Abstract
Purpose
Surgery for aneurysmal clipping after subarachnoid haemorrhage (SAH) poses a unique anaesthetic challenge. However, data on the influence of anaesthetic agents in these patients are lacking. The study aims to evaluate the superiority of propofol over desflurane for postanaesthetic morbidity in patients undergoing surgery following aneurysmal SAH.
Methods
Seventy World Federation of Neurosurgeons Grade I and II patients were randomized into propofol (n = 35) and desflurane groups (n = 35). Anaesthesia was maintained with propofol/fentanyl in propofol group and desflurane/fentanyl in the desflurane group. Jugular venous oxygen saturation (SjVO2) and brain relaxation were assessed intraoperatively. Time to eye opening, response to verbal commands, and extubation were noted from the time of discontinuing the anaesthetic agent. Duration of postoperative hospital stay and modified Rankin score (MRS) at discharge were subsequently compared.
Results
Median postoperative hospital stay was 9 (6, 14) days with use of propofol and 9 (7, 12) days in desflurane group (P = 0.671). 18 patients in the propofol group and 14 patients in the desflurane group had good outcome (modified Rankin score 0–1; P = 0.453). Both the anaesthetics were similar in terms of intraoperative haemodynamics, brain relaxation, time to eye opening, response to verbal commands, and extubation time (P > 0.05). Emergence hypertension was more in the desflurane group (P = 0.007). The intraoperative SjVO2 values were significantly higher in the desflurane group (P < 0.05).
Conclusion
Propofol and desflurane are comparable in terms of postoperative morbidity in patients undergoing aneurysm neck clipping following SAH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Annual incidence of subarachnoid haemorrhage (SAH) following rupture of cerebral aneurysms is approximately 5–11/100,000 [1]. Case fatality is approximately 50% and one-third of survivors remain dependant [2]. The patients scheduled for clipping of aneurysmal neck following SAH undergo early surgery to prevent rebleeding [3]. During this period, there are ongoing consequences of acute neurological insult [4]. Since intravenous and inhalational anaesthetics have variable effects on cerebral physiology, they have the potential to influence the outcome in patients undergoing surgery during acute phase of aneurysmal SAH.
Goals of anaesthesia during aneurysmal neck clipping following SAH are to maintain cerebral perfusion, facilitate brain relaxation, and reduce transmural pressure during dissection around the aneurysm. The anaesthetics should also facilitate prompt awakening and neurological assessment following surgery. Both inhalational as well as intravenous agents are being used for maintenance of anaesthesia but data comparing the two in terms of outcome in this subset of patients is lacking.
Propofol has been a popular drug for neurosurgery since its first clinical trial in 1977 [5]. Rapid return to consciousness after discontinuation of continuous infusion is a major advantage in comparison with other agents. Propofol reduces the Cerebral metabolic requirement of oxygen (CMRO2), reduces the cerebral blood flow (CBF), preserves cerebrovascular reactivity to changes in carbon-di-oxide levels, and offers neuroprotection [6, 7]. Desflurane has been in use for maintenance of anaesthesia since 1992. Its solubility characteristics and potency permit rapid achievement of anaesthesia as well as prompt awakening. Desflurane also reduces the CMRO2, preserves cerebrovascular reactivity, and has been found to offer neuroprotection in various in vivo and in vitro models [8, 9]. However, it is seen that the reduction in CBF caused by desflurane due to concomitant reduction in CMRO2 may be offset by direct cerebral vasodilatory properties [10]. This property of desflurane may increase the ICP and aggravate preexisting neurological insult when compared to propofol which has cerebral vasoconstrictive properties. One study comparing perioperative outcome with the use of burst suppression doses of propofol and desflurane found similar brain conditions and awakening times in patients undergoing clipping following aneurysmal SAH [11]. However, when used at maintenance doses for anaesthesia, the neurological outcome at hospital discharge is improved with the use of propofol [12].
