Abstract
Background
Little is known about the specific risks of metastasis in esophageal adenocarcinoma in relation to invasion depth or other pathologic factors.
Methods
We conducted a multicenter retrospective study in 13 high-volume centers in Japan from January 2000 to October 2014 to elucidate the risk of metastasis of esophageal adenocarcinoma. A total of 458 patients (217 surgically resected and 241 endoscopically resected) with esophageal adenocarcinoma or esophagogastric adenocarcinoma involving the esophagus were included. Metastasis was considered positive if there was histologically confirmed metastasis in the surgical specimen or clinically confirmed metastasis during follow-up. Metastasis was considered negative if no metastasis was identified in resected specimens and during follow-up in patients treated surgically or no metastasis during follow-up for >5 years in patients treated by endoscopic resection.
Results
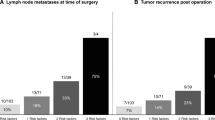
Metastasis was identified in 72 patients. Multivariate analysis confirmed lymphovascular involvement [odds ratio (OR) 6.20; 95 % confidence interval (CI) 3.12–12.32; p < 0.001], a poorly differentiated component (OR 3.69; 95 % CI 1.92–7.10; p < 0.001), and lesion size >30 mm (OR 3.12; 95 % CI 1.63–5.97; p = 0.001) as independent risk factors for metastasis. No metastasis was detected in patients with mucosal cancer without lymphovascular involvement and a poorly differentiated component (0/186 lesions) or in patients with cancer invading the submucosa (1–500 µm) without lymphovascular involvement, a poorly differentiated component, and ≤30 mm (0/32 lesions).
Conclusions
Mucosal and submucosal cancers (1–500 µm invasion) without risk factors have a low incidence of metastasis and may thus be good candidates for endoscopic resection.

Similar content being viewed by others
References
DeMeester SR. Adenocarcinoma of the esophagus and cardia: a review of the disease and its treatment. Ann Surg Oncol. 2006;13:12e30.
Shaheen NJ, Richter JE. Barrett’s oesophagus. Lancet. 2009;373:850–61.
Brown LM, Devesa SS, Chow WH. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J Natl Cancer Inst. 2008;100:1184–7.
Wu JC. Gastroesophageal reflux disease: an Asian perspective. J Gastroenterol Hepatol. 2008;23:1785–93.
Hongo M, Nagasaki Y, Shoji T. Epidemiology of esophageal cancer: orient to occident. Effects of chronology, geography and ethnicity. J Gastroenterol Hepatol. 2009;24:729–35.
Gillison EW, Powell J, Mcconkey CC, et al. Surgical workload and outcome after resection for carcinoma of the oesophagus and cardia. Br J Surg. 2002;89:344–8.
Inadomi JM, Sampliner R, Lagergren J, et al. Screening and surveillance for Barrett esophagus in high-risk groups: a cost-utility analysis. Ann Intern Med. 2003;138:176–86.
Sharma P, Sidorenko EI. Are screening and surveillance for Barrett’s oesophagus really worthwhile? Gut. 2005;54:i27–32.
Abela JE, Going JJ, Mackenzie JF, et al. Systematic four-quadrant biopsy detects Barrett’s dysplasia in more patients than nonsystematic biopsy. Am J Gastroenterol. 2008;103:850–5.
Nakagawa K, Koike T, Iijima K, et al. Comparison of the long-term outcomes of endoscopic resection for superficial squamous cell carcinoma and adenocarcinoma of the esophagus in Japan. Am J Gastroenterol. 2014;109:348–56.
Pech O, May A, Manner H, et al. Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus. Gastroenterology. 2014;146:652–60.
Manner H, Pech O, Heldmann Y, et al. Efficacy, safety, and long-term results of endoscopic treatment for early stage adenocarcinoma of the esophagus with low-risk sm1 invasion. Clin Gastroenterol Hepatol. 2013;11:630–5.
Westerterp M, Koppert LB, Buskens CJ, et al. Outcome of surgical treatment for early adenocarcinoma of the esophagus or gastro-esophageal junction. Virchows Arch. 2005;446:497–504.
Stein HJ, Feith M, Bruecher BL, et al. Early esophageal cancer: pattern of lymphatic spread and prognostic factors for long-term survival after surgical resection. Ann Surg. 2005;242:566–73.
Barbour AP, Jones M, Brown I, et al. Risk stratification for early esophageal adenocarcinoma: analysis of lymphatic spread and prognostic factors. Ann Surg Oncol. 2010;17:2494–502.
Lee L, Ronellenfitsch U, Hofstetter WL, et al. Predicting lymph node metastases in early esophageal adenocarcinoma using a simple scoring system. J Am Coll Surg. 2013;217:191–9.
Altorki NK, Lee PC, Liss Y, et al. Multifocal neoplasia and nodal metastases in T1 esophageal carcinoma: implications for endoscopic treatment. Ann Surg. 2008;247:434–9.
Pennathur A, Farkas A, Krasinskas AM, et al. Esophagectomy for T1 esophageal cancer: outcomes in 100 patients and implications for endoscopic therapy. Ann Thorac Surg. 2009;87:1048–54.
Dubecz A, Kern M, Solymosi N, et al. Predictors of lymph node metastasis in surgically resected T1 esophageal cancer. Ann Thorac Surg. 2015;99:1879–86.
