Abstract
Purpose
Possible surgical therapies for odontoid fracture type IIb include odontoid screw osteosynthesis (OG) with preservation of mobility or dorsal C1/2 fusion with restriction of cervical rotation. In order to reduce material loosening in odontoid screw osteosynthesis in patients with low bone density, augmentation at the base of the axis using bone cement has been established as a suitable alternative. In this study, we compared cement-augmented OG and C1/2 fusion according to Harms (HG).
Methods
Body donor preparations of the 1st and 2nd cervical vertebrae were randomized in 2 groups (OG vs. HG). The range of motion (ROM) was determined in 3 principle motion plains. Subsequently, a cyclic loading test was performed. The decrease in height of the specimen and the double amplitude height were determined as absolute values as an indication of screw loosening. Afterward, the ROM was determined again and loosening of the screws was measured in a computed tomography.
Results
A total of 16 were included. Two groups of 8 specimens (OG vs. HG) from patients with a median age of 80 (interquartile range (IQ) 73.5–85) years and a reduced bone density of 87.2 (IQ 71.2–104.5) mg/cc dipotassium hydrogen phosphate were examined for their biomechanical properties. Before and after exposure, the OG preparations were significantly more mobile. At the time of loading, the OG had similar loading properties to HG decrease in height of the specimen and the double amplitude height. Computed tomography revealed similar outcomes with regard to the screw loosening rate (62.5 vs. 87.5%, p = 0.586).
Conclusion
In patients with an odontoid fracture type IIb and reduced bone density, cement-augmented odontoid screw yielded similar properties in the loading tests compared to the HG. It may, therefore, be considered as a primary alternative to preserve cervical mobility in these patients.
Similar content being viewed by others
Introduction
The surgical approach to odontoid fractures type IIb in the elderly is challenging. Anchoring the osteosynthesis material may be needed due to the reduced bone mineralization [1]. The optimal approach to achieve this target remains unclear [2]. The least invasive surgical method is an odontoid screw, which represents the treatment of choice in many clinics, but in the long term, this procedure is associated with a high risk of pseudarthrosis, material dislocation and subsequent neck pain [3]. Another established surgical procedure in these patients is the C1/2 fusion according to Harms or Magerl which are associated with higher fusion rates [4, 5]. However, both methods are more invasive and are associated with higher morbidity. A major disadvantage C1/2 fusion is the resulting stiffening of the 1st and 2nd cervical vertebrae and the associated restriction of rotation of the head [6].
The major difference of both surgical strategies is the obtained stiffness. Patients, who were treated with an odontoid screw, have no restriction of the physiological motion. The Harms method is more stiff and leads to a complete loss of motion in the operated segment.
In a cadaver study, Waschke et al. demonstrated a significant improvement in biomechanical stability with a novel surgical method by additionally augmenting the screw in the corpus using bone cement, thus minimizing the migration rate of the screw in osteoporotic bone [7].
The aim of our study was to compare the biomechanical stability after a cement-augmented odontoid screw to dorsal stabilization according to Harms in C1/2 in geriatric patients. We hypothesized that the biomechanical stability using the less invasive cement-augmented odontoid screw would be equivalent to that using C1/2 dorsal stabilization, justifying its use as primary approach to maintain cervical mobility in these patients.
Materials and methods
A total of 16 body donor preparations of the 1st and 2nd cervical vertebrae were included. All body donors have voluntarily participated in the university's anatomical body donor program during their lifetime and have made themselves available free of charge for teaching and research purposes. The donors for our study should have been over 65 years old at the time of death.
The preparations were cryopreserved for storage. Subsequently, a bone density measurement was carried out using quantitative computed tomography in the area of the base of the axis (Q-CT, CT LightSpeed™ VCT, GE Healthcare).
The dens axis was fractured with an oscillating saw, resulting in a type IIb fracture without destroying the transverse ligament. Randomization was then performed using computer-generated sequence in 2 groups of 8 specimens each. Each group was treated surgically, either with a cement-augmented odontoid screw or with a spondylodesis according to Harms.