Considering the above factors, it appears that at anaesthetic doses, propofol may offer better neuroprotection than desflurane in influencing the postoperative outcome of these patients. The aim of the present study is to evaluate the superiority of propofol for short-term outcome when compared to desflurane in patients undergoing surgery for clipping of cerebral aneurysm following SAH. The comparison of duration of postoperative hospital stay as a surrogate marker of morbidity was the primary outcome. Comparison of intraoperative haemodynamics, brain relaxation, jugular venous oxygen saturation (SjVO2), emergence characteristics, and neurological outcome at discharge were the secondary outcomes of the study.
Methods
After approval from institutional ethical committee, this prospective randomized study was conducted in patients undergoing aneurysmal neck clipping following spontaneous rupture of intracranial aneurysm in the anterior cerebral circulation. Patients included were between 18 and 65 years of age, World Federation of Neurosurgeons (WFNS) Grade I–II, ASA physical status I–III, diameter of ruptured aneurysm less than 25 mm and duration of surgery less than 5 h. Patients with aneurysm in the posterior circulation and also the ones with illness like coronary artery disease, valvular disorder, hepatic, and renal impairment were not included in the study. 70 patients were randomized into propofol (n = 35) and desflurane (n = 35) groups using computer generated random tables and concealment done using opaque sealed envelope by the corresponding author who was not involved in conduct of anaesthesia for the included patients. Written informed consent was taken from the patient or next of kin. The trial was registered with Clinical Trials Registry, India (http://ctri.nic.in. Unique identifier: CTRI/2014/10/005118).
Preinduction monitoring included noninvasive blood pressure, electrocardiography, pulse oximetry, and urine output. The patients were administered fentanyl 2 µg/kg prior to induction followed by 0.5–2 µg/kg/h as infusion. Propofol was used for induction of anaesthesia with the dose titrated to loss of response to verbal command. Lignocaine 1.5 mg/kg was administered prior to laryngoscopy to attenuate the hemodynamic stress response. Vecuronium was used for intubation in the doses of 0.1 mg/kg and subsequently 0.02 mg/kg to maintain less than two twitches on the ‘Train of Four’ neuromuscular monitor. For beat to beat monitoring of blood pressure and blood gas analysis, an arterial catheter was placed in the radial artery. Nasopharyngeal thermometer probe was placed to measure the body temperature and normothermia (36–37 °C) maintained in all the patients with the help of forced air-warming blankets. The patients were maintained with either propofol infusion or desflurane. ENTROPY™ (Datex-Ohmeda) was used to maintain comparable depth of anaesthesia in both the groups. Propofol and desflurane were titrated to maintain state entropy values between 40 and 60.
Normal saline was used as intraoperative fluid. Packed red blood cells were administered if hematocrit reduced to less than 30. Mannitol 0.5 gm/kg was administered at the time of skin incision. PaCO2 was kept between 32 and 35 mmHg, but patients were hyperventilated to a PaCO2 of 28–32 mmHg if the brain swelling persisted despite osmotic therapy. Ventilation was maintained with 100% oxygen in all the patients. Fentanyl infusion was stopped at the beginning of scalp closure, whereas anaesthetic agents were stopped after application of staples for skin closure. Neuromuscular blockade was reversed with a combination of neostigmine 50 µg/kg and glycopyrrolate 10 µg/kg. The patients were extubated if (1) they were haemodynamically stable; (2) there was adequate reversal of neuromuscular blockade; (3) return of spontaneous and regular respiration with adequate tidal volume; (4) ability to maintain adequate oxygen saturation; and (5) there was spontaneous eye opening or response to verbal commands. Total duration from the time of induction until the time of cessation of the anaesthetic agent (i.e., after the application of skin staples for scalp closure) was noted as duration of anaesthesia. This included the time required for insertion of intra arterial and jugular bulb catheter, positioning of the patient and complete duration of surgery. The duration of surgery was the time from scalp incision until the time of complete closure of scalp incision.
