Abstract
Purpose
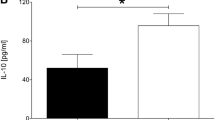
The overwhelming inflammatory response plays a critical role in the secondary injury cascade of traumatic spinal cord injury (tSCI). The systemic immune inflammatory index (SII) and systemic inflammatory response index (SIRI) are two novel inflammatory biomarkers. The SII was calculated based on lymphocyte, neutrophil, and platelet counts, while the SIRI was calculated based on lymphocyte, neutrophil, and monocyte counts. Their prognostic value in patients with tSCI remains unclear.
Methods
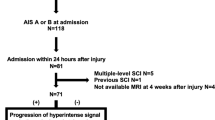
Patients with tSCI admitted within 24 h of trauma were retrospectively and consecutively enrolled. Peripheral blood samples were collected on admission. The primary outcome was American Spinal Injury Association Impairment Scale (AIS) grade conversion at discharge. Multivariable logistic regression analysis was performed to determine the relationship between SII and SIRI and AIS grade conversion. We performed receiver operating characteristic curve (ROC) analysis to assess the discriminative ability of SII, and SIRI in predicting AIS grade conversion.
Results
Among 280 included patients, 77 (27.5%) had improved AIS grade conversion at discharge. After adjustment for confounders, SII was independently associated with AIS grade conversion (per SD, odds ratio [OR], 0.68; 95% confidence interval [CI] 0.47–0.98, p = 0.040), while the association between SIRI and AIS grade conversion was insignificant (per 1 SD, OR, 0.77; 95% CI 0.55–1.08, p = 0.130). The ROC analysis revealed that the SII had the best predictive value for AIS grade conversion (area under curve: 0.608, 95% CI 0.536–0.678).
Conclusions
Increased SII was independently associated with a decreased likelihood of improved AIS grade conversion.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Ofori-Asenso R (2019) Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(1):56–87. https://doi.org/10.1016/s1474-4422(18)30415-0
Spiess MR, Müller RM, Rupp R et al (2009) Conversion in ASIA impairment scale during the first year after traumatic spinal cord injury. J Neurotrauma 26(11):2027–2036. https://doi.org/10.1089/neu.2008.0760
Khorasanizadeh M, Yousefifard M, Eskian M et al (2019) Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine. https://doi.org/10.3171/2018.10.Spine18802
Ahuja CS, Wilson JR, Nori S et al (2017) Traumatic spinal cord injury. Nat Rev Dis Primers 3:17018. https://doi.org/10.1038/nrdp.2017.18
Hellenbrand DJ, Quinn CM, Piper ZJ et al (2021) Inflammation after spinal cord injury: a review of the critical timeline of signaling cues and cellular infiltration. J Neuroinflammation 18(1):284. https://doi.org/10.1186/s12974-021-02337-2
Faden AI, Wu J, Stoica BA, Loane DJ (2016) Progressive inflammation-mediated neurodegeneration after traumatic brain or spinal cord injury. Br J Pharmacol 173(4):681–691. https://doi.org/10.1111/bph.13179
Orr MB, Gensel JC (2018) Spinal cord injury scarring and inflammation: therapies targeting glial and inflammatory responses. Neurotherapeutics 15(3):541–553. https://doi.org/10.1007/s13311-018-0631-6
Yang YL, Wu CH, Hsu PF et al (2020) Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest 50(5):e13230. https://doi.org/10.1111/eci.13230
Jin Z, Wu Q, Chen S et al (2021) The associations of two novel inflammation indexes, SII and SIRI with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 individuals. J Inflamm Res 14:131–140. https://doi.org/10.2147/jir.S283835
Wang C, Yu X, Wang T, Ding M, Ran L (2023) D-dimer/fibrinogen ratio for the prediction of deep venous thrombosis after traumatic spinal cord injury. Spinal Cord. https://doi.org/10.1038/s41393-023-00905-2
Wang C, Yu X, Wang T et al (2023) Association between neutrophil percentage-to-albumin ratio and pneumonia in patients with traumatic spinal cord injury. Spinal Cord 61(2):106–110. https://doi.org/10.1038/s41393-022-00844-4