Cement-augmented odontoid screw implantation
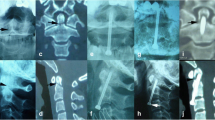
The perforated odontoid screw was inserted ventrally into the body of the fractured second cervical vertebra. A reamer was used to open the cortex centrally at the anterior lower edge. A Kirschner wire was inserted thereafter from the opened cortical bone through the fracture gap into the fractured dens tip. The screw was implanted bicortically over the Kirschner wire and thus the dens tip was fixed to the corpus. After setting the screw, a Jamshidi needle was used to apply high-viscosity polymethylmethacrylate cement (Confidence Spinal Cement System, DePuy SpineTM, Leeds, England). Hereby, the tip of the needle was put next to the head of the screw in the body of C2. The cement was applied under X-ray control around the screw base, which fixes the lag screw proximally [22]. After the cement has set for 5–10 min, the lag screw was tightened again to achieve additional strength and compression of the fragment onto the body (Fig. 1).
C1/2 spondylodesis according to Harms
A total of four screws, two each in the first and second cervical vertebrae, were implanted dorsally and fixed with two rods. The entry point for the screws in the first cervical vertebra was located centrally in the inferior–posterior massa lateralis of the atlas. A polyaxial screw was inserted bicortically. The entry point in the second cervical vertebra was the medial upper quadrant of the pars interarticularis with a 20°–30° converging and cranially directed screw position. These screws should also be placed bicortically. In many cases, a monocortical position is possible in vivo. This depends on the anatomy of the transverse vertebral foramen. The screws in C1 and C2 are finally fixed with a titanium rod (Fig. 2).
Testing procedure
To investigate whether and how physiological movement is restricted by the two different surgical methods, we were using a using a spine tester that has been previously established [8].
The range of motion (ROM) of all preparations was measured in 3 motions plains. With the help of three motors, pure moments were applied: flexion/extension, lateral bending left/right and axial rotation left/right. Loads were applied angle-controlled at a speed of 1°/s. The specimens were loaded to a pure moment between ± 1 Nm in the individual directions of movement, while three loading cycles were performed per plane, of which the third cycle was evaluated in order to minimize viscoelastic effects [9] (Fig. 3).
After the flexibility tests, all specimens were taken to another material testing machine (Instron 8871, Darmstadt, Germany). Here, we wanted to see how the implants behave under loading tests and whether there are signs of loosening of the implants.
The servohydraulic dynamic testing machine was equipped with a self-developed rotating device for continuous loading [10, 11]. In this fixture, the specimen was rotated axially at a speed of 360°/min and at the same time eccentrically loaded cyclically with a lever arm of 30 mm and a gradually increasing force (from 200 to 1200 N in steps of 100 N) and a frequency of 2 Hz.
As a result, repetitive movements starting with a flexion which merges to lateral bending left and followed by extension to lateral bending right were applied, which corresponds to a head movement in the sense of a circular movement. During loading, the decrease in height of the specimen and the double amplitude height, which corresponds to the deflection of the lever arm pressing on the specimen, were determined as absolute values as an indication of screw loosening. Following the cyclic loading tests, the ROM of all specimens was measured in the spine tester and computed tomography of the specimens was performed to determine screw loosening [12]. Loosening was defined when a loosening seam has occurred around a screw or when a screw was dislodged.
Statistical analysis
Data were analyzed using IBM® SPSS® Statistics software, version 22 for Windows. The Shapiro–Wilk test was used to verify the normality assumption of continuous variables. Difference testing between groups was performed using Mann–Whitney test, Chi-square test, or Fisher’s exact test, as appropriate. Changes in ROM, amplitude height and specimen height were assessed using Wilcoxon Test.
Data are presented as medians and interquartile ranges (IQ), or counts and percentages (n, %). All statistics were 2-tailed and a p-value < 0.05 was considered significant.
Results
Characteristics of the study preparations
The median age of the body donors was 80 (IQ 73.5–85) years at the time of death. In total, specimens were taken from 10 women to 6 men. The median bone density value was 87.2 (IQ 71.2–104.5) mg/cc dipotassium hydrogen phosphate (K2HPO4). In the Harms group, the median bone density was 89.5 (IQ 66–115.9) mg/cc K2HPO4. The median age in this group was 82 (IQ 74–84) years with preparations from 5 female and 3 male donors (Table 1). In the OG group, the median age was 78 (72–88) years with a bone mineral density of 87.4 (IQ 66.4–110.1) mg/cc K2HPO4. As in the other group, the preparations were donated by 5 women and 3 men (Table 1). Both groups were statistically comparable with respect to bone density (p = 0.96).
Results of the biomechanical tests
ROM before and after the loading tests
ROM was markedly lower in the Harms than the odontoid screw group before and after loading (Fig. 1). In flexion/extension, an increase in ROM after loading tests was observed in all specimens (flexion/extension before loading—OG vs. HG: 21.7° vs. 4.8°, p = 0.003; flexion/extension after loading—OG vs. HG: 31.6° vs. 7.8°, p = 0.002), mainly in the odontoid screw specimens (Flexion: 9.3° vs. 18.5°, p = 0,012, Extension: 10.6° vs. 13.3°, p = 0.028).
In lateral bending, significantly lower ROMs were measured for all specimens compared to flexion/extension. Likewise, ROM was lower during lateral bending in the Harms than the odontoid screw group before and after loading (Fig. 1). A significant increase in ROM after loading tests was observed in all specimens (lateral bending before loading—OG vs. HG: 5.3° vs. 0.9°, p = 0.003; lateral bending after loading—OG vs. HG: 12.4° vs. 1.8°, p = 0.009).
In axial rotation, the clearest difference between odontoid screw preparations and Harms preparations was found with regard to their mobility. Higher range of motion was observed for odontoid screw preparations before and after loading state compared to Harms preparations (axial rotation before loading—OG vs. HG: 43.8° vs. 1.3°, p < 0.001; axial rotation after loading—OG vs. HG: 66.7° vs. 1.7°, p = 0.001).
Change in specimen height and amplitude height during repetitive loading
During loading in the material testing machine, the constant pressure caused a decrease in the specimen height. The decrease in height of the odontoid screw group and the Harms group was approximately in the same range (Table 2). A significant difference between the two surgical methods was found in the low force range. This difference was evened out at higher force values (Table 2).
A similar behavior of odontoid screw preparations and Harms preparations was observed during loading concerning amplitude height measurements; however, no significant differences were found between the two groups (Table 3).
Computed tomography after loading tests
Computed tomography revealed similar outcomes with regard to the screw loosening rate between the odontoid screw and Harms groups (87.5% vs. 62.5%, p = 0.586). A screw loosening is detected when a loosening seam has occurred around a screw or a dislocation was seen in the computed tomography.
Seven odontoid screws showed a dislocation of the screw compared to pretesting specimen. In the Harms group in 5 cases, a seam around at least one screw, as a sign for a screw loosening, could be detected.
Discussion
In our study, we found that the biomechanical stability was similar between a cement-augmented odontoid screw and dorsal stabilization according to Harms in C1/2 in geriatric patients. Also, the restriction of mobility was significantly lower in patients who were treated with a cement-augmented odontoid screw.
According to the literature, the odontoid fracture is one of the most common cervical fractures in elderly patients and one of the most isolated fractures of the spine in geriatric patients [13,14,15]. Neurological deficits are rare due to the relatively wide spinal canal in this area of the spine [16]. Type II fractures according to Anderson & d'Alonzo account for as much as 95% of the elderly population [17]. Operative or conservative therapies are associated with high mortality [14]. Recent studies showed that surgical therapy can lead to a reduction in mortality rates [18]. In addition, it has been shown that surgical therapy increases functional outcome compared to conservative therapy. For this reason, many authors recommend that the surgical procedure should always be considered in case of an odontoid fracture in elderly patients [19]. Overall, the optimal treatment of the fracture in elderly patients is unclear [20].
Surgical options for the treatment of an odontoid fracture type IIb are on the one hand the ventrally implanted odontoid screw and on the other hand a dorsal fusion, e.g., according to Magerl or Harms. Fusion rates in the dorsal stabilization from C1 to C2 are almost 100% with the major disadvantage that the movement, especially the rotation in the joint, is diminished. This results in a significant restriction of the mobility of the cervical spine. The potential advantages of a lag screw osteosynthesis are the relatively low invasiveness and the preservation of the rotation of the C1/2 joint; however, these may be outweighed by the possible high degree of screw loosening in patients with a low bone mineral density [21]. One possibility to reduce the loosening rate is an additional augmentation of the lag screw with cement. We have already been able to demonstrate this in a biomechanical study and in the clinical practice [7, 22, 23]. In our study, we compared both surgical methods with the background that if the examination results are approximately equivalent, lag screw osteosynthesis is recommended for type IIb fractures. This surgical method does not restrict the mobility of the cervical spine.
In the course of our studies, we have applied a steadily increasing cyclical load to the specimens and imitated a circular motion similar to that which occurs during rotational movements of the head.
Before loading of the specimens, we measured flexion/extension, lateral bending and rotation using a spine tester. In this study, we were able to confirm that specimens with lag screw osteosynthesis do not result in any significant limitation of movement compared to physiological preparations. Specimens that were fused by a dorsal C1/2 spondylodesis tended toward zero with their degree of movement in all directions.
After loading of all specimens in a cyclic loading test, similar results were found in both groups operated on. A difference of 15% in favor of the Harms group, which was statistically not significant, could only be detected in the postinterventional computed tomography.
Regarding the literature and our results, the dorsal C1/2 fusion is the most stable. The cement-augmented odontoid screw osteosynthesis, however, shows similar test values in some phases and has the great advantage that there is no limitation of movement as occurs with the dorsal fusion.
Study limitations
A limitation of the study is that it was not possible to determine the exact time of screw loosening. One possibility would have been to remove the specimen from the cyclic load simulator after each loading cycle and to examine the bone structure around the screw in a micro-CT. This would have made it possible to determine the exact degree of loosening after each cycle. Furthermore, this was not practical because of time constrains and due to the large height of the embedded specimen and the small size of the micro-CT, it was not possible to examine the specimen after each cycle without damaging it further.
Another important limitation is, that our results are only in vitro results and probably cannot directly be transferred to the patient.
Conclusion
A summary of the findings obtained shows that dorsal fusion according to Harms is the more stable construction for the treatment of odontoid type IIb fractures. However, the cement-augmented odontoid screw may show similar values in the load tests with additional preservation of cervical mobility. Accordingly, the cement-augmented lag screw osteosynthesis may be considered in patients with reduced bone density and a type IIb fracture.
In future studies, it would be advisable to examine the data obtained in vivo. In two prospective, randomized groups (cement-augmented lag screw vs. dorsal fusion) of geriatric patients with reduced bone mineral density and a type IIb fracture, quality of life, fusion rates, mortality/morbidity rates should be compared.
References
Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Beiner JM, Albert TJ, Fehlings MG, Vaccaro AR (2005) Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J 5:123–129. https://doi.org/10.1016/j.spinee.2004.09.014
Sarode DP, Demetriades AK (2018) Surgical versus nonsurgical management for type II odontoid fractures in the elderly population: a systematic review. Spine J 18:1921–1933. https://doi.org/10.1016/j.spinee.2018.05.017
Shen Y, Miao J, Li C, Fang L, Cao S, Zhang M, Yan J, Kuang Y (2015) A meta-analysis of the fusion rate from surgical treatment for odontoid factures: anterior odontoid screw versus posterior C1–C2 arthrodesis. Eur Spine J 24:1649–1657. https://doi.org/10.1007/s00586-015-3893-2
Harms J, Melcher RP (2001) Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine 26:2467–2471. https://doi.org/10.1097/00007632-200111150-00014
Jeanneret B, Magerl F (1992) Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord 5:464–475. https://doi.org/10.1097/00002517-199212000-00012
Rizvi SA, Fredo HL, Lied B, Nakstad PH, Ronning P, Helseth E (2012) Surgical management of acute odontoid fractures: surgery-related complications and long-term outcomes in a consecutive series of 97 patients. J Trauma Acute Care Surg 72:682–690. https://doi.org/10.1097/TA.0b013e318236b675
Waschke A, Berger-Roscher N, Kielstein H, Ewald C, Kalff R, Wilke HJ (2015) Cement augmented anterior odontoid screw fixation is biomechanically advantageous in osteoporotic patients with Anderson type II fractures. J Spinal Disord Tech 28:E126-132. https://doi.org/10.1097/BSD.0000000000000177
Wilke HJ, Claes L, Schmitt H, Wolf S (1994) A universal spine tester for in vitro experiments with muscle force simulation. Eur Spine J 3:91–97. https://doi.org/10.1007/bf02221446
Wilke HJ, Wenger K, Claes L (1998) Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J 7:148–154. https://doi.org/10.1007/s005860050045
Kettler A, Schmoelz W, Shezifi Y, Ohana N, Ben-Arye A, Claes L, Wilke HJ (2006) Biomechanical performance of the new BeadEx implant in the treatment of osteoporotic vertebral body compression fractures: restoration and maintenance of height and stability. Clin Biomech 21:676–682. https://doi.org/10.1016/j.clinbiomech.2006.02.005
Wilke HJ, Mehnert U, Claes LE, Bierschneider MM, Jaksche H, Boszczyk BM (2006) Biomechanical evaluation of vertebroplasty and kyphoplasty with polymethyl methacrylate or calcium phosphate cement under cyclic loading. Spine 31:2934–2941. https://doi.org/10.1097/01.brs.0000248423.28511.44
Liebsch C, Zimmermann J, Graf N, Schilling C, Wilke HJ, Kienle A (2018) In vitro validation of a novel mechanical model for testing the anchorage capacity of pedicle screws using physiological load application. J Mech Behav Biomed Mater 77:578–585. https://doi.org/10.1016/j.jmbbm.2017.10.030
Deng H, Yue JK, Upadhyayula PS, Burke JF, Suen CG, Chan AK, Winkler EA, Dhall SS (2016) Odontoid fractures in the octogenarian: a systematic review and meta-analysis. J Neurosurg Sci 60:543–555
Smith HE, Kerr SM, Maltenfort M, Chaudhry S, Norton R, Albert TJ, Harrop J, Hilibrand AS, Anderson DG, Kopjar B, Brodke DS, Wang JC, Fehlings MG, Chapman JR, Patel A, Arnold PM, Vaccaro AR (2008) Early complications of surgical versus conservative treatment of isolated type II odontoid fractures in octogenarians: a retrospective cohort study. J Spinal Disord Tech 21:535–539. https://doi.org/10.1097/BSD.0b013e318163570b
Iyer S, Hurlbert RJ, Albert TJ (2018) Management of odontoid fractures in the elderly: a review of the literature and an evidence-based treatment algorithm. Neurosurgery 82:419–430. https://doi.org/10.1093/neuros/nyx546
Weller SJ, Malek AM, Rossitch E Jr (1997) Cervical spine fractures in the elderly. Surg Neurol 47:274–280. https://doi.org/10.1016/s0090-3019(96)00362-x
Muller EJ, Wick M, Russe O, Muhr G (1999) Management of odontoid fractures in the elderly. Eur Spine J 8:360–365. https://doi.org/10.1007/s005860050188
Robinson Y, Robinson AL, Olerud C (2014) Systematic review on surgical and nonsurgical treatment of type II odontoid fractures in the elderly. Biomed Res Int 2014:231948. https://doi.org/10.1155/2014/231948
Wagner SC, Schroeder GD, Kepler CK, Schupper AJ, Kandziora F, Vialle EN, Oner C, Fehlings MG, Vaccaro AR (2017) Controversies in the Management of Geriatric Odontoid Fractures. J Orthop Trauma 31:S44–S48. https://doi.org/10.1097/BOT.0000000000000948
Lohrer L, Raschke MJ, Thiesen D, Hartensuer R, Surke C, Ochman S, Vordemvenne T (2012) Current concepts in the treatment of Anderson type II odontoid fractures in the elderly in Germany, Austria and Switzerland. Injury 43:462–469. https://doi.org/10.1016/j.injury.2011.09.025
Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI (2010) Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine 12:1–8. https://doi.org/10.3171/2009.7.SPINE08589
Schwarz F, Lawson McLean A, Waschke A, Kalff R (2018) Cement-augmented anterior odontoid screw fixation in elderly patients with odontoid fracture. Clin Neurol Neurosurg 175:144–148. https://doi.org/10.1016/j.clineuro.2018.11.005
Waschke A, Ullrich B, Kalff R, Schwarz F (2016) Cement-augmented anterior odontoid screw fixation for osteoporotic type II odontoid fractures in elderly patients: prospective evaluation of 11 patients. Eur Spine J 25:115–121. https://doi.org/10.1007/s00586-015-4084-x
Funding
Open Access funding enabled and organized by Projekt DEAL. This project was funded by the German Spine Foundation (Grant no. 2015-03) (“Deutsche Wirbelsäulenstiftung”).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by FS, CL, NBR, YS and AW. The first draft of the manuscript was written by FS and reviewed by all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the local ethic committee (Number: 2020-1763).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schwarz, F., Liebsch, C., Berger-Roscher, N. et al. A biomechanical comparison of a cement-augmented odontoid screw with a posterior-instrumented fusion in geriatric patients with an odontoid fracture type IIb. Eur Spine J 30, 1566–1573 (2021). https://doi.org/10.1007/s00586-021-06848-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06848-7