With the patients lying undisturbed in the operative room, the preinduction heart rate and blood pressure were recorded thrice at 1 min interval. The mean of the three readings was taken as the baseline value of heart rate and blood pressure for a particular patient. Subsequently, patient's heart rate and blood pressure were kept as close to baseline as possible during the conduct of the procedure. Prior to application of temporary clip, the mean blood pressure was increased to 20% of the baseline values to augment collateral blood flow. Any sustained increase or decrease in blood pressure during the course of surgery which was more than 20% than the baseline was managed aggressively with the use of beta-blockers (Metoprolol) for hypertension and vasopressors (Dopamine) for hypotension. Any adverse intraoperative event leading to major haemodynamic instability resulted in exclusion of the patient from the study. After craniotomy, scoring for brain relaxation was done by the neurosurgeon who was unaware of the agent used for maintenance of anaesthesia. Brain relaxation was graded as Grade 1—relaxed brain, Grade 2—tense brain with mild but acceptable swelling, Grade 3—tight brain with moderate brain swelling but no specific change in management required, and Grade 4—bulging brain with severe swelling requiring some specific change in management (e.g., administration of additional doses of mannitol, boluses of propofol, etc.).
Jugular bulb oximetry was done using a 5 Fr, 20 cm, single lumen central venous catheter (CVC), inserted in the internal jugular vein (IJV) ipsilateral to the lesion. The tip of the CVC was placed in the jugular bulb by retrograde cannulation of IJV following tracheal intubation. Intermittent sampling was done immediately after insertion and thereafter following craniotomy, permanent clipping, closure of duramater and following extubation. Confirmation of correct placement was done postoperatively by skull and neck radiography. If the tip of the catheter was not in correct position, the data of SjVO2 values were excluded but the patient continued to be a part of the study for other parameters.
Following discontinuation of anaesthetic agent, time to eye opening, response to verbal commands and extubation were compared. Incidence of emergence hypertension (mean arterial pressure more than 20% of baseline sustained for more than 1 min and requiring administration of intravenous Esmolol) and the number of patients who were extubated were noted.
All the patients were reviewed 24 h after surgery for any neurological deficits and the Glasgow Coma Score. Subsequently, they were followed up until the time of discharge from hospital or death. The criterion for discharge of patients were neurological stability (no alteration in the GCS for five successive days), haemodynamic stability, spontaneous breathing, and the ability to maintain oxygen saturation > 95% on room air, accepting feeds either orally or through nasogastric tube and when the patients were free of any infection. The incidence of vasospasm, infarction, decompressive craniectomy, and tracheostomy was also noted. The hospital stay in days after the surgery was compared for both the groups. Patients at the time of discharge were assessed for functional neurological status as per modified Rankin score (MRS) by the neurosurgical residents who were unaware of the agent used for maintenance of anaesthesia. Patients with MRS of 0 and 1 at discharge were considered to have a good outcome, whereas those with MRS of 2–6 were considered to be poor outcome.
Duration of mean hospital stay after clipping is 13.5 days in our institution. Our study hypothesized that propofol could be better than desflurane for outcome in these group of patients. We assumed mean hospital stay to be 13 days when propofol is used and 15 days when desflurane is used. With SD of ± 2.5, a sample size of 25 cases was considered adequate for a study with 80% Power and 95% confidence interval. Adjusting for dropouts, we decided to include 35 patients per group.
Statistical analysis
Normality of quantitative data was checked by measures of Kolmogorov–Smirnov tests of normality. For normally distributed data, means have been compared using unpaired t test and presented as mean ± standard deviation (SD). The variables with skewed data were analysed using Mann–Whitney tests and presented as median and interquartile range (IQR). Categorical variables were analysed using Chi-square test and presented as number and percentages. All calculations are two sided and were performed using Statistical Package for Social Sciences (SPSS Inc. 2013, version 22.0 for Windows, Armonk, NY, USA). A ‘p’ value of < 0.05 has been considered statistically significant.