Kobayakawa K, Kumamaru H, Saiwai H et al (2014) Acute hyperglycemia impairs functional improvement after spinal cord injury in mice and humans. Sci Transl Med 6(256):256ra137. https://doi.org/10.1126/scitranslmed.3009430
Wang C, Cui T, Li S et al (2023) The change in fibrinogen is associated with outcome in patients with acute ischemic stroke treated with endovascular thrombectomy. Neurocrit Care. https://doi.org/10.1007/s12028-023-01768-4
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3):837–845
Jogia T, Lübstorf T, Jacobson E et al (2021) Prognostic value of early leukocyte fluctuations for recovery from traumatic spinal cord injury. Clin Transl Med 11(1):e272. https://doi.org/10.1002/ctm2.272
Fleming JC, Norenberg MD, Ramsay DA et al (2006) The cellular inflammatory response in human spinal cords after injury. Brain 129(Pt 12):3249–3269. https://doi.org/10.1093/brain/awl296
Noble LJ, Donovan F, Igarashi T, Goussev S, Werb Z (2002) Matrix metalloproteinases limit functional recovery after spinal cord injury by modulation of early vascular events. J Neurosci 22(17):7526–7535. https://doi.org/10.1523/jneurosci.22-17-07526.2002
Zrzavy T, Schwaiger C, Wimmer I et al (2021) Acute and non-resolving inflammation associate with oxidative injury after human spinal cord injury. Brain 144(1):144–161. https://doi.org/10.1093/brain/awaa360
Ankeny DP, Popovich PG (2009) Mechanisms and implications of adaptive immune responses after traumatic spinal cord injury. Neuroscience 158(3):1112–1121. https://doi.org/10.1016/j.neuroscience.2008.07.001
Moalem G, Gdalyahu A, Shani Y et al (2000) Production of neurotrophins by activated T cells: implications for neuroprotective autoimmunity. J Autoimmun 15(3):331–345. https://doi.org/10.1006/jaut.2000.0441
Jones TB (2014) Lymphocytes and autoimmunity after spinal cord injury. Exp Neurol 258:78–90. https://doi.org/10.1016/j.expneurol.2014.03.003
Leister I, Linde LD, Vo AK et al (2021) Routine blood chemistry predicts functional recovery after traumatic spinal cord injury: a post hoc analysis. Neurorehabil Neural Repair 35(4):321–333. https://doi.org/10.1177/1545968321992328
Rawish E, Nording H, Münte T, Langer HF (2020) Platelets as mediators of neuroinflammation and thrombosis. Front Immunol 11:548631. https://doi.org/10.3389/fimmu.2020.548631
Thomas MR, Storey RF (2015) The role of platelets in inflammation. Thromb Haemost 114(3):449–458. https://doi.org/10.1160/th14-12-1067
May AE, Langer H, Seizer P et al (2007) Platelet-leukocyte interactions in inflammation and atherothrombosis. Semin Thromb Hemost 33(2):123–127. https://doi.org/10.1055/s-2007-969023
Gensel JC, Zhang B (2015) Macrophage activation and its role in repair and pathology after spinal cord injury. Brain Res 1619:1–11. https://doi.org/10.1016/j.brainres.2014.12.045
Shechter R, London A, Varol C et al (2009) Infiltrating blood-derived macrophages are vital cells playing an anti-inflammatory role in recovery from spinal cord injury in mice. PLoS Med 6(7):e1000113. https://doi.org/10.1371/journal.pmed.1000113
Greenhalgh AD, Zarruk JG, Healy LM et al (2018) Peripherally derived macrophages modulate microglial function to reduce inflammation after CNS injury. PLoS Biol 16(10):e2005264. https://doi.org/10.1371/journal.pbio.2005264
Hong LTA, Kim YM, Park HH et al (2017) An injectable hydrogel enhances tissue repair after spinal cord injury by promoting extracellular matrix remodeling. Nat Commun 8(1):533. https://doi.org/10.1038/s41467-017-00583-8
Milich LM, Ryan CB, Lee JK (2019) The origin, fate, and contribution of macrophages to spinal cord injury pathology. Acta Neuropathol 137(5):785–797. https://doi.org/10.1007/s00401-019-01992-3
Heller RA, Seelig J, Crowell HL et al (2021) Predicting neurological recovery after traumatic spinal cord injury by time-resolved analysis of monocyte subsets. Brain 144(10):3159–3174. https://doi.org/10.1093/brain/awab203
Kirshblum SC, Botticello AL, Dyson-Hudson TA et al (2016) Patterns of sacral sparing components on neurologic recovery in newly injured persons with traumatic spinal cord injury. Arch Phys Med Rehabil 97(10):1647–1655. https://doi.org/10.1016/j.apmr.2016.02.012
