Abstract
Purpose
Adolescent idiopoathic scoliosis (AIS) is a progressive spinal deformity, most often observed in female patients of pubescent age. The deformity’s severity, its progression through time, its treatment and subsequent follow-up are assessed with routine radiological evaluation of the patient’s full spine. This study aimed to determine the cumulative radiation exposure in average patients with AIS treated by brace or surgery throughout their treatment.
Methods
The average number of imaging procedures and corresponding radiation doses were retrospectively obtained from the medical charts of AIS patients treated conservatively and/or surgically at our institution. The median radiation exposure of all imaging modalities was stated in effective dose (mSv). The estimated cumulative effective radiation dose of the each treatment group was determined by multiplication of the average number of imaging conducted, and the median effective radiation dose per imaging modality.
Results
In total, 73 AIS patients were included (28 brace, 45 surgically). Patients treated with a brace were subjected to an average of 9.03 full spine radiographs, resulting in an estimated effective cumulative dose of 0.505 mSv over a median treatment period of 3.23 years. Patients treated surgically received an average of 14.29 full spine radiographs over a median treatment period of 2.76 years. The estimated effective cumulative dose amounted from 0.951 to 1.841 mSv, depending on the surgical technique.
Conclusion
The cumulative effective radiation doses rendered to AIS patients as part of their treatment and follow-up were relatively low. However, every exposure to ionising radiation for medical imaging purposes should be minimised.
Similar content being viewed by others
Introduction
Adolescent idiopathic scoliosis (AIS) has been defined as a progressive spinal deformity, most often observed in female patients of roughly pubescent age [1]. To assess the progression of the curvatures over time, patients are routinely regularly exposed to full spine radiographs (every four to eighteen months) [2, 3]. More often than not, these evaluations add up to significant numbers of radiographs [4, 5]. When surgical scoliosis correction is indicated, various preoperative and intraoperative imaging modalities are available to ensure proper pedicle screw placement, including 2D fluoroscopy and the combined use of low-dose preoperative computed tomography (CT) scans and patient-specific 3D printed drill guides [6, 7]. Postoperatively, additional radiographs are taken to assess both the instrumentation and deformity correction achieved [8]. In conservatively treated patients, additional radiographs are taken to assess in-brace curvature correction [4]. The management of AIS is thus associated with repeated doses of radiation in every treatment phase due to medical imaging.
Given that adolescent patients are more susceptible to the carcinogenic effect of ionising radiation, concerns have been raised regarding AIS patients’ potential subsequent health risks associated with the cumulative radiation doses received throughout their treatment [9, 10]. According to a retrospective review by Simony et al. [9], malignancy rates for AIS patients surgically treated 25 years ago may be up to five times higher when compared to an age-matched healthy population. A systematic review by Luan et al. [10] also suggested significantly elevated malignancy rates and their associated mortality in AIS patients as a result of repeated radiographs. Breast cancer is of particular concern, as AIS predominantly affects young females (with a female-to-male ratio of 7.2:1 for severe curvatures), in addition to which an odds ratio of 1.20 has been reported for female AIS patients with regard to developing breast cancer [10, 11]. Therefore, while ensuring adequate imaging quality is maintained, radiation exposure throughout the clinical treatment and follow-up of AIS should be kept to a minimum.
Gathering data regarding cumulative radiation exposures and effective doses per imaging modality is important. Based on this information, the effective dose received by individual patients during the clinical management of their AIS can be predicted, and points of attention can be identified. However, studies reporting such data are scarce, and an overview of the effective dose for every imaging modality during the treatment and follow-up of AIS shows a large variability in the literature [12]. The primary aim of this study, therefore, was to determine cumulative radiation doses for the average AIS patient, whether treated conservatively (i.e. by brace) or surgically.
Most studies have reported that a significant percentage of the cumulative radiation dose is received during surgical treatment [4, 5]. More recently, the combined use of low-dose preoperative CT scans and intraoperative patient-specific 3D printed drill guides has been introduced to secure accurate pedicle screw placement. Satisfactory results regarding the safety and accuracy of this new approach to pedicle screw placement have been reported [7]. In patients operated on with this approach, there is a need for a low-dose CT to preoperatively plan pedicle screw entry points and trajectories, while the need for intraoperative 2D fluoroscopy is abolished. The secondary aim of this study, therefore, was to compare and contrast the cumulative effective doses received by AIS patients surgically treated using either intraoperative 2D fluoroscopy or a combination of a low-dose preoperative CT scan and intraoperative patient-specific 3D printed drill guides.