Results
Out of 118 patients assessed for eligibility, 70 patients were enrolled and randomized into Propofol and Desflurane groups. Both the groups had 35 patients. 2 (5.7%) patients in the propofol group and 4 (11.4%) patients in the Desflurane were excluded during the course of study (Fig. 1). In propofol group, both the patients were excluded due to intraoperative rupture of aneurysm leading to major haemorrhage and hemodynamic instability. Out of the 4 patients excluded in the desflurane group, 3 were excluded due to intraoperative aneurysmal rupture leading to major haemorrhage and hemodynamic instability, whereas 1 patient was excluded due to duration of surgery exceeding 5 h. Hence, 33 patients in the propofol group and 31 patients in the desflurane group were considered for final analysis (Fig. 1). Patient population in both the groups were compared for baseline characteristics and no significant differences were noted (Table 1).
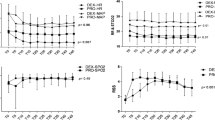
There was no significant difference in variables recorded intraoperatively (Table 2). Data for SjVO2 could be obtained in 13 patients in propofol group and 14 patients in the desflurane group. Sampling was done at five different instances as mentioned in the methodology. The mean values obtained at these five points were analysed for any difference within the individual group as well as in between the two groups. Values in desflurane group were higher than propofol group at all instances when sampling was done. The mean SjVO2 values were 74% or more at any of the five occasions in the desflurane group. However, the values reached statistical significance between the two groups following craniotomy and after clipping of the neck of aneurysm (Fig. 2). Analysing the mean values within the same group, no significant difference was seen at any time when compared to the baseline values which were recorded immediately after insertion of the jugular bulb catheter.
20 patients (60.6%) in the propofol group and 23 patients (74.2%) in the desflurane group were extubated in the operation theatre after the end of surgery. Consequently, the data for emergence characteristics were analysed for 20 patients in propofol group and 23 patients in desflurane group (Table 3). Both the groups were comparable for time to eye opening, time to extubation and time to obeying of verbal commands. The incidence of emergence hypertension was significantly higher in the desflurane group (Table 3).
Patients were evaluated at 24 h after surgery and no statistical difference was found in between the groups in terms of GCS and appearance of new neurological deficits. More number of patients had postoperative mechanical ventilation after 24 h in the propofol group than the desflurane group, but this difference was also statistically insignificant (Table 4). Both the groups were similar for adverse postoperative events which included vasospasm, origin of a new infarct, need for tracheostomy or decompressive craniectomy (Table 4).
Median hospital stay of patients in the propofol group was 9 (6, 14) days which was similar to desflurane group which also had a median hospital stay of 9 (7, 12) days (Table 4). Patient’s condition at the time of discharge was assessed in both the groups using MRS. The distribution of patients in both the groups is shown in Table 4. There is no difference in between the two groups as far as distribution among MRS is considered. The number of patients discharged with good outcome (MRS 0–1) is numerically better in the propofol group but this difference is statistically not significant (Table 4).
Discussion
Both intravenous as well as inhalational agents have been used for maintenance of anaesthesia during neurosurgery [13,14,15]. However, the data comparing various anaesthetic agents specifically for outcome following surgery for aneurysmal neck clipping after SAH is lacking except for a retrospective analysis which found better outcome with the use of propofol [12]. The present study is the first prospective randomized clinical trial which compares the effect of an intravenous with an inhalational anaesthetic for postoperative outcome in patients undergoing surgery following an acute neurological insult due to aneurysmal SAH.