Kirshblum S, Snider B, Eren F, Guest J (2021) Characterizing natural recovery after traumatic spinal cord injury. J Neurotrauma 38(9):1267–1284. https://doi.org/10.1089/neu.2020.7473
Donnelly DJ, Popovich PG (2008) Inflammation and its role in neuroprotection, axonal regeneration and functional recovery after spinal cord injury. Exp Neurol 209(2):378–388. https://doi.org/10.1016/j.expneurol.2007.06.009
Kwon BK, Streijger F, Fallah N et al (2017) Cerebrospinal fluid biomarkers to stratify injury severity and predict outcome in human traumatic spinal cord injury. J Neurotrauma 34(3):567–580. https://doi.org/10.1089/neu.2016.4435
Pouw MH, Kwon BK, Verbeek MM et al (2014) Structural biomarkers in the cerebrospinal fluid within 24 h after a traumatic spinal cord injury: a descriptive analysis of 16 subjects. Spinal Cord 52(6):428–433. https://doi.org/10.1038/sc.2014.26
Yousefifard M, Sarveazad A, Babahajian A et al (2019) Potential diagnostic and prognostic value of serum and cerebrospinal fluid biomarkers in traumatic spinal cord injury: a systematic review. J Neurochem 149(3):317–330. https://doi.org/10.1111/jnc.14637
Zhou W, Mao Z, Wang Z et al (2023) Diagnostic and predictive value of novel inflammatory markers of the severity of acute traumatic spinal cord injury: a retrospective study. World Neurosurg 171:e349–e354. https://doi.org/10.1016/j.wneu.2022.12.015
Zhao JL, Lai ST, Du ZY et al (2020) Circulating neutrophil-to-lymphocyte ratio at admission predicts the long-term outcome in acute traumatic cervical spinal cord injury patients. BMC Musculoskelet Disord 21(1):548. https://doi.org/10.1186/s12891-020-03556-z
Biglari B, Swing T, Child C et al (2015) A pilot study on temporal changes in IL-1β and TNF-α serum levels after spinal cord injury: the serum level of TNF-α in acute SCI patients as a possible marker for neurological remission. Spinal Cord 53(7):510–514. https://doi.org/10.1038/sc.2015.28
Heller RA, Raven TF, Swing T et al (2017) CCL-2 as a possible early marker for remission after traumatic spinal cord injury. Spinal Cord 55(11):1002–1009. https://doi.org/10.1038/sc.2017.69
Moghaddam A, Sperl A, Heller R et al (2016) Elevated serum insulin-like growth factor 1 levels in patients with neurological remission after traumatic spinal cord injury. PLoS ONE 11(7):e0159764. https://doi.org/10.1371/journal.pone.0159764
Alexander JK, Popovich PG (2009) Neuroinflammation in spinal cord injury: therapeutic targets for neuroprotection and regeneration. Prog Brain Res 175:125–137. https://doi.org/10.1016/s0079-6123(09)17508-8
Fehlings MG, Wilson JR, Tetreault LA et al (2017) A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the use of methylprednisolone sodium succinate. Global Spine J 7(3 Suppl):203s-s211. https://doi.org/10.1177/2192568217703085
Chio JCT, Wang J, Surendran V et al (2021) Delayed administration of high dose human immunoglobulin G enhances recovery after traumatic cervical spinal cord injury by modulation of neuroinflammation and protection of the blood spinal cord barrier. Neurobiol Dis 148:105187. https://doi.org/10.1016/j.nbd.2020.105187
Funding
This work was supported by the National Natural Science Foundation (82102656); China Postdoctoral Science Foundation (2022T150452,2021M692299); PostDoctor Research Project, West China Hospital, Sichuan University (2021HXBH021); and Natural Science Foundation of Sichuan Province (2023NSFSC1580, 2022NSFSC1392).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that there are no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, C., Chen, M., Wang, T. et al. Prognostic value of the systemic inflammatory index (SII) and systemic inflammatory response index (SIRI) in patients with traumatic spinal cord injury. Eur Spine J 33, 1245–1255 (2024). https://doi.org/10.1007/s00586-023-08114-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08114-4