft augmentation in medial open wedge high tibial osteotomies superior to no augmentation in terms of bone healing? Joint Dis Relat Surg 31(2):360
Pornrattanamaneewong C et al (2012) A retrospective analysis of medial opening wedge high tibial osteotomy for varus osteoarthritic knee. Indian J Orthop 46(4):455–461
Castillo RC et al (2005) Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma 19(3):151–157
Kallala R et al (2013) The in vitro and in vivo effects of nicotine on bone, bone cells and fracture repair. Expert Opin Drug Saf 12(2):209–233
Floerkemeier S et al (2014) Does obesity and nicotine abuse influence the outcome and complication rate after open-wedge high tibial osteotomy? A retrospective evaluation of five hundred and thirty three patients. Int Orthop 38(1):55–60
Aryee S et al (2008) Do we need synthetic osteotomy augmentation materials for opening-wedge high tibial osteotomy. Biomaterials 29(26):3497–3502
Acknowledgements
The successful patient acquisition could be performed thanks to the cooperation with the Sports Orthopaedics Department (Center for Orthopaedics, Trauma Surgery and Spinal Cord Injury, Heidelberg University Hospital).
Funding
Open Access funding enabled and organized by Projekt DEAL. There was no external funding provided for this study. Material and devices were used of the Heidelberg University Hospital.
Author information
Authors and Affiliations
Contributions
EB participated in statistical analysis, in interpretation and design and developed the final manuscript. JB performed statistical analysis, designed figures and tables and drafted the manuscript. JD helped to draft the manuscript and its design. FB conceived of the study, performed study coordination as well as patient and data acquisition. GS revised the manuscript critically. CF conceived of the study, participated in its design, coordination and interpretation and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was conducted in accordance with the current declaration of Helsinki and was approved by the local Ethics Committee (S-033/2014).
Informed consent
All patients participated voluntarily, agreed with the study protocol and gave their written informed consent before any study relevant procedures began.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bodenbeck, EM., Böpple, J.C., Doll, J. et al. Earlier consolidation and improved knee function of medial open wedge high tibial osteotomy with autologous bone graft. Eur J Orthop Surg Traumatol 34, 371–378 (2024). https://doi.org/10.1007/s00590-023-03656-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03656-1