In our study, the duration of postoperative hospital stay has been used as a surrogate marker of short-term outcome. The effect of an individual anaesthetic on the cerebral physiology and neuroprotection can influence the morbidity and postoperative course of a patient. In our study, no appreciable difference was noted in the postoperative hospital stay between the propofol and desflurane groups. The MRS at discharge was also similar among the two groups. Numerically, more patients had good outcome (MRS 0–1) in the propofol group than the desflurane group, but the difference is not statistically significant. Mortality was also similar in both the groups. We also looked at the short-term outcome, in terms of GCS of the patient and presence of any fresh neurological deficit at 24 h after surgery as we felt that early outcome is important in context of the anaesthetic agents used. Majority of the patients in both the groups had a GCS of 15. However, more patients continued to be on ventilator support at 24 h in the propofol group than in the desflurane group. The fact that propofol reduces regional CBF preferentially in the regions implicated for arousal and its elimination half life being 4–7 h may have a minor contributory effect in this regard [16, 17]. Five patients in each group had fresh neurological deficits. Location of the ruptured aneurysm and the surgical technique may be the probable causes for these deficits. The incidence of postoperative complications like cerebral vasospasm, cerebral infarction and those who underwent decompressive craniectomy were also similar among the groups.
An important goal of neuroanaesthesia is to maintain haemodynamic stability and provide a relaxed brain during surgery. Propofol reduces the CMRO2 as well as CBF and is likely to provide a relaxed brain during surgery [18]. Desflurane also reduces CMRO2, but it may not cause a proportionate decrease in CBF, and hence, it appears less favourable for use in neurosurgery [10]. However, our results did not show any difference in the grades of brain swelling in both the group. Majority of patients in both the groups had either a relaxed brain or mild brain swelling. Cheng et al. compared propofol with desflurane for brain relaxation in patients undergoing aneurysm neck clipping surgeries. They found that all the patients in both the propofol and desflurane groups had Grade I brain relaxation when burst suppression dose of anaesthetics were used [11]. In our study, we used propofol and desflurane, for maintenance of anaesthesia as measured by ENTROPY™, keeping the values of State Entropy between 40 and 60. It is unlikely that burst suppression can be achieved at the above-mentioned values of State Entropy. In spite of the above, it will be safe to assume that even though there is a difference in pharmacodynamics of propofol and desflurane on CBF and ICP but still both the agents are similar in terms of providing identical brain relaxation in “good grade” aneurysmal SAH patients. The effect of two anaesthetics on intraoperative haemodynamics was also similar. Less than 10% of patients in both the groups had haemodynamic variation which required corrective measures.
Another major endeavour of neuroanaesthesia is to have smooth and early awakening. Smooth emergence is vital to prevent the development of hematomas, whereas early awakening facilitates early neurological assessment [19]. However, one major drawback of early emergence is the hypertension which accompanies it and predisposes the patient to development of hematoma [20]. Both propofol and desflurane can facilitate early emergence from anaesthesia. Since our patients were WFNS grade I and II (“good grade”), our plan was to reverse the residual neuromuscular blockade and extubate the trachea after surgery except in those patients who had some intraoperative event or had a “tight” brain at the time of dural closure. 60.6% patients in the propofol group and 74.2% in the desflurane group were extubated in the operation theatre after the end of surgery. Even though the percentage of patients extubated in the propofol group is less than that in the desflurane group, the difference is statistically not significant. Discontinuation of anaesthetics towards the end of surgery leads to stress caused by arousal and this compounded by the presence of an endotracheal tube leads to catecholamine surge which manifests as emergence hypertension [21]. In our study, greater number of patients in the desflurane group had emergence hypertension requiring use of a beta blocker when compared to propofol group, which was significant. The observations are similar to a study in which the use of inhalational agents in neurosurgical patients has greater incidence of emergence hypertension when compared to intravenous agents [19]. In our study, the mean time to eye opening, extubation, and obeying verbal commands after stopping the anaesthetic agent are similar in both the groups. The results are comparable to two trials conducted in supratentorial surgeries which compared emergence and extubation time with the use of an intravenous and an inhalational agent [15, 22].