Methods
After ethical approval was waived by the local ethics committee, a single-centre retrospective review of patients treated for AIS was conducted. In all included patients whose treatments ended from 2016 to 2021, a chart review was performed, and the average number of imaging procedures of each type conducted at our institution throughout their treatment was calculated. Patients were included when treated for AIS by bracing and/or posterior spinal fusion with either intraoperative 2D fluoroscopy guidance or intraoperative 3D printed patient-specific drill guides, including low-dose preoperative CT. Patients whose treatment was still ongoing, who started extensive treatment elsewhere or were in need of additional imagery as a result of complications were excluded from this study. Patients with a spinal deformity resulting from alternative pathologies, such as congenital, degenerative or neuromuscular scoliosis, were also excluded.
The available radiation doses per radiological examination were obtained from radiological archives. The average number of every imaging procedure conducted for diagnosis, treatment and post-therapy follow-up was calculated and related to the median radiation dose per examination in order to arrive at the cumulative effective radiation dose in millisievert (mSv) for the average AIS patient either treated conservatively and/or surgically at our institution. The durations of treatment (starting with the first radiological and ending at 1 year postoperative or 1 year after termination of brace treatment) were defined to determine the period over which the cumulative radiation doses were received. The patients’ ages at the start and end of their treatment were also taken into consideration when converting the dose area product (DAP) in mGy*cm2 or dose length product (DLP) in mGy*cm to the effective dose in mSv. Patient gender was also extracted from the charts.
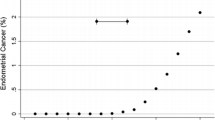
Radiologic management of AIS
Figure 1 shows the radiological management of AIS patients at our institution. At the first assessment, full spine posterior-anterior (PA), lateral and supine bending anterior–posterior (AP) radiographs were taken (Fig. 2). After diagnosis, PA full spine radiographs were repeated every six months for all treatment groups. In patients with a Cobb angle of 25°–40° and a Stage 2 and lower, according to the Risser Classification, brace treatment was prescribed, and a single in-brace full spine PA radiograph was conducted to ensure adequate in-brace curvature correction. Whenever a new brace is fitted, this examination is repeated. In addition, an out-of-brace radiograph was acquired every six months to assess curvature progression under treatment. Brace treatment will continue until patients are no longer expected to grow. At treatment termination, full spine PA radiographs were repeated after one year, followed by orthopaedic discharge.
Surgical correction was performed for Cobb angles larger than 45°–50°. The standard posterior surgical treatment for AIS consists of pedicle screw insertion using intraoperative PA 2D fluoroscopy. To comply with the ‘As Low as Reasonably Achievable’ (ALARA) principle when using intraoperative radiation, we solely performed PA views, with a small diaphragm of maximally 3–4 vertebrae [13]. When pedicle screw insertion is conducted using intraoperative 3D printed patient-specific screw guides, a preoperative low-dose planning CT is performed mandatorily. The 3D pilot hole drill guides and guide docking probes of each individual to be instrumented segment were 3D printed after planning the entry points and interpedicular trajectories of the pedicle screws based on low-dose CT. With this technology, no intraoperative imaging is warranted or used. After surgical treatment, full spine PA and lateral radiographs are routinely taken directly postoperatively and are followed by a full spine PA radiograph at six weeks, half a year and one year after surgery (Fig. 3).
Imaging protocols
Standard radiographs were conducted using Philips DigitalDiagnost C90 (0.1 mm Cu and 1 mm Al spectral filter) at a tube potential of 86 kV and a tube current exposure time product value of 24 mAs. A source imaging receptor distance (SID) of 270 cm was used. For full spine PA radiographs, the exposure width was adjusted to include the projection of both hip joints, while the craniocaudal projection was extended to include the cervical spine and femoral heads. An identical craniocaudal extension was utilised for the lateral and AP bending radiographs. AP bending radiographs were performed in a supine position at an SID of 140 cm.
Intraoperative fluoroscopy was conducted using a Philips Veradius Unity or Ziehm Vision FD mobile C-arm at an average tube potential of 97.5 kV and a tube current exposure time product value of 2.65 mAs. A SID of 98 cm was applicable for both C-arms.