Prasad GA, Wu TT, Wigle DA, et al. Endoscopic and surgical treatment of mucosal (T1a) esophageal adenocarcinoma in Barrett’s esophagus. Gastroenterology. 2009;137:815–23.
Alvarez HL, Pouw RE, van Vilsteren FG, et al. Risk of lymph node metastasis associated with deeper invasion by early adenocarcinoma of the esophagus and cardia: study based on endoscopic resection specimens. Endoscopy. 2010;42:1030–6.
Buskens CJ, Westerterp M, Lagarde SM, et al. Prediction of appropriateness of local endoscopic treatment for high-grade dysplasia and early adenocarcinoma by EUS and histopathologic features. Gastrointest Endosc. 2004;60:703–10.
Sepesi B, Watson TJ, Zhou D, et al. Are endoscopic therapies appropriate for superficial submucosal esophageal adenocarcinoma? An analysis of esophagectomy specimens. J Am Coll Surg. 2010;210:418–27.
Leers JM, DeMeester SR, Oezcelik A, et al. The prevalence of lymph node metastases in patients with T1 esophageal adenocarcinoma a retrospective review of esophagectomy specimens. Ann Surg. 2011;253:271–8.
Dunbar KB, Spechler SJ. The risk of lymph-node metastases in patients with high-grade dysplasia or intramucosal carcinoma in Barrett’s esophagus: a systematic review. Am J Gastroenterol. 2012;107:850–62.
Japan Esophageal Society. Japanese Classification of Esophageal Cancer, tenth edition: part I. Esophagus. 2009;6:1–58.
Metz CE. Basic principles of ROC analysis. Semin Nucl Med. 1978;8:283–98.
Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–25.
Morson BC, Whiteway JE, Jones EA, et al. Histopathology and prognosis of malignant colorectal polyps treated by endoscopic polypectomy. Gut. 1984;25:437–44.
Goseki N, Koike M, Yoshida M. Histopathologic characteristics of early stage esophageal carcinoma. A comparative study with gastric carcinoma. Cancer. 1992;69:1088–93.
Bogomoletz WV, Molas G, Gayet B, et al. Superficial squamous cell carcinoma of the esophagus. A report of 76 cases and review of the literature. Am J Surg Pathol. 1989;13:535–46.
Sugimachi K, Ikebe M, Kitamura K, et al. Long-term results of esophagectomy for early esophageal carcinoma. Hepatogastroenterology. 1993;40:203–6.
Sabik JF, Rice TW, Goldblum JR, et al. Superficial esophageal carcinoma. Ann Thorac Surg. 1995;60:896–902.
Davison JM, Landau MS, Luketich JD, et al. A model based on pathologic features of superficial esophageal adenocarcinoma complements clinical node staging in determining risk of metastasis to lymph nodes. Clin Gastroenterol Hepatol. 2016;14:369–77.
Griffin SM, Burt AD, Jennings NA. Lymph node metastasis in early esophageal adenocarcinoma. Ann Surg. 2011;254:731–6.
Bollschweiler E, Baldus SE, Schroder W, et al. High rate of lymph-node metastasis in submucosal esophageal squamous cell carcinomas and adenocarcinomas. Endoscopy. 2006;38:149–56.
Manner H, Pech O, Heldmann Y, et al. The frequency of lymph node metastasis in early-stage adenocarcinoma of the esophagus with incipient submucosal invasion (pT1b sm1) depending on histological risk patterns. Surg Endosc. 2015;29:1888–96.
Greene CL, Worrell SG, Attwood SE, et al. Emerging concepts for the endoscopic management of superficial esophageal adenocarcinoma. J Gastrointest Surg. 2016;20:851–60.
Mohiuddin K, Dorer R, El Lakis MA, et al. Outcomes of surgical resection of T1bN0 esophageal cancer and assessment of endoscopic mucosal resection for identifying low-risk cancers appropriate for endoscopic therapy. Ann Surg Oncol. 2016;23:2673–8.
Dresner SM, Griffin SM. Pattern of recurrence following radical oesophagectomy with two-field lymphadenectomy. Br J Surg. 2000;87:1426–33.
Sgourakis G, Gockel I, Lang H. Endoscopic and surgical resection of T1a/T1b esophageal neoplasms: a systematic review. World J Gastroenterol. 2013;19:1424–37.
Schlemper RJ, Itabashi M, Kato Y, et al. Differences in diagnostic criteria for gastric carcinoma between Japanese and Western pathologists. Lancet. 1997;349:1725–9.
Stolte M, Kirtil T, Oellig F, et al. The pattern of invasion of early carcinomas in Barrett’s esophagus is dependent on the depth of infiltration. Pathol Res Pract. 2010;206:300–4.
Acknowledgments
We thank Tomoki Shimizu, Yasutaka Kuribayashi, Yuko Hara, Hiroki Kikuchi, Yuichi Sato, Mitsuhiro Fujishiro, and Taku Yamagata for help with data collection, Yasuo Ohkura, Tomio Arai and Atsusi Ochiai for help with pathologic examination, and Junya Oguma, Takayuki Nishi for general advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Saku Central Hospital Ethics Committee.
Funding
Supported by a grant from the Japanese Gastroenterological Association.
Rights and permissions
About this article
Cite this article
Ishihara, R., Oyama, T., Abe, S. et al. Risk of metastasis in adenocarcinoma of the esophagus: a multicenter retrospective study in a Japanese population. J Gastroenterol 52, 800–808 (2017). https://doi.org/10.1007/s00535-016-1275-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1275-0