SjVO2 provides an indirect assessment of cerebral oxygen use and is used to guide management decisions in a variety of clinical paradigms [23]. A constant SjVO2 in the normal range indicates coupling of cerebral blood flow and metabolism. A low SjVO2 indicates either an increase in oxygen extraction due to increase in CMRO2 or a reduction of CBF while a high SjVO2 indicates a decrease in oxygen extraction due to decrease in CMRO2 or an increase in CBF. In our study, data could be obtained only from 13 patients in propofol group and 14 patients in the desflurane group. As evident from our results, the SjVO2 values at all times are within the normal range (55–75%) in the propofol group. The mean values of SjVO2 in the desflurane group during surgery were always higher (74% or more). In a couple of other studies, the CMR reduction has been observed to be 48–58% with propofol, while it is 35–51% with desflurane while using anaesthetic dose of both the agents [8, 24]. Since the maximum reduction of CMR is almost similar with propofol and desflurane, it would be logical to interpret that the increase in SjVO2 values with desflurane could be related to increase in the CBF. The difference in values obtained after craniotomy and after application of clip is statistically higher in the desflurane group when compared to propofol group. The findings are consistent with the fact that the flow metabolism coupling is preserved with propofol, whereas volatile agents like desflurane leads to a state, wherein CMRO2 is reduced, but the CBF does not reduce in proportion to the reduction in CMRO2 [10]. In other studies as well, SjVO2 values generally increased above baseline whenever a volatile agent was used [25, 26]. A study was conducted in the subset of SAH patients in the ICU for sedation, wherein propofol was compared with isoflurane for the effect on regional CBF. An increase in regional CBF was observed for the time when isoflurane was used for sedation which is consistent with our results for desflurane in terms of SjVO2 [27]. Nevertheless, this difference in the SjVO2 values among the groups in our study did not influence any of the clinical parameters like intraoperative brain condition, incidence of postoperative vasospasm or outcome.
We used 100% oxygen to ventilate the lungs of patients in both the groups in our study. This was due to the unavailability of medical air in the neurosurgical operating room complex in which the aneurysm surgeries were undertaken. We did not administer nitrous oxide as it causes increase in CBF, CMRO2, and ICP which are greater in proportion with concomitant use of an inhalation agent than with the use of propofol [28]. This could have confounded the observations of our study. Use of a high fraction of inspired oxygen during surgeries has been suggested to cause a significant reduction in the incidence of surgical site infection and postoperative nausea and vomiting [29,30,31]. At the same time, it has been found to increase the incidence of pulmonary complications like atelectasis and airway inflammation [32, 33]. However, a large randomized trial did not find either a significant reduction in the incidence of surgical site infection or an increase in the frequency of pulmonary complications with the use of high inspiratory oxygen concentration [34]. From the available literature, 100% O2 can be used safely for around 6 h in humans without causing any side effects [35]. Hence, only those patients who underwent surgery for 5 h or less were included in our study.
In addition to the above, our study has a few other limitations. First, our study included only good grade SAH patients, whereas it is poor grade patients who are more likely to have significantly raised ICP. In such patients, the use of these two agents with different actions on cerebral physiology might show up different results and is an area of future research. The measurement of ICP would have been ideal and an objective indication of the effect of anaesthetics. Second, the SjVO2 values were only intermittently measured by jugular venous sampling in limited number of patients. Moreover, the interpretation that there is increased CBF with use of desflurane when compared to propofol is indirect and based on the SjVO2 values.
However, the intraoperative parameters and the neurological outcome at discharge were similar with the use of both the anaesthetic agents. Desflurane when compared to propofol has the potential to cause an increase in cerebral blood flow. The study concludes that in patients with good grade SAH, the post anaesthetic outcome as measured by the duration of postoperative hospital stay is similar with use of either propofol or desflurane.
References
Linn FH, Rinkel GJ, Algra A, van Gijn J. Incidence of subarachnoid haemorrhage: role of region, year and rate of CT: a meta analysis. Stroke. 1996;27:625–9.
Van Gijn J, Rinkel GJ. Subarachnoid hemorrhage: diagnosis, causes and management. Brain. 2001;124:249–78.
Haley EC Jr, Kassell NF, Torner JC. The International Cooperative Study on the timing of aneurysm surgery: the North American experience. Stroke. 1992;23:205–14.
Wartenberg KE, Schmidt JM, Classeen J, Temes RE, Frontera JA, Ostapkovich N, Parra A, Connolly ES, Mayer SA. Impact of medical complications on outcome after subarachnoid haemorrhage. Crit Care Med. 2006;34:617.
Kay B, Rolly G. I.C.I. 35868. The effect of a change of formulation on the incidence of pain after intravenous injection. Acta Anaesthesiol Belg. 1977;28:317–22.
Strebel S, Kaufman M, Guardiola PM, Schaefer HG. Cerebral vasomotor responsiveness is preserved during propofol and midazolam anaesthesia in humans. Anaesth Analg. 1994;78:884–8.
Adembri C, Venturi L, Pellegrini Giampietro DE. Neuroprotective effects of propofol in acute cerebral injury. CNS Drug Rev. 2007;13:333–5.
Mielck F, Stephen H, Buhre W, Weyland A, Sonntag H. Effects of 1 MAC desflurane on cerebral metabolism, cerebral blood flow and carbon dioxide reactivity in humans. BJA. 1998;81:155–60.
Engelhard K, Werner C, Reeker W, Lu H, Mollenberg O. Desflurane and isoflurane improve neurological outcome after incomplete cerebral ischaemia in rats. BJA. 1999;83:415–21.
Matta BF, Mayberg TS, Lam AM. Direct cerebrovasodilatory effects of halothane, isoflurane and desflurane during propofol induced isoelectric electroencephalogram in humans. Anaesthesiology. 1995;83:980–5.
Cheng MA, Ratnaraj J, McHugh TA, Dacey RG Jr, Tempelhoff R. Burst suppression during surgery for cerebral aneurysm: propofol vs. desflurane. Anesthesiology. 2002;96:A25.
Foroohar M, Macdonald RL, Roth S, Stoodley M, Weir B. Intraoperative variables and early outcome after aneurysm surgery. Surg Neurol. 2000;54:304–15.
Todd MM, Warner DS, Sokol MD, Mazen AM, Bradley JH, Franklin LS, Jerry K. A prospective comparative trial of three anaesthetics for elective supratentorial craniotomy: propofol/fentanyl, isoflurane/nitrous oxide, fentanyl/nitrous oxide. Anaesthesiology. 1993;78:1005–20.
Peterson KD, Landsfeldt U, Cold GE, Petersen CB, Mau S, Hauerberg J, Holst P, Olsen KS. Intracranial pressure and cerebral haemodynamics in patients with cerebral tumors: a randomized prospective study of patients subjected to craniotomy in propofol-fentanyl, isoflurane-fentanyl or sevoflurane-fentanyl anaesthesia. Anaesthesiology. 2003;98:329–36.
Bastola P, Bhagat H, Wig J. Comparative trial of propofol, sevoflurane and desflurane as a choice of anaesthesia in patients undergoing elective supratentorial craniotomy. Indian J Anaesth. 2015;59:287–94.
Fiset P, Paus T, Daloze T, Plourde G, Meuret P, Bonhomme V, Hajj-Ali N, Backman SB, Evans AC. Brain mechanism of propofol induced loss of consciousness in humans. A PET study. J Neurosci. 1999;19:5506–13.
Schuttler J, Stoeckel H, Schwilden H. Pharmacokinetic and pharmacodynamics modelling of propofol (Diprivan) in volunteers and surgical patients. Postgrad Med J. 1985;61:53.
Mishra LD. Cerebral blood flow and anaesthesia: a review. Indian J Anaesth. 2002;46:87–95.
Bhagat H, Dash Hari H, Bithal PK, Chouhan RS, Pandia MP. Planning for early emergence in neurosurgical patients: a randomized prospective trial of low dose anaesthetics. Anaesth Analg. 2008;107:1348–55.
Basali A, Mascha EJ, Kalfas I, Schubert A. Relation between perioperative hypertension and intracranial haemorrhage after craniotomy. Anesthesiology. 2000;93:48–54.
Gal TJ, Cooperman LH. Hypertension in the immediate postoperative period. BJA. 1975;47:70–4.