A preoperative low-dose CT (slice thickness 0.6 mm) without intra venous contrast-enhancement was performed for the patients surgically treated using intraoperative 3D printed patient-specific drill guides. The scans were made using a 3rd generation dual-source CT scanner (Somatom Force, Siemens Healthineers, Erlangen, Germany) at a tube potential of 100 kVp. An ultra-low-dose (ULD) CT scan protocol was implemented using a built-in selective photon shield filter (Sn) [7].
Calculation of the effective dose
The available radiation doses, as reported after every radiological procedure performed for curve assessment in the AIS, were obtained from the radiological archives at our institution. DAP (mGy*cm2) values were extracted for conventional radiographs (PA, lateral and side-bending radiographs) and intraoperative 2D fluoroscopy imaging. These DAP values were converted to effective doses by the PCXMC software programme (PCXMCI 1.5.2 STUK, Radiation and Nuclear Safety Authority, Helsinki, Finland) utilising Monte Carlo simulations [14]. A reference individual of 15 years old with a length of 163.99 cm, weighing 54.5 kg, was defined. An age of 15 years was selected, as it best represents the study population since only 10 years old, 15 years old or adult age individuals could be selected. The weight and length of the reference individual were defined as standard according to PCXMC. The acquisition parameters of the protocols described above were imported into the simulations.
To convert DLP (mGy*cm) values extracted from archived low-dose CT scans to effective doses, conversion factors adapted for age and body part were used according to the International Commission on Radiological Protection (ICRP) publication 103 [15]. The conversion factors for CT data were adjusted for age (mean age at conduction of the CT scan: 18.36 years) by linear interpolation, as these were only available for 10-year-olds or adults.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics 28 (IBM Corp., Armonk, NY). Data distribution was examined using the Kolmogorov–Smirnov and Shapiro–Wilk tests. For continuous normally distributed data, the mean ± standard deviation (SD) and range are given. For data that were not normally distributed, the median ± interquartile range (IQR) and range were calculated. Unpaired t tests were used to compare the mean total number of radiographs conducted for patients treated surgically or by brace. A Mann–Whitney U test was performed to compare the median radiation dose of 2D fluoroscopy and the low-dose CT scan. A P value below 0.05 was considered statistically significant.
Results
Table 1 denotes the AIS patients’ characteristics and the average number of each imaging procedure conducted. Of the 73 AIS patients included, 28 were treated conservatively by brace and 45 were treated surgically. In 40 of those patients, pedicle screw insertion was performed using 2D intraoperative fluoroscopy, while in 5 cases, the combination of a preoperative low-dose CT and 3D printed patient-specific drill guides was used. Conservatively treated patients received an average total of 9.03 ± 2.95 (4–14) full spine radiographs. Surgically treated patients were subjected to an average total of 14.29 ± 3.65 (9–28) full spine radiographs.
The median DAP or DLP and the effective dose per radiological imaging procedure are shown in Table 2. A cumulative effective dose of 0.505 mSv was derived for braced patients by combining the average number of each imaging procedure conducted with the median radiation dose per examination. The average patient treated surgically received a dose of 0.951 mSv when pedicle screw insertion was done under 2D fluoroscopy guidance. When making the combined use of preoperative low-dose planning CT and 3D printed intraoperative patient-specific drill guides, a higher effective dose of 1.841 mSv was delivered. Brace therapy prior to surgery would deliver another 0.088 mSv due to in-brace radiographs. The low-dose planning CT delivered a median effective dose of 0.942 ± 0.082 (0.620–1.450) mSv, which is significantly higher (P < 0.001) in comparison to said dose when using intraoperative 2D fluoroscopy (patients were exposed to a median of 0.052 ± 0.050 [0.010–0.410] mSv).
Discussion
Radiation exposure related to the clinical management of AIS is considered disadvantageous due to the patients’ young age and the subsequently elevated risk of developing malignancies [16]. This study aimed to establish a cumulative radiation dose for an average AIS patient treated with a brace or surgery. We were impressed by the relatively low cumulative effective doses calculated for all treatment groups within the realm of this study (Table 3). In braced patients, the cumulative effective dose resulting from repeated full spine radiographs (0.505 mSv) is equivalent to receiving an extra 0.21 years’ worth of local natural background radiation (The worldwide annual average background radiation is estimated to be 2.4 mSv (range 1–10 mSv [12]). As the radiation dose of in-brace full spinal radiographs showed no statistical significant difference compared to out-brace full spinal radiographs, these were mentioned together under 'full spinal PA radiograph' in Table 2. In surgically treated patients, the effective cumulative dose for patients with 2D intraoperative fluoroscopy (0.951 mSv) equals 0.39 years of background radiation. The combination of preoperative low-dose CT scans and patient-specific intraoperative drill guides renders an effective cumulative dose (1.841 mSv), corresponding to 0.77 years of background radiation. Our results demonstrate that, compared to conservatively treated patients, those treated surgically received a higher effective cumulative dose, the reason being the additional radiation used for accurate pedicle screw insertion and a higher average number of full spine radiographs taken. Other studies have yielded similar results [4, 5].
The use of intraoperative 2D fluoroscopy is eliminated by the use of 3D printed patient-specific intraoperative drill guides but comes at a cost in the form of an extra low-dose preoperative CT scan for screw trajectory planning purposes. In this study, the CT protocol delivered a mean effective dose of 0.942 ± 0.580 (0.620–1.450) mSv, in comparison to the significantly (P < 0.001) lower mean effective radiation dose of 0.052 ± 0.050 (0.010–0.410) mSv received when using intraoperative 2D fluoroscopy guidance. As a result, the cumulative effective dose for patients operated on using CT and 3D printed patient-specific intraoperative drill guides increased in comparison to those where 2D fluoroscopy was used.
At the same time, however, the use of planning and patient-specific drill guides has been reported to lead to a significantly higher rate of accurate pedicle screw placement (i.e. higher number of screws placed within the safe zone) in comparison [17]. This, in turn, might eliminate the need for future radiological imagery and follow-up surgery. From these data, the disadvantage of additional radiation exposure can be weighed against the advantage of more accurate pedicle screw insertion and radiation-free surgery.
A study by Cecchinato et al. [7, 18] included 12 surgically treated patients, comparing the use of intraoperative 2D fluoroscopy with the combined use of low-dose preoperative CT scans and patient-specific intraoperative 3D printed drill guides. In the latter group, the use of intraoperative 2D fluoroscopy was reduced by 72%. In our study, the use of 2D fluoroscopy could be abolished altogether for the ‘scan and drill guides’ patient group, as an additional 1:1 3D printed model of the patients’ full spine was made available and was used during surgery for orientation and segment specification through the identification of anatomical landmarks.
The low-dose CT scan protocol used for the surgical planning of the pedicle screw entry points and trajectories by Cecchinato et al. [18] on average delivered a radiation dose of 2.15 mSv. In our study, a ULD CT scan protocol was used, delivering a lower median radiation dose of 0.942 ± 0.580 (0.620–1.450) mSv. This could be achieved by adding a selective photon shield filter (Sn), thus effectively removing the majority of low-energy photons. Overall, the cumulative effective radiation dose could therefore be minimised both by eliminating intraoperative 2D fluoroscopy (thanks to an additional 1:1 3D model of the full spine) and by developing a preoperative ULD CT protocol.
Demirel et al. [5] described the cumulative effective dose of conservative or surgically treated juvenile idiopathic scoliosis and AIS patients. These patients were radiologically examined using primarily EOS® low-dose stereoradiography, with a low-dose intraoperative O-arm protocol used to facilitate correct pedicle screw placement during surgery. Patients treated with a brace or patients who merely received radiological follow-up in this study received a median cumulative effective dose of 1.1 mSv, while the average patient treated with a brace in our cohort showed a lower cumulative effective dose of 0.505 mSv. Patients surgically treated by Demirel et al. [5] were subjected to a median cumulative effective dose of 10.8 mSv, 50% of which was a result of intraoperative imaging (median of two O-arm 3D scans and 2D fluoroscopy). In our study, the cumulative effective dose for surgically treated patients depended mainly on the technology used to ensure accurate pedicle screw insertion. Still, both surgical treatment groups were subjected to a substantially lower cumulative radiation dose than those reported by Demirel et al. [5]. Intraoperative 2D fluoroscopy accounted for 6.3% of the cumulative radiation dose when used to guide pedicle screw insertion in our study. In addition to intraoperative 3D printed patient-specific drill guides, no additional intraoperative imaging was used. The low-dose CT scan made prior to surgery delivered 55% of the cumulative effective radiation dose (0.942 ± 0.580 [0.620–1.450] mSv).
