Abstract
Purpose
Management of female sexual dysfunction (FSD) is vital for women with breast cancer due to the devastating consequences, which include marital disharmony and reduced quality of life. We explore healthcare providers’ (HCPs) perceptions and experiences in managing FSD for women living with breast cancer using a phenomenological approach.
Methods
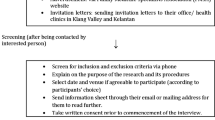
This qualitative study was conducted using a face-to-face interview method with HCPs from two tertiary hospitals in North East Malaysia. The interviews were recorded, transcribed verbatim, and transferred to NVivo ® for data management. The transcriptions were analyzed using thematic analysis.
Results
Three key barriers were identified through the thematic analysis: a scarcity of related knowledge; the influence of socio-cultural ideas about sex; and the specialty-centric nature of the healthcare system. Most HCPs interviewed had a very narrow understanding of sexuality, were unfamiliar with the meaning of FSD, and felt their training on sexual health issues to be very limited. They viewed talking about sex to be embarrassing to both parties that are both to HCPs and patients and was therefore not a priority. They focused more on their specialty hence limited the time to discuss sexual health and FSD with their patients.
Conclusion
Therefore, interventions to empower the knowledge, break the socio-cultural barriers, and improve the clinic settings are crucial for HCPs in managing FSD confidently.

adapted from Hayden (2019))


Similar content being viewed by others
Availability of data and material
Data are kept at the Family Medicine Department, School of Medical Sciences, Universiti Sains Malaysia, 16,150 Kubang Kerian, Kelantan, Malaysia. Data will be shared upon request and it is subjected to the data protection regulations.
Code availability
Not applicable.
References
Del Pup L, Villa P, Amar ID, Bottoni C, Scambia G (2019) Approach to sexual dysfunction in women with cancer. Int J Gynecol Cancer ijgc-2018–000096. https://doi.org/10.1136/ijgc-2018-000096
Webber K, Mok K, Bennett B, Lloyd AR, Friedlander M, Juraskova I et al (2011) If I am in the mood, I enjoy it: an exploration of cancer-related fatigue and sexual functioning in women with breast cancer. Oncologist 16(9):1333–1344. https://doi.org/10.1634/theoncologist.2011-0100
Norley S (2014) Sexual dysfunction, body image distress and marital dissatisfaction in breast cancer patients of University Malaya Medical Centre (UMMC): University of Malaya
Ishak WW, Tobia G (2013) DSM-5 changes in diagnostic criteria of sexual dysfunctions. Reprod Syst Sex Disord 2:122. https://doi.org/10.4172/2161-038X.1000122
Boswell EN, Dizon DS (2015) Breast cancer and sexual function. Transl Androl Urol 4(2):160–168. https://doi.org/10.3978/j.issn.2223-4683.2014.12.04
Sbitti Y, Kadiri H, Essaidi I, Fadoukhair Z, Kharmoun S, Slimani K et al (2011) Breast cancer treatment and sexual dysfunction: Moroccan women’s perception. BMC Women’s Health 11:29. https://doi.org/10.1186/1472-6874-11-29
Park EL, Norris R, Bober S (2009) Sexual health communication during cancer care: barriers and recommendations. 74–7. https://doi.org/10.1097/PPO.0b013e31819587dc
Dyer K, das Nair R (2013) Why don’t healthcare professionals talk about sex A systematic review of recent qualitative studies conducted in the United Kingdom. J Sex Med 10(11):2658–70. https://doi.org/10.1111/j.1743-6109.2012.02856.x
Canzona MR, Ledford CJW, Fisher CL, Garcia D, Raleigh M, Kalish VB (2018) Clinician barriers to initiating sexual health conversations with breast cancer survivors: the influence of assumptions and situational constraints. Fam Syst Health 36(1):20–28. https://doi.org/10.1037/fsh0000307
