Abstract
Purpose
The aim is to analyze the agreement between different types of physicians in terms of the inter-observer and intra-observer reliability in addition to the agreement between the experienced and non-experienced physicians with respect to three different classification systems for diagnosis of cervical spinal canal stenosis.
Methods
Total nine doctors including experienced group of three doctors and non-experienced group of six doctors classified the patients according to three different classification in an independent, blinded manner using magnetic resonance imaging (MRI) to diagnose cervical canal stenosis. MRI slice included sagittal plane (midline cut) and an image slice from each horizontal plane that penetrated the right center of each disk (C3–4, C4–5, C5–6, and C6–7) was made by PPT format.
Results
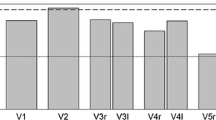
For the inter-observer reliability, Vaccaro et al.’s classification system showed the excellent reproducibility, followed by Muhle et al. and Kang et al. All three classification systems showed excellent reproducibility and substantial agreement in terms of the intra-observer reliability.
Conclusions
All three classification systems showed excellent reproducibility and also displayed a substantial agreement. The classification system used by Vaccaro et al. was proven to be a method with substantial agreement both in the experienced group and the non-experienced group. It can be a useful classification system for simplifying communication among all physicians.

Similar content being viewed by others
References
Meyer F, Börm W, Thomé C (2008) Degenerative cervical spinal stenosis. Current strategies in diagnosis and treatment. Dtsch Arztebl Int 105:366–372
Freeman BA, Hoffler CE II, Cameron BM, Rhee JM, Bawa M, Malone DG et al (2015) A comparison of computed tomography measures for diagnosing cervical spinal stenosis associated with myelopathy: a case–control study. Asian Spine J 9:22–29
Teresi LM, Lufkin RB, Relcher MA, Moffit BJ, Vinuela FV, Wilson GM et al (1987) Asymptomatic degenerative disc disease and spondylosis of the cervical spine: MR imaging. Radiology 164:83–88
Muhle C, Metzner J, Weinert D, Falliner A, Brinkmann G, Mehdorn MH et al (1998) Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. Am J Neuroradiol 19:1763–1771
Edwards CC 2nd, Riew KD, Anderson PA, Hillibrand AS, Vaccaro AF (2003) Cervical myelopathy. Current diagnostic and treatment strategies. Spine J 3:68–81
Radcliff K, Kepler C, Sidhu G, Albert T, Hillibrand A, Anderson DG et al (2012) A novel, anatomically based classification of cervical stenosis. CSRS Resource Center. http://www.csrs.org/clinical-validation-of-a-novel-anatomically-based-classification-of-cervical-stenosis/
Kang YS, Lee JW, Koh YH, Hur SB, Kim SJ, Chai JW et al (2011) New MRI grading system for the cervical canal stenosis. Am J Roentgenol 197:134–140
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Lee MJ, Cassinelli EH, Riew KD (2007) Prevalence of cervical spine stenosis: anatomic study in cadavers. J Bone Joint Surg Am 89:376–380
Kang JD, Figgie MP, Bohlman HH (1994) Sagittal measurements of the cervical spine in subaxial fractures and dislocations. An analysis of two hundred and eighty-eight patients with and without neurological deficits. J Bone Joint Surg Am 76:1617–1628
Torg JS, Naranja RJ Jr, Pavlov H, Galinat BJ, Warren R, Stine RA (1996) The relationship of developmental narrowing of the cervical spinal canal to reversible and irreversible injury of the cervical spinal cord in football players. J Bone Joint Surg Am 78:1308–1314
Gore DR (2001) Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine 26:2463–2466
Boden SD, Dodge LD, Bohlman HH, Rechtine GR (1993) Rheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recovery. J Bone Joint Surg Am 75:1282–1297
Murone I (1974) The importance of the sagittal diameters of the cervical spinal canal in relation to spondylosis and myelopathy. J Bone Joint Surg Br 56:30–36
Nakashima H, Yukawa Y, Suda K, Yamagata M, Ueta T, Kato F (2016) Narrow cervical canal in 1211 asymptomatic healthy subjects: the relationship with spinal cord compression on MRI. Eur Spine J 25:2149–2154
Pavlov H, Torg JS, Robie B, Jahre C (1987) Cervical spinal stenosis: determination with vertebral body ratio method. Radiology 164:771–775
Rüegg TB, Wicki AG, Aebli N, Wisianowsky C, Krebs J (2015) The diagnostic value of magnetic resonance imaging measurements for assessing cervical spinal canal stenosis. J Neurosurg Spine 22:230–236
Kadanka Z, Bednarík J, Vohánka S, Vlach O, Stejskal L, Chaloupka R et al (2000) Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomized study. Eur Spine J 9:538–544
Kadaňka Z, Bednařík J, Novotný O, Urbánek I, Dusek L (2011) Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J 20:1533–1538
Rhee JM, Shamji MF, Erwin MW, Bransford RJ, Yoon ST, Smith JS et al (2013) Nonoperative management of cervical myelopathy: a systematic review. Spine 38:S55–S67
Edwards WC, LaRocca SH (1983) The development segmental sagittal diameter of the cervical spinal canal in patients with cervical spondylosis. Spine 8:20–27
Lim JK, Wong HK (2004) Variation of the cervical spinal Torg ratio with gender and ethnicity. Spine J 4:396–401
Tierney RT, Maldjian C, Mattacola CG, Straub SJ, Sitler MR (2002) Cervical spine stenosis measures in normal subjects. J Athl Train 37:190–193
Prasad SS, O’Malley M, Caplan M, Shackleford IM, Pydisetty RK (2003) MRI measurements of the cervical spine and their correlation to Pavlov’s ratio. Spine 28:1263–1268
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Ko, S., Choi, W. & Chae, S. Comparison of inter- and intra-observer reliability among the three classification systems for cervical spinal canal stenosis. Eur Spine J 26, 2290–2296 (2017). https://doi.org/10.1007/s00586-017-5187-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5187-3