Abstract
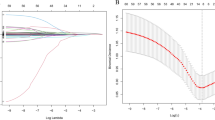
Ossification of the posterior longitudinal ligament (OPLL) causes serious problems, such as myelopathy and acute spinal cord injury. The early and accurate diagnosis of OPLL would hence prevent the miserable prognoses. Plain lateral radiography is an essential method for the evaluation of OPLL. Therefore, minimizing the diagnostic errors of OPLL on radiography is crucial. Image identification based on a residual neural network (RNN) has been recognized to be potentially effective as a diagnostic strategy for orthopedic diseases; however, the accuracy of detecting OPLL using RNN has remained unclear. An RNN was trained with plain lateral cervical radiography images of 2,318 images from 672 patients (535 images from 304 patients with OPLL and 1,773 images from 368 patients of Negative). The accuracy, sensitivity, specificity, false positive rate, and false negative rate of diagnosis of the RNN were calculated. The mean accuracy, sensitivity, specificity, false positive rate, and false negative rate of the model were 98.9%, 97.0%, 99.4%, 2.2%, and 1.0%, respectively. The model achieved an overall area under the curve of 0.99 (95% confidence interval, 0.97–1.00) in which AUC in each fold estimated was 0.99, 0.99, 0.98, 0.98, and 0.99, respectively. An algorithm trained by an RNN could make binary classification of OPLL on cervical lateral X-ray images. RNN may hence be useful as a screening tool to assist physicians in identifying patients with OPLL in future setting. To achieve accurate identification of OPLL patients clinically, RNN has to be trained with other cause of myelopathy.


Similar content being viewed by others
References
Shin J, Choi J, Kim Y, Chang J, Yoon S (2019) Quantification of Risk Factors for Cervical Ossification of the Posterior Longitudinal Ligament in Korean Populations. Spine (Phila Pa) 44(16):E957–E964
Iwaski M, Yonenobu K. (2011) Ossification of the posterior longitudinal ligament. In: Herkowitz H, Garfin S, Eismont F, et al. Rothman-Simeone The Spine. 6th ed. 896–912.
Resnick D, Guerra J Jr, Robinson CA et al (1978) Association of diffuse idiopathic skeletal hyperotosis (DISH) and calcification and ossification of the posterior longitudinal ligament. AJR Am J Roentgenol 131:1049–1053
Matsunaga S, Nakamura K, Seichi A et al (2008) Radiographic predictors for the development of myelopathy in patients with ossification of the posteriro longitudinal ligament: a multicenter cohort study. Spine (Phila Pa) 33:2648–2650
Koyanagi I, Imamura H, Fujimoto S et al (2004) Spinal canal size in ossification of the longitudinal ligament of the cervical spine. Surg Neurol 62:286–291
Matsunaga S, sakou T, Taketomi E, et al. (2004) Clinical cource of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study. J Neurosurg 100(3 suppl Spine):245–8.
Endo S, Shimamura T, Nakae H et al (1994) Cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Arch Orthop Trauma Surg 113:213–221
Koyanagi I, Iwasaki Y, Hida K et al (2003) Acute cervical cord injury associated with ossification of the posteriro longitudinal ligament. Neurosurg 53:887–891
Kwon SY, Shin JJ, Lee JH, Cho WH (2015) Prognostic factors for surgical outcome in spinlal cord injury associated with ossification of the postrior longitudinal ligament (OPLL). J Orthop Surg Res 10:94
Katoh S, el Masry WS, Jaffery D et al (1996) Neurologic outcome in consevatively treated patients with incomplete closed traumatic cervical spinal cord injuries. Spine (Phila Pa) 21:2345–2351
Chen LF, Tu TH, Chen YC et al (2016) Risk of spinal cord injury in patients with cervical spondylotic myelopathy and ossification of posterior longitudinal ligament: a national cohort study. Neurosurg Focus 40:E4
Koyanagi I, Iwasaki Y, Hida K et al (2000) Acute cervical cord injury without fracture or dislocation of the spinal column. J Nuerosurg 93:15–20
Wu JC, Chen YC, Liu L et al (2012) Conservatively treated ossification of the posterior longitudinal ligament increases the risk of spinal cor injury: a nation-wide cohort study. J Neurotrauma 29:462–468
Onishi E, Sakamoto A, Murata S, Matushita M (2012) Risk factors for acute cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Spine (Phila Pa) 37:660–666
Chikuda H, Seichi A, Takeshita K et al (2011) Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: a multicenter study. Spine (Phila Pa) 36:1453–1458
Gu Y, Chen L, Dong RB et al (2014) Laminoplasty versus conservative treatment for acute cervical spinal cord injury caused by ossification of the posterior longitudinal ligament after minor trauma. Spine J 14:344–352
Matsunaga S, Sakou T, Hayashi K et al (2002) Trauma-induced myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg 97:172–175
Kang MS, Lee JW, Zhang HY et al (2012) Diagnosis of Cervical OPLL in Lateral Radiograph and MRI: Is It Reliable? Korean J Spine 9(3):205–208
Romero LG, Cable W, Lesniak A, Tseytlin E, McHugh J, Parwani A, et al. (20139) Digital pathology consultations-a new era in digital imaging, challenges and practical applications. J Digit Imaging 26(4):668–77.
Peng L, Lin L, Hu H et al (2019) Classification and Quantification of Emphysema Using a Multi-Scale Residual Network. IEEE J Biomed Health Inform 23(6):2526–2536
Maki S, Furuya T, Horikoshi T, et al. (2020) A Deep Convolutional Neural Network With Performance Comparable to Radiologists for Differentiating Between Spinal Schwannoma and Meningioma. Spine (Phila Pa 1976) 45(10):694–700.
Murata K, Endo K, Aihara T, et al. (2020) Artificial intelligence for the detection of vertebral fractures on plain spinal radiography. Sci Rep [ePub ahead of print].
Ioffe S, Szegedy C. (2015) Batch normalization: Accelerating deep network training by reducing internal covariate shift", ICML 37.
Kang MS, Lee JW, Zhang HY et al (2012) Diagnosis of cervical OPLL in lateral radiograph and MRI: is it reliable? Korean J Spine 9:205–208
He K, ZhangX, Ren S, et al. (2016) Deep Residual Learning for Image Recognition. IEEE 770–8.
Banzato T, Cherubini GB, Atzori M, Zotti A (2018) Development of a deep convolutional neural network to predict grading of canine meningiomas from magnetic resonance images. Vet J 235:90–92
Banzato T, Bernardini M, Cherubini G, Zotti A (2018) A Methodological Approach for Deep Learning to Distinguish Between Meningiomas and Gliomas on Canine MR-images. BMC Vet Res 14(1):317
Chiba K, Kato Y, Tsuzuki N et al (2005) Computer-assisted measurement of the size of ossification in patients with ossification of the posterior longitudinal ligament in the cervical spine. J Orthop Sci 10(5):451–456
Doi T, Sakamoto R, Horii C, et al. (2020) Risk factors for progression of ossification of the posterior longitudinal ligament in asymptomatic subjects. J Neurosurg Spine 8:1–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest in any form received from a commercial party associated directly or indirectly with this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Murata, K., Endo, K., Aihara, T. et al. Use of residual neural network for the detection of ossification of the posterior longitudinal ligament on plain cervical radiography. Eur Spine J 30, 2185–2190 (2021). https://doi.org/10.1007/s00586-021-06914-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06914-0