Abstract
Purpose
Factors influencing paraspinal muscle degeneration are still not well understood. Fatty infiltration is known to be one main feature of the degeneration cascade. The aim of this cross-sectional study was to illustrate the 3D cluster of paraspinal lumbar muscle degeneration on T2-weighted MRI images using our newly developed software application ‘iSix’.
Methods
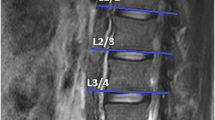
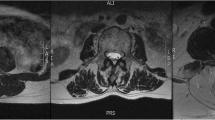
Mono- (Mm. rotatores), multi- (Mm. multifidus) and pluri-segmental (M. erector spinae) lumbar muscles groups were segmented on T2-weighted MR sequences using a novel computer-assisted technique for quantitative muscle/fat discrimination. The degree of fatty infiltration of the three predefined muscle groups was compared on a 3-dimensional basis, with regard to segment involvement and age. General linear models were utilized for statistical comparison.
Results
N = 120 segments (age: 52.7; range 16—87 years) could be included. The overall relative fatty infiltration of the mono-segmental muscles was higher (21.1 14.5%) compared to the multi-segmental (16.0 8.8% p = 0.049) and pluri-segmental muscles (8.5 8.0%; p = 0.03). Mono-segmental muscles on the levels L4/5 (22.9 ± 10.2 [CI 17.6–28.2] %) and L5/S1 (27.01 ± 15.1 [CI 21.4–32.7] %) showed a significant higher amount of fat compared to the levels L2/3 (8.2 ± 6.8 [CI 2.2–14.2] %; L4/5 vs. L2/3, p = 0.03; L5/S1 vs. L2/3, p = 0.02) and L3/4 (13.2 ± 5.4 [CI 8.6–17.7]%; L4/5 vs. L3/4, p = 0.02; L5/S1 vs. L3/4, p < 0.01). Multivariate linear regression analyses revealed age and Pfirrmann grade as independent factors for fatty muscle degeneration.
Conclusions
3D analysis of fatty infiltration is an innovative tool to study lumbar muscle degeneration. Mono-segmental muscles are more severely affected by degeneration compared to multi-/pluri-segmental muscles, especially at the L4/5 and L5/S1 level. Age and disc degeneration independently correlate with muscle degeneration.





Similar content being viewed by others
Code availability
Please contact the corresponding author.
References
Teichtahl AJ, Urquhart DM, Wang Y et al (2015) Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J 15:1593–1601. https://doi.org/10.1016/j.spinee.2015.03.039
Andersson GBJ (1999) Epidemiological features of chronic low-back pain. Lancet 354:581–585
Ward SR, Kim CW, Eng CM et al (2009) Architectural analysis and intraoperative measurements demonstrate the unique design of the multifidus muscle for lumbar spine stability. J Bone Jt Surg—Ser A. https://doi.org/10.2106/JBJS.G.01311
Kulig K, Scheid AR, Beauregard R et al (2009) Multifidus morphology in persons scheduled for single-level lumbar microdiscectomy: qualitative and quantitative assessment with anatomical correlates. Am J Phys Med Rehabil 88:355–361. https://doi.org/10.1097/PHM.0b013e31819c506d
Freeman MD, Woodham MA, Woodham AW (2010) The Role of the lumbar multifidus in chronic low back pain: a review. PM R 2:142–146. https://doi.org/10.1016/j.pmrj.2009.11.006
Takayama K, Kita T, Nakamura H et al (2016) New predictive index for lumbar paraspinal muscle degeneration associated with aging. Spine (Phila Pa 1976) 41:E84–E90. https://doi.org/10.1097/BRS.0000000000001154
Shahidi B, Parra CL, Berry DB et al (2017) Contribution of lumbar spine pathology and age to paraspinal muscle size and fatty infiltration. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000001848
Jun HS, Kim JH, Ahn JH et al (2016) The effect of lumbar spinal muscle on spinal sagittal alignment: evaluating muscle quantity and quality. Neurosurgery. https://doi.org/10.1227/NEU.0000000000001269
Lee SH, Park SW, Kim YB et al (2017) The fatty degeneration of lumbar paraspinal muscles on computed tomography scan according to age and disc level. Spine J 17:81–87. https://doi.org/10.1016/j.spinee.2016.08.001
Teichtahl AJ, Urquhart DM, Wang Y et al (2016) Lumbar disc degeneration is associated with modic change and high paraspinal fat content—a 3.0T magnetic resonance imaging study. BMC Musculoskelet Disord 17:1–7. https://doi.org/10.1186/s12891-016-1297-z
Rossi A, Zoico E, Goodpaster BH et al (2010) Quantification of intermuscular adipose tissue in the erector spinae muscle by MRI: agreement with histological evaluation. Obesity 18:2379–2384. https://doi.org/10.1038/oby.2010.48
Bierry G, Kremer S, Kellner F et al (2008) Disorders of paravertebral lumbar muscles: from pathology to cross-sectional imaging. Skeletal Radiol 37:967–977. https://doi.org/10.1007/s00256-008-0494-8
Ferguson S (2008) Biomechanics of the spine. In: Boos N, Aebi M (eds) Spinal disorders, fundamentals of diagnosis and treatment. Springer, Berlin, Heidelberg, pp 41–66
Faur C, Patrascu JM, Haragus H, Anglitoiu B (2019) Correlation between multifidus fatty atrophy and lumbar disc degeneration in low back pain. BMC Musculoskelet Disord 20:414. https://doi.org/10.1186/s12891-019-2786-7
Urrutia J, Besa P, Lobos D et al (2018) Lumbar paraspinal muscle fat infiltration is independently associated with sex, age, and inter-vertebral disc degeneration in symptomatic patients. Skeletal Radiol 47:955–961. https://doi.org/10.1007/s00256-018-2880-1
Goubert D, van Oosterwijck J, Meeus M, Danneels L (2016) Structural changes of lumbar muscles in non-specific low back pain. Pain Physician 19:E985–E1000
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis. Age Ageing 39:412–423. https://doi.org/10.1093/ageing/afq034
Hirschfeld HP, Kinsella R, Duque G (2017) Osteosarcopenia: where bone, muscle, and fat collide. Osteoporos Int 28:2781–2790. https://doi.org/10.1007/s00198-017-4151-8
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoppe, S., Maurer, D., Valenzuela, W. et al. 3D analysis of fatty infiltration of the paravertebral lumbar muscles using T2 images—a new approach. Eur Spine J 30, 2570–2576 (2021). https://doi.org/10.1007/s00586-021-06810-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06810-7