Rosenstock IM (1974) Historical origins of the Health Belief Model. Health Educ Monogr 2(4):328–335
Shabibi P, Zavareh MSA, Sayehmiri K, Qorbani M, Safari O, Rastegarimehr B, et al. Effect of educational intervention based on the Health Belief Model on promoting self-care behaviors of type-2 diabetes patients. Electron Phys. 2017;9(12):5960–8. https://doi.org/10.19082/5960
Brinsley KJ, Sinkowitz-Cochran RL, Cardo DM (2005) Assessing motivation for physicians to prevent antimicrobial resistance in hospitalized children using the Health Belief Model as a framework. Am J Infect Control 33(3):175–181. https://doi.org/10.1016/j.ajic.2004.12.004
Rosenstock IM, Strecher VJ, Becker MH (1988) Social learning theory and the Health Belief Model. Health Educ Q 15(2):175–183
Bandura A (1997) Self-efficacy: the exercise of control. Freeman, New York
Orji R, Vassileva J, Mandryk R (2012) Towards an effective health interventions design: an extension of the health belief model. Online J Public Health Inform. 4(3):ojphi.v4i3.4321. https://doi.org/10.5210/ojphi.v4i3.4321
Khan S (2014) Qualitative research method - Phenomenology. 298–310 p
Rasmussen DM, Hansen HP, Elverdam B (2010) How cancer survivors experience their changed body encountering others. Eur J Oncol Nurs 14(2):154–159. https://doi.org/10.1016/j.ejon.2009.10.001
Hammarberg K, Kirkman M, de Lacey S (2016) Qualitative research methods: when to use them and how to judge them. Hum Reprod 31(3):498–501. https://doi.org/10.1093/humrep/dev334
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B et al (2018) Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 52(4):1893–1907. https://doi.org/10.1007/s11135-017-0574-8
Green J, Thorogood N (2018) Qualitative methods for health research. Sage
Liamputtong P (2020) Qualitative research methods, 5th edn. Oxford University Press, Melbourne
Muhamad R, Horey D, Liamputtong P, Low WY (2019) Managing women with sexual dysfunction: difficulties experienced by Malaysian family physicians. Arch Sex Behav 48(3):949–960. https://doi.org/10.1007/s10508-018-1236-1
Kingsberg SA, Schaffir J, Faught BM, Pinkerton JV, Parish SJ, Iglesia CB et al (2019) Female sexual health: barriers to optimal outcomes and a roadmap for improved patient-clinician communications. J Women’s Health 28(4):432–443. https://doi.org/10.1089/jwh.2018.7352
Lai P, Yee Tan S, Liew S (2016). Views and experiences of Malaysian family medicine trainees of female sexual dysfunction. https://doi.org/10.1007/s10508-016-0796-1
Ariffin F (2013) Sexual history taking: assessing Malaysian medical student knowledge in sexual health
Perz J, Ussher JM, Gilbert E (2013) Constructions of sex and intimacy after cancer: a methodology study of people with cancer, their partners, and health professionals. BMC Cancer 13(1):270. https://doi.org/10.1186/1471-2407-13-270
Hinchliff S, Gott M (2011) Seeking medical help for sexual concerns in mid and later life: a review of the literature. J Sex Res 48(2–3):106–117. https://doi.org/10.1080/00224499.2010.548610
Lieber E, Chin D, Li L, Rotheram-Borus MJ, Detels R, Wu Z et al (2009) Sociocultural contexts and communication about sex in China: informing HIV/STD prevention programs. AIDS Educ Prev 21(5):415–429. https://doi.org/10.1521/aeap.2009.21.5.415
Parish SJ, Hahn SR, Goldstein SW, Giraldi A, Kingsberg SA, Larkin L et al (2019) The international society for the study of women’s sexual health process of care for the identification of sexual concerns and problems in women. Mayo Clin Proc 94(5):842–856. https://doi.org/10.1016/j.mayocp.2017.11.002
