Abstract
Purpose
Patients with chronic low back pain, who do not respond to conservative treatment methods, generally undergo surgical revision operations, and sometimes an undesirable condition called failed back surgery syndrome (FBSS) may be inevitable. Hereby, dextrose is one of the regenerative methods that has gained popularity in the treatment of many musculoskeletal problems, and we aimed to present and evaluate the outcomes of 5% dextrose for the treatment of FBSS.
Methods
It has been designed as a consecutive case series. A total of 79 patients with FBSS, who had minimum 6 months of symptoms and did not respond to 3 months of conservative methods between May 2014 and March 2016, participated in the study. Prolotherapy injections were applied in posterior and lateral approaches. Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) were used for the pre- and post-treatment evaluations. Patient satisfaction was assessed with using a 5-point Likert scale by phone contacting.
Results
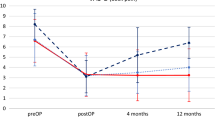
There was statistically significant difference between repeated VAS and ODI measurements.
Conclusions
These results may be the first step giving a lead to an undiscovered field. This treatment method should be kept in mind for FBSS patients before giving a decision of revision surgery.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.



Similar content being viewed by others
References
Dagenais S, Caro J, Haldeman S (2008) A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 8(1):8–20. https://doi.org/10.1016/j.spinee.2007.10.005
Schofferman J, Reynolds J, Herzog R et al (2003) Failed back surgery: etiology and diagnostic evaluation. Spine J 3(5):400–403
Chan C-W, Peng P (2011) Failed back surgery syndrome. Pain Med 12:577–606
Hussain A, Erdek M (2014) Interventional pain management for failed back surgery syndrome. Pain Pract 14:64–78
Choi HS, Chi EH, Kim MR et al (2014) Demographic characteristics and medical service use of failed back surgery syndrome patients at an integrated treatment hospital focusing on complementary and alternative medicine: a retrospective review of electronic medical records. Evid Based Complement Altern Med 2014:714389
Shapiro C (2014) The failed back surgery syndrome: pitfalls surrounding evaluation and treatment. Phys Med Rehabil Clin N Am 25(2):319–340
Hazard RG (2006) Failed back surgery syndrome: surgical and nonsurgical approaches. Clin Orthop Relat Res 443:228–232
Weir S, Samnaliev M, Kuo TC et al (2017) The rate of persistent post-operative pain (FBSS) in revision lumbar spinal surgery. Spine J 17(3):S10
Tronnier VM, Eldabe S, Franke J, Huygen F, de Andres Rigoard P, Ares J et al (2018) The appropriate management of persisting pain after spine surgery: a European panel study with recommendations based on the RAND/UCLA method. Eur Spine J 28(1):31–45. https://doi.org/10.1007/s00586-018-5711-0
Seven MM, Ersen O, Akpancar S et al (2017) Effectiveness of prolotherapy in the treatment of chronic rotator cuff lesions. Orthop Traumatol Surg Res 103(3):427–433
Ersen O, Koca K, Akpancar S et al (2017) A randomized-controlled trial of prolotherapy injections in the treatment of plantar fasciitis. Turk J Phys Med Rehab 64(1):i–xi
Akpancar S, Seven MM, Tuzun HY et al (2017) Current concepts of prolotherapy in orthopedic surgery. Arch Trauma Res 6(2):e40447
Rabago D, Slattengren A, Zgierska A (2010) Prolotherapy in primary care practice. Prim Care 37(1):65–80
Reeves KD, Topol GA, Fullerton BD (2008) Evidence-based regenerative injection therapy (prolotherapy) in sports medicine. In: Seidelberg PH, Beutler PL (eds) The sports medicine resource manual. Saunders, Philadelphia, pp 611–619
Di Paolo S, Gesualdo L, Ranieri E, Grandaliano G, Schena FP (1996) High glucose concentration induces the overexpression of transforming growth factor-beta through the activation of a platelet-derived growth factor loop in human mesangial cells. Am J Pathol. 149(6):2095–2106
Murphy M, Godson C, Cannon S, Kato S, Mackenzie HS, Martin F et al (1999) Suppression subtractive hybridization identifies high glucose levels as a stimulus for expression of connective tissue growth factor and other genes in human mesangial cells. J Biol Chem. 274(9):5830–5834
Krump E, Nikitas K, Grinstein S (1997) Induction of tyrosine phosphorylation and Na+/H+ exchanger activation during shrinkage of human neutrophils. J Biol Chem 272(28):17303–17311
Lyftogt J (2008) Pain conundrums: which hypothesis? Central nervous system sensitization versus peripheral nervous system autonomy. Aust Musculoskelet Med 13(2):72
Sanderson LM, Bryant A (2015) Effectiveness and safety of prolotherapy injections for management of lower limb tendinopathy and fasciopathy: a systematic review. J Foot Ankle Res 8:57. https://doi.org/10.1186/s13047-015-0114-5
Maniquis-Smigel L, Dean Reeves K, Jeffrey Rosen H et al (2017) Short term analgesic effects of 5% dextrose epidural injections for chronic low back pain: a randomized controlled trial. Anesthesiol Pain Med 7(1):e42550. https://doi.org/10.5812/aapm.42550
Yelland MJ, Glasziou PP, Bogduk N, et al (2004) Prolotherapy injections, saline injections, and exercises for chronic low-back pain: a randomized trial. Spine (Phila Pa 1976) 29(1):9–16 (discussion 16)
Dagenais S, Yelland MJ, Del Mar C, Schoene ML (2007) Prolotherapy injections for chronic low-back pain. Cochrane Database Syst Rev. 18(2):CD004059.
