Abstract
Background/Purpose
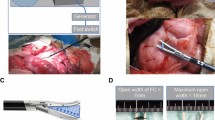
The VIO soft-coagulation system (SC) is a new device for tissue coagulation. We hypothesized that this device would be an effective tool for sealing small pancreatic ducts, thus reducing pancreatic fistula following pancreatectomy.
Methods
To confirm whether the SC could be used to seal small pancreatic ducts, we measured the burst pressure in sealed ducts in mongrel dogs. Eight dogs underwent distal pancreatectomy, with the remnant stump coagulated by using the SC. The animals were necropsied on postoperative day 10. In a clinical trial, 11 patients who underwent pancreatoduodenectomy with SC treatment (SC group), and 24 patients who underwent pancreatoduodenectomy without SC treatment (non-SC group) were compared.
Results
In the experimental study, the burst-pressure test revealed that the SC had efficiently sealed the small pancreatic ducts. Histological examination revealed completely obstructed pancreatic ductal structures, ranging from large pancreatic ducts (diameter, 500 μm) to microscopic ducts. No pancreatic leakage was observed following distal pancreatectomy without main pancreatic duct (MPD) suturing in dogs that had an MPD diameter of less than 500 μm. In the clinical trial, pancreatic fistula developed in only one patient (9.1%) in the SC group, but a pancreatic fistula developed in five patients (20.8%) in the non-SC group.
Conclusions
This novel technique using the SC is an effective procedure for preventing the development of pancreatic fistula following pancreatectomy.
Similar content being viewed by others
References
Balcom JH 4th, Rattner DW, Warshaw AL, Chang Y, Fernandezdel, Castillo C. Ten years’ experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg 2000;136:391–398.
Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, Yeo CJ. Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg 1999;229:693–698.
Knaebel HP, Diener MK, Wente MN, Buchler MW, Seiler CM. Systematic review and meta-analysis of technique for closure of the pancreatic remnant after distal pancreatectomy. Br J Surg 2005;92:539–546.
Bilimoria MM, Cormier JN, Mun Y, Lee JE, Evans DB, Pisters PWT. Pancreatic leak after left pancreatectomy is reduced following MPD ligation. Br J Surg 2003;90:190–196.
Sugo H, Mikami Y, Matsumoto F, Tsumura H, Watanabe Y, Futagawa S. Comparison of ultrasonically activated scalpel versus conventional division for the pancreas in distal pancreatectomy. J Hepatobiliary Pancreat Surg 2001;8:349–352.
Landman J, Kerbl K, Rehman J, Andreoni C, Humphrey PA, Collyer W, et al. Evaluation of a vessel sealing system, bipolar electrosurgery, harmonic scalpel, titanium clips, endoscopic gastrointestinal anastomosis, vascular staples and sutures for arterial and venous ligation in a porcine model. J Urol 2003;169:697–700.
Kuroda Y, Tanioka Y, Suzuki Y, Ku Y, Saitoh Y. Distal pancreatectomy using the ultrasonic dissector. J Am Coll Surg 1995;180:737–738.
Truty MJ, Sawyer MD, Que FG. Decreasing pancreatic leak after distal pancreatectomy: saline-coupled radiofrequency ablation in a porcine model. J Gastrointest Surg 2007;11:998–1007.
Pachter HL, Pennington R, Chassin J, Spencer FC. Simplified distal pancreatectomy with the auto suture stapler: preliminary clinical observations. Surgery 1979;85:166–170.
Suzuki Y, Fujino Y, Tanioka Y, Hori Y, Ueda T, Takeyama Y, et al. Randomized clinical trial of ultrasonic dissector or conventional division in distal pancreatectomy for non-fibrotic pancreas. Br J Surg 1999;86:608–611.
Author information
Authors and Affiliations
About this article
Cite this article
Nagakawa, Y., Tsuchida, A., Saito, H. et al. The VIO soft-coagulation system can prevent pancreatic fistula following pancreatectomy. J Hepatobiliary Pancreat Surg 15, 359–365 (2008). https://doi.org/10.1007/s00534-008-1329-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-008-1329-7