Magni G, Baisi F, La Rosa I. No difference in emergence time and early cognitive function between sevoflurane-fentanyl and propofol-remifentanil in patients undergoing craniotomy for supratentorial intracranial surgery. J Neurosurg Anesthesiol. 2005;17:134–8.
De Deyne C, Van Aken J, Decruyenaere J, Struys M, Colardyn F. Jugular bulb oximetry: review on a cerebral monitoring technique. Acta Anaesthesiol Belg. 1998;49:21–31.
Alkire MT, Haier RJ, Barker SJ, Shah NK, Wu JC, Kao YJ. Cerebral metabolism during propofol anesthesia in humans studied with positron emission tomography. Anesthesiology. 1995;82:393–403.
Jansen GF, van Pragh BH, Kedaria MB, Odoom JA. Jugular bulb saturation during propofol and isoflurane/nitrous oxide anaesthesia in patients undergoing brain tumor surgery. Anaesth Analg. 1999;89:358–63.
Liao Ren, Li Jingyi, Liu Jin. Volatile induction/maintenance of anaesthesia with sevoflurane increases jugular venous oxygen saturation and lumbar cerebrospinal fluid pressure in patients undergoing craniotomy. Eur J Anaesthesiol. 2010;27:369–76.
Villa F, Iacca C, Molinari AF, Gussani C, Aletti C, Pesenti A, Citerio GL. Inhalation versus endovenous sedation in subarachnoid haemorrhage patients. Effects on regional cerebral blood flow. Crit Care Med. 2012;40:2797–804.
Kaisti KK, Langsjo JW, Aalto S, Oikonen V, Sipila H, Teras M, Hinkka S, Metsahonkala L, Scheinin H. Effects of sevoflurane, propofol and adjunct nitrous oxide on regional CBF, oxygen consumption and blood volume in humans. Anaesthesiology. 2003;99:603–13.
Greif R, Akça O, Horn EP, Kurz A, Sessler DI, Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000;342:161–7.
Belda FJ, Aguilera L, García de la Asunción J, Alberti J, Spanish Reduccion de la Tasa de Infeccion Quirurgica Group. Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA. 2005;294:2035–42.
Greif R, Laciny S, Rapf B, Hickle RS, Sessler DI. Supplemental oxygen reduces the incidence of postoperative nausea and vomiting. Anesthesiology. 1999;91:1246–52.
Akca O, Podolsky A, Eisenhuber E, Panzer O, Hetz H, Lampl K, Lackner FX, Wittmann K, Grabenwoeger F, Kurz A, Schultz AM, Negishi C, Sessler DI. Comparable postoperative pulmonary atelectasis in patients given 30% or 80% oxygen during and 2 hours after colon resection. Anesthesiology. 1999;91:991–8.
Carpagnano GE, Kharitonov SA, Foschino-Barbaro MP, Resta O, Gramiccioni E, Barnes PJ. Supplementary oxygen in healthy subjects and those with COPD increases oxidative stress and airway inflammation. Thorax. 2004;59:1016–9.
Meyhoff CS, Wetterslev J, Jorgensen LN, Henneberg SW, Hogdall C, PROXI Trial Group. Effect of high perioperative oxygen fraction on surgical site infection and pulmonary complications after abdominal surgery. The PROXI randomized clinical trial. JAMA. 2009;302:1543–50.
Van de Water J, Kagey KS, Miller IT, Parker DA, O’Connor NE, Sheh J-M, MacArthur JD, Zollinger RM Jr, Moore FD. Response of the lung to six to twelve hours of 100% oxygen inhalation in normal men. N Engl J Med. 1970;283:621–6.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Bhardwaj, A., Bhagat, H., Grover, V.K. et al. Comparison of propofol and desflurane for postanaesthetic morbidity in patients undergoing surgery for aneurysmal SAH: a randomized clinical trial. J Anesth 32, 250–258 (2018). https://doi.org/10.1007/s00540-018-2474-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-018-2474-z