Gott M, Hinchliff S (2003) Barriers to seeking treatment for sexual problems in primary care: a qualitative study with older people. Fam Pract 20(6):690–695. https://doi.org/10.1093/fampra/cmg612
Tudor KI, Eames S, Haslam C, Panicker J (2015) Barriers in clinic to discussing sexual dysfunction due to multiple sclerosis. J Neurol Neurosurg Psychiatry 86(11):e4. https://doi.org/10.1136/jnnp-2015-312379.6
Bdair I, Constantino R (2017) Barriers and promoting strategies to sexual health assessment for patients with coronary artery diseases in nursing practice: a literature review. 473–92. https://doi.org/10.4236/health.2017.93034
Wylie K (2007) Assessment & management of sexual problems in women. J R Soc Med 100(12):547–550. https://doi.org/10.1258/jrsm.100.12.547
Sidi H, Puteh SE, Abdullah N, Midin M (2007) The prevalence of sexual dysfunction and potential risk factors that may impair sexual function in Malaysian women. J Sex Med 4(2):311–321. https://doi.org/10.1111/j.1743-6109.2006.00319.x
Mohdamin H. Budaya Melayu dan Ancaman. Majalah Dewan Budaya. 2013
Mahmoud ZM, Fawaz MA (2015) Nurse’s perception of barriers toward discussing female sexual issues in nursing practice. Med J Cairo Univ 83(2):221–230
Abdulrasulnia M, Shewchuk RM, Roepke N, Granstaff US, Dean J, Foster JA et al (2010) Perceived barrier, practice patterns, and confidence among primary care physicians and gynecologists. J Sex Med 7:2499–2508. https://doi.org/10.1111/j.1743-6109.2010.01857.x
Gott M, Galena E, Hinchliff S, Elford H (2004) “Opening a can of worms”: GP and practice nurse barriers to talking about sexual health in primary care. Fam Pract 21:528–536. https://doi.org/10.1093/fampra/cmh509
Humphery S, Nazareth I (2001) GPs view on their management of sexual dysfunction. Fam Pract 18(5):516–518. https://doi.org/10.1093/fampra/18.5.516
Burd ID, Nevadunsky N, Bachmann G (2006) Original research—education: impact of physician gender on sexual history taking in a multispecialty practice. J Sex Med 3(2):194–200. https://doi.org/10.1111/j.1743-6109.2005.00168.x
Stokes T, Mears J (2000) Sexual health and the practice nurse: a survey of reported practice and attitudes. Br J Fam Plann 26(2):89–92. https://doi.org/10.1783/147118900101194328
Burd ID, Nevadunsky N, Bachmann G (2006) Impact of physician gender on sexual history taking in a multispecialty practice. J Sex Med 3(2):194–200. https://doi.org/10.1111/j.1743-6109.2005.00168.x
Solursh DS, Ernst JL, Lewis RW, Prisant LM, Mills TM, Solursh LP et al (2003) The human sexuality education of physicians in North American medical schools. Int J Impot Res 15(Suppl 5):S41–S45. https://doi.org/10.1038/sj.ijir.3901071
Hughes AK, Rostant OS, Curran PG (2013) Improving sexual health communication between older women and their providers: how the Integrative Model of Behavioral Prediction can help. Res Aging 36(4):450–466. https://doi.org/10.1177/0164027513500055
Acknowledgements
We would like to thank all HCPs that participated in this study
Funding
This study was funded by Universiti Sains Malaysia with Research University Grants (1001/PPSP/8012284) and Graduate Development Study Incentive Fund (TIPPS).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Siti Balqis Chanmekun, Maryam Mohd Zulkifli, Norhasmah Mohd Zin, Rosediani Muhamad, Low Wah Yun, and Pranee Liamputtong. The first draft of the manuscript was written by Siti Balqis Chanmekun and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study protocol and the questionnaires used in this study were reviewed and approved by the ethical approval of Universiti Sains Malaysia (USM/JEPeM/17090387) