Abstract
Purpose
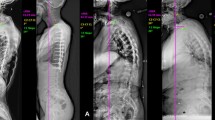
To evaluate the impact of the lowest instrumented vertebra (LIV) on Distal Junctional kyphosis (DJK) incidence in adult cervical deformity (ACD) surgery.
Methods
Prospectively collected data from ACD patients undergoing posterior or anterior–posterior reconstruction at 13 US sites was reviewed up to 2-years postoperatively (n = 140). Data was stratified into five groups by level of LIV: C6-C7, T1-T2, T3-Apex, Apex-T10, and T11-L2. DJK was defined as a kyphotic increase > 10° in Cobb angle from LIV to LIV-1. Analysis included DJK-free survival, covariate-controlled cox regression, and DJK incidence at 1-year follow-up.
Results
25/27 cases of DJK developed within 1-year post-op. In patients with a minimum follow-up of 1-year (n = 102), the incidence of DJK by level of LIV was: C6-7 (3/12, 25.00%), T1-T2 (3/29, 10.34%), T3-Apex (7/41, 17.07%), Apex-T10 (8/11, 72.73%), and T11-L2 (4/8, 50.00%) (p < 0.001). DJK incidence was significantly lower in the T1-T2 LIV group (adjusted residual = −2.13), and significantly higher in the Apex-T10 LIV group (adjusted residual = 3.91). In covariate-controlled regression using the T11-L2 LIV group as reference, LIV selected at the T1-T2 level (HR = 0.054, p = 0.008) or T3-Apex level (HR = 0.081, p = 0.010) was associated with significantly lower risk of DJK. However, there was no difference in DJK risk when LIV was selected at the C6-C7 level (HR = 0.239, p = 0.214).
Conclusion
DJK risk is lower when the LIV is at the upper thoracic segment than the lower cervical segment. DJK incidence is highest with LIV level in the lower thoracic or thoracolumbar junction.




Similar content being viewed by others
References
Shamji MF, Ames CP, Smith JS et al (2013) Myelopathy and spinal deformity: relevance of spinal alignment in planning surgical intervention for degenerative cervical myelopathy. Spine 38:S147–S148
Passias PG, Soroceanu A, Smith J et al (2015) Postoperative cervical deformity in 215 thoracolumbar patients with adult spinal deformity: prevalence, risk factors, and impact on patient-reported outcome and satisfaction at 2-year follow-up. Spine 40:283–291
Tan LA, Riew KD, Traynelis VC (2017) Cervical spine deformity-Part 1: biomechanics, radiographic parameters, and classification. Neurosurgery 81:197–203
Tan LA, Riew KD, Traynelis VC (2017) Cervical spine deformity-part 2: management algorithm and anterior techniques. Neurosurgery 81:561–567
Tan LA, Riew KD, Traynelis VC (2017) Cervical spine deformity-Part 3: posterior techniques, clinical outcome, and complications. Neurosurgery 81:893–898
Kato S, Nouri A, Wu D et al (2018) Impact of cervical spine deformity on preoperative disease severity and postoperative outcomes following fusion surgery for degenerative cervical myelopathy: sub-analysis of aospine north america and international studies. Spine 43:248–254
Ames CP, Smith JS, Eastlack R et al (2015) Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 23:673–683
Scheer JK, Passias PG, Sorocean AM et al (2016) Association between preoperative cervical sagittal deformity and inferior outcomes at 2-year follow-up in patients with adult thoracolumbar deformity: analysis of 182 patients. J Neurosurg Spine 24:108–115
Scheer JK, Tang JA, Smith JS et al (2013) Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 19:141–159
Passias PG, Oh C, Horn SR et al (2019) Predicting the occurrence of complications following corrective cervical deformity surgery: analysis of a prospective multicenter database using predictive analytics. J Clin Neurosci 59:155–161
Scheer JK, Fakurnejad S, Lau D et al (2015) Results of the 2014 SRS survey on PJK/PJF: a report on variation of select SRS member practice patterns, treatment indications, and opinions on classification development. Spine 40:829–840
Glassman SD, Coseo MP, Carreon LY (2016) Sagittal balance is more than just alignment: why PJK remains an unresolved problem. Scoliosis Spinal Disord 11:1
Smith MW, Annis P, Lawrence BD, Daubs MD, Brodke DS (2015) Acute proximal junctional failure in patients with preoperative sagittal imbalance. Spine J 15:2142–2148
Fradet L, Wang X, Crandall D, Aubin CE (2018) Biomechanical analysis of acute proximal junctional failure after surgical instrumentation of adult spinal deformity: the impact of proximal implant type, osteotomy procedures, and lumbar lordosis restoration. Spine Deform 6:483–491
Hostin R, McCarthy I, O’Brien M et al (2013) Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine 38:1008–1015
Theologis AA, Burch S (2015) Prevention of acute proximal junctional fractures after long thoracolumbar posterior fusions for adult spinal deformity using 2-level cement augmentation at the upper instrumented vertebra and the vertebra 1 level proximal to the upper instrumented vertebra. Spine 40:1516–1526
Lonner BS, Newton P, Betz R et al (2007) Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine 32:2644–2652
Denis F, Sun EC, Winter RB (2009) Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine 34:E729–E734
Trobisch PD, Ducoffe AR, Lonner BS, Errico TJ (2013) Choosing fusion levels in adolescent idiopathic scoliosis. J Am Acad Orthop Surg 21:519–528
Cho KJ, Lenke LG, Bridwell KH, Kamiya M, Sides B (2009) Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine 34:765–770
Yanik HS, Ketenci IE, Coskun T, Ulusoy A, Erdem S (2016) Selection of distal fusion level in posterior instrumentation and fusion of Scheuermann kyphosis: is fusion to sagittal stable vertebra necessary? Eur Spine J 25:583–589
Sardar ZM, Ames RJ, Lenke L (2019) Scheuermann’s Kyphosis: diagnosis, management, and selecting fusion levels. J Am Acad Orthop Surg 27:e462–e472
Passias PG, Vasquez-Montes D, Poorman GW et al (2018) Predictive model for distal junctional kyphosis after cervical deformity surgery. Spine J 18:2187–2194
Passias PG, Horn SR, Oh C et al (2020) Predicting the occurrence of postoperative distal junctional kyphosis in cervical deformity patients. Neurosurgery 86:E38–E46
O Brien MF KTBK (2005) Spinal Deformity Study Group Radiographic Measurement Manual http://www.oref.org/docs/default-source/default-document-library/sdsg-radiographic-measuremnt-manual.pdf?sfvrsn=2. Accessed August 21, 2021.
Harrison DE, Harrison DD, Cailliet R et al (2000) Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine 25:2072–2078
Alentado VJ, Lubelski D, Healy AT et al (2016) Predisposing characteristics of adjacent segment disease after lumbar fusion. Spine 41:1167–1172
Nohara A, Kawakami N, Seki K et al (2015) The effects of spinal fusion on lumbar disc degeneration in patients with adolescent idiopathic scoliosis: a minimum 10-year follow-Up. Spine Deform 3:462–468
Berjano P, Damilano M, Pejrona M, Langella F, Lamartina C (2020) Revision surgery in distal junctional kyphosis. Eur Spine J 29:86–102
Kuhns CA, Bridwell KH, Lenke LG et al (2007) Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5–S1 disc, minimum 5-year follow-up. Spine 32:2771–2776
Edwards CN, Bridwell KH, Patel A et al (2003) Thoracolumbar deformity arthrodesis to L5 in adults: the fate of the L5–S1 disc. Spine 28:2122–2131
Yang J, Andras LM, Broom AM et al (2018) Preventing distal junctional kyphosis by applying the stable sagittal vertebra concept to selective thoracic fusion in adolescent idiopathic scoliosis. Spine Deform 6:38–42
Ghasemi A, Stubig T, Nasto A, Ahmed M, Mehdian H (2017) Distal junctional kyphosis in patients with Scheuermann’s disease: a retrospective radiographic analysis. Eur Spine J. 26:913–920
Kim HJ, Nemani V, Boachie-Adjei O et al (2017) Distal fusion level selection in scheuermann’s kyphosis: a comparison of lordotic disc segment versus the sagittal stable vertebrae. Global Spine J 7:254–259
Schwab F, Ungar B, Blondel B et al (2012) Scoliosis research society—schwab adult spinal deformity classification. Spine 37:1077–1082
Yilgor C, Sogunmez N, Boissiere L et al (2017) Global Alignment and Proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99:1661–1672
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
Data was collected from a database of 13 spine centers in the United States, which was approved by the institutional review board (IRB) at each participating unit.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ye, J., Rider, S.M., Lafage, R. et al. Distal junctional kyphosis in adult cervical deformity patients: where does it occur?. Eur Spine J 32, 1598–1606 (2023). https://doi.org/10.1007/s00586-023-07631-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07631-6