Guran S, Coban ZD, Karasimav O et al (2018) Dextrose solution used for prolotherapy decreases cell viability and increases gene expressions of angiogenic and apopitotic factors. Gulhane Med J 60:42
Hackett GS, Hemwall GA, Montgomery GA (1993) Ligament and tendon relaxation treated by prolotherapy, 5th edn. Gustav A. Hemwall, Oak Park
Fairbank JCT, Pynsent PB (2000) The oswestry disability index. Spine 25(22):2940–2953
Jamieson S (2004) Likert scales: how to (ab)use them. Med Educ 38(12):1217–1218
Lee JH, Lee SH (2014) Clinical effectiveness of percutaneous adhesiolysis versus transforaminal epidural steroid injection in patients with postlumbar surgery syndrome. Reg Anesth Pain Med 39:214–218
Hollingworth W, Turner JA, Welton NJ et al (2011) Costs and cost effectiveness of spinal cord stimulation (SCS) for failed back surgery syndrome. Spine 36:2076–2083
Lad SP, Babu R, Bagley JH et al (2014) Utilization of spinal cord stimulation in patients with failed back surgery syndrome. Spine 39:E719–E727
North RB, Kidd D, Shipley J et al (2007) Spinal cord stimulation versus reoperation for failed back surgery syndrome: a cost effectiveness and cost utility analysis based on a randomized, controlled trial. Neurosurgery 61:361–368
Manchikanti L, Abdi S, Atluri S et al (2013) An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician 16:S49–283
Chun-jing J, Hao-xiong N, Jia-ziang N (2012) The application of percutaneous lysis of epidural adhesions in patients with failed back surgery syndrome. Acta Cir Bras 27:357–362
Manchikanti L, Boswell MV, Datta S et al (2009) Comprehensive review of therapeutic interventions in managing chronic spinal pain. Pain Physician 12:E123–E198
Fritsch EW, Heisel J, Rupp S (1996) The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine (Phila Pa 1976) 21: 626–633
Amirdelfan K, Webster L, Poree L et al (2017) Treatment options for failed back surgery syndrome patients with refractory chronic pain: an evidence based approach. Spine 42:S41–S52
Louw A, Diener I, Landers MR et al (2014) Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1-year follow-up. Spine (Phila Pa 1976) 39:1449–1457
Brox JI, Reikeras O, Nygaard O et al (2006) Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: a prospective randomized controlled study. Pain 122:145–155
Jensen KT, Rabago DP, Best TM et al (2008) Early inflammatory response of knee ligaments to prolotherapy in a rat model. J Orthop Res 26(6):816–823. https://doi.org/10.1002/jor.20600
Thomson S, Jacques L (2009) Demographic characteristics of patients with severe neuropathic pain secondary to failed back surgery syndrome (PROCESS study). Pain Pract 9:206–214
Drucker M, Cardenas E, Arizti P et al (1998) Experimental studies on the effect of lidocaine on wound healing. World J Surg. 22(4):394–397 (discussion 397–8)
Kim MY, Na YM, Moon JH (1997) Comparison on treatment effects of dextrose water, saline, and lidocaine for trigger point injection. J Korean Acad Rehabil Med 21(5):967–973
Rabago D, Kijowski R, Woods M et al (2013) Association between disease-specific quality of life and magnetic resonance imaging outcomes in a clinical trial of prolotherapy for knee osteoarthritis. Arch Phys Med Rehabil 94(11):2075–2082
Panjabi M, Abumi K, Duranceau J et al (1989) Spinal stability and intersegmental muscle forces. A biomechanical model. Spine 14(2):194–200
Clemente CD (1985) Gray’s Anatomy, 30th edn. Lea & Febiger, Philadelphia
Yelland M, Glasziou P, Bogduk N, Schluter P, McKernon M (2004) Prolotherapy injections, saline injections, and exercises for chronic low back pain: a randomized trial. Spine 29(1):9–16
Acknowledgements
We all thank Michael Yelland, Associate Professor, MD, and John Lyftogt, MD, for their respected contributions to the designation of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
İlker Solmaz, Serkan Akpancar, Aydan Örsçelik, Özlem Yener-Karasimav and Deniz Gül declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Solmaz, İ., Akpancar, S., Örsçelik, A. et al. Dextrose injections for failed back surgery syndrome: a consecutive case series. Eur Spine J 28, 1610–1617 (2019). https://doi.org/10.1007/s00586-019-06011-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06011-3