Subsequent health risks
Increased cancer risk associated with low-dose radiation exposure has been studied in survivors of nuclear bombings, establishing a higher cancer incidence and increased mortality [12, 19]. In addition, the ICRP has reported a 0.5% increase in the risk of death by cancer associated with each additional Sv (0.005% for each mSv) of radiation exposure [20]. In our study population, therefore, the braced patients ran an increased cancer mortality risk of 0.003%, and the surgically treated patients ran an extra 0.005% (2D intraoperative fluoroscopy group) or 0.009% (CT scan and 3D printed models and guides group). These increases must be compared to the overall risk of death from cancer, amounting to 20.5% for males and 17.9% for females, as reported by the American Cancer Society 2022 [21].
Simony et al. [9] reported a cancer incidence of 4.3% in AIS patients treated surgically or with braces between 1983 and 1990, most of whom were affected by breast and endometrial cancers. This reported incidence amounts to a fivefold increase compared to an age-matched healthy population. The patients included in this published cohort received a mean total of 16.3 radiographs, with radiation doses per radiograph ranging from 0.8 to 1.4 mSv. Patients treated for AIS between 1983 and 1990 thus received a cumulative effective dose between 13.04 mSv and 22.82 mSv. The cumulative effective dose of all treatment groups that we calculated based on the ICRP report was substantially lower, at least by 86%. It is not clear why the cancer incidence is much higher in the cohort studied by Simony et al. [9].
Reducing radiation exposure
In accordance with the ALARA principle, a patient’s exposure to ionising radiation should be kept low as reasonably achievable without compromising imaging quality [22]. To realise a reduction in radiation exposure as part of the clinical treatment of AIS, various methods have been introduced, such as the EOS® low-dose stereoradiography instead of conventional radiographs for the radiological evaluation of spinal deformity [23]. This technique makes use of orthogonally placed X-ray tubes and detector pairs, as well as a gaseous particle detector with a multiwire proportional chamber. This method allows for the simultaneous capture of PA-AP and lateral radiographs, thus eliminating the need for digital stitching of multiple radiographs. This method has been reported to enhance imaging quality and reduce the time needed per imaging procedure [24, 25].
Its main advantage, however, lies in the reported reduction in exposure to radiation. Luo et al. [23] showed such a decrease when comparing EOS® low-dose stereoradiography to conventional radiographs in a cohort of AIS patients, reporting an average radiation dose of 0.069 mSv for PA full spine radiographs and 0.121 mSv for lateral full spine radiographs. Our study results show a median radiation dose of 0.051 ± 0.047 (0.018–0.19) mSv and 0.074 ± 0.047 (0.024–0.211) mSv, respectively, for PA and lateral full spine radiographs. As such, the radiation dose received with a single PA or lateral conventional radiograph at our institution is not inferior to the radiation dose received by using EOS® low-dose stereoradiography [23]. To minimise the radiation doses of conventional radiographs at our institution, respecting the ALARA principle by both limiting the width of the radiation beam and minimising exposure has become a standard medical practice. X-ray beam minimisation was realised by eliminating the os ilium from the radiograph. The bone age was based on a left-hand radiograph instead. The radiation dose of this radiograph was considered negligible. In addition, all follow-up radiographs were conducted with reduced imaging quality, hence with a lower associated radiation dose. Finally, to prevent unwarranted patient exposure to medical imaging, any emerging subsequent need for radiographs was always critically appraised.
Currently, there are no international guidelines regarding the amount and timing of radiographs in the treatment of AIS [5]. At our institution, patients are subjected to radiological evaluation at least once every six months to monitor curvature progression. There is a variety in the literature from 4 to 18 months between radiological evaluations, mainly depending on the skeletal maturity and remaining growth of the patient [2, 3]. Future research should focus on the impact of extended follow-up intervals to further reduce radiation exposure, as also recommended by Demirel et al. [5].
International consensus regarding the amount, timing and interval of postoperative radiographs is also lacking [5]. In this study, the AIS patients were subjected to a mean total of 3.56 ± 0.59 (2–4) PA and 1.80 ± 0.79 (1–4) lateral full spine radiographs in the first postoperative year. Radiographs taken more than one year postoperatively were excluded because they were deemed clinically insignificant by the authors and were no longer being conducted. A study by Garg et al. [8] concludes that, in the absence of symptoms, routine postoperative radiological evaluations in the first year after surgery rarely provide essential information. Their suggestion is to make a single PA and lateral radiograph one to two months after surgery, followed by annual radiographs to monitor spinal alignment, until no further patient growth is expected. In our cohort, this approach would lead to a further 0.190 mSv reduction in radiation exposure, but additional imaging would be needed to monitor the remaining patient growth. However, this protocol should be investigated prospectively before such an approach is put into extensive use.
We acknowledge several limitations to this study, the first of which is our choice to use a retrospective study design. Effectively making it impossible to determine each patient’s actual individual cumulative effective dosage since the exposure details of full spinal radiographs and intraoperative 2D-fluoroscopy were not routinely recorded. This was most notably the case regarding radiographs taken at the beginning of clinical treatment. As a result, the number of imaging procedures described in Table 2 to form the median effective dose per imaging modality was limited. However, we were able to calculate the average amount of imaging conducted for each treatment group using all the imaging actually performed. This, in our opinion, enabled us to postulate a cumulative effective radiation dose for the average AIS patient treated with brace and/or surgery at our institution without any underestimation of the missing actual figures. Second, we recently introduced a combination of preoperative low-dose CT scans and patient-specific intraoperative 3D printed drill guides for accurate pedicle screw insertion into our clinical practice. As a result, the number of patients included using this technique did not match the number of surgically treated patients using intraoperative 2D fluoroscopy guidance. Future research should include more patients operated on using the new patient-matching planning technology to provide additional data regarding the radiation dose delivered by the low-dose CT scan.
Conclusion
The estimated cumulative effective radiation exposure in the clinical treatment of AIS patients, as calculated in this study, was relatively low, given the ample number of radiological examinations conducted and the cumulative radiation dose reported elsewhere in the literature. However, any amount of additional radiation exposed to as a result of medical imaging represents potential harm, especially so in the adolescent patient and should therefore be kept to a minimum. In surgically treated patients, the recently introduced combination of preoperative low-dose CT scans and patient-specific intraoperative drill guides for accurate pedicle screw insertion increased the average cumulative effective radiation dose compared to the use of intraoperative 2D fluoroscopy, which was caused by the significantly higher radiation dose of the preoperative low-dose CT scan.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable
References
Janicki JA, Alman B (2007) Scoliosis: review of diagnosis and treatment. Paediatr Child Health 12:6
Kim HK, Moon HS, Yoon ES, Chung C, Song TS, Suh H, Lee F, Kim YHS (2010) Scoliosis imaging: what radiologists should know. Radiographics 30:22
Knott P, Pappo E, Michelle Cameron JC, deMauroy C, Rivard TK, Zaina F, Wynne J, Stikeleather L, Bettany-Saltikov J, Grivas TB, Durmala J, Maruyama T, Negrini S, O’Brien JP, Rigo M (2014) SOSORT 2012 consensus paper: reducing x-ray exposure in pediatric patients with scoliosis. Scoliosis. https://doi.org/10.1186/1748-7161-9-4
Presciutti SM, Karukanda T, Lee M (2014) Management decisions for adolescent idiopathic scoliosis significantly affect patient radiation exposure. Spine J Off J North Am Spine Soc 14:1984–1990. https://doi.org/10.1016/j.spinee.2013.11.055
Demirel AP, Søren PH, PE, (2020) Cumulative radiation exposure during current scoliosis management. Dan Med J 67:5
Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, Ploumis A, Xenakis TA (2012) Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 21:247–255. https://doi.org/10.1007/s00586-011-2011-3
Cool J, van Schuppen J, de Boer MA, van Royen BJ (2021) Accuracy assessment of pedicle screw insertion with patient specific 3Dprinted guides through superimpose CT-analysis in thoracolumbar spinal deformity surgery. Eur Spine J. https://doi.org/10.1007/s00586-021-06951-9
Garg S, Kipper E, LaGreca J, Carry P, Erickson M (2015) Are routine postoperative radiographs necessary during the first year after posterior spinal fusion for idiopathic scoliosis? A retrospective cohort analysis of implant failure and surgery revision rates. J Pediatr Orthop 35:6
Simony A, Hansen EJ, Christensen SB, Carreon LY, Andersen MO (2016) Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. Eur Spine J 25:3366–3370. https://doi.org/10.1007/s00586-016-4747-2
Luan FJ, Wan Y, Mak KC, Ma CJ, Wang HQ (2020) Cancer and mortality risks of patients with scoliosis from radiation exposure: a systematic review and meta-analysis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 29:3123–3134. https://doi.org/10.1007/s00586-020-06573-7
Konieczny MR, Senyurt H, Krauspe R (2013) Epidemiology of adolescent idiopathic scoliosis. J Child Orthop 7:3–9. https://doi.org/10.1007/s11832-012-0457-4
Pace N, Ricci L, Negrini S (2013) A comparison approach to explain risks related to X-ray imaging for scoliosis, 2012 SOSORT award winner. Scoliosis 8:11. https://doi.org/10.1186/1748-7161-8-11
Do KH (2016) General principles of radiation protection in fields of diagnostic medical exposure. J Korean Med Sci 31(Suppl 1):S6-9. https://doi.org/10.3346/jkms.2016.31.S1.S6
Harrison RL (2010) Introduction to monte carlo simulation. AIP Conf Proc 1204:17–21. https://doi.org/10.1063/1.3295638
Deak PD, Smal Y, Kalender WA (2010) Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 257:9. https://doi.org/10.1148/radiol.10100047/-/DC1
Larson AN, Schueler BA, Dubousset J (2019) Radiation in Spine deformity: state-of-the-art reviews. Spine Deform 7:386–394. https://doi.org/10.1016/j.jspd.2019.01.003
Wallace N, Butt B, Aleem I, Patel R (2020) Three-dimensional printed drill guides versus fluoroscopic-guided freehand technique for pedicle screw placement. Clin Spine Surg 33:9
Cecchinato R, Berjano P, Zerbi A, Damilano M, Redaelli A, Lamartina C (2019) Pedicle screw insertion with patient-specific 3D-printed guides based on low-dose CT scan is more accurate than free-hand technique in spine deformity patients: a prospective, randomized clinical trial. Eur Spine J 28:1712–1723. https://doi.org/10.1007/s00586-019-05978-3
Ozasa K, Shimizu Y, Suyama A, Kasagi F, Soda M, Grant EJ, Sakata R, Sugiyama H, Kodama K (2012) Studies of the mortality of atomic bomb survivors, report 14, 1950–2003: an overview of cancer and noncancer diseases. Radiat Res 177:229–243. https://doi.org/10.1667/rr2629.1
ICRP (1990) 1990 Recommendations of the international commission on radiological protection. Ann ICRP 21:201
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72:7–33. https://doi.org/10.3322/caac.21708
Strauss KJ, Kaste SC (2006) The ALARA (as low as reasonably achievable) concept in pediatric interventional and fluoroscopic imaging: striving to keep radiation doses as low as possible during fluoroscopy of pediatric patients–a white paper executive summary. Pediatr Radiol 36(Suppl 2):110–112. https://doi.org/10.1007/s00247-006-0184-4
Luo TD, Stans AA, Schueler BA, Larson AN (2015) Cumulative radiation exposure with EOS imaging compared with standard Spine radiographs. Spine Deform 3:144–150. https://doi.org/10.1016/j.jspd.2014.09.049
Garg B, Mehta N, Bansal T, Malhotra R (2020) EOS(R) imaging: Concept and current applications in spinal disorders. J Clin Orthop Trauma 11:786–793. https://doi.org/10.1016/j.jcot.2020.06.012
Deschênes S, Charron G, Beaudoin G, Labelle H, Dubois J, Miron M, Parent S (2010) Diagnostic imaging of spinal deformities. Spine 35:6
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by JC, JS, MAB, BJR. The first draft of the manuscript was written by JC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethics approval
Ethical approval was waived by the local Ethics Committee of Amsterdam UMC, University of Amsterdam in view of the retrospective nature of the study, and all the procedures being performed were part of the routine care (reference number W21_090 # 21.101).
Consent to participate
Informed consent was obtained from all individual participants and/or parents included in the study.
Consent for publication
Patients and/or parents provided informed consent regarding publishing their data and photographs.
Informed consent
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cool, J., Streekstra, G.J., van Schuppen, J. et al. Estimated cumulative radiation exposure in patients treated for adolescent idiopathic scoliosis. Eur Spine J 32, 1777–1786 (2023). https://doi.org/10.1007/s00586-023-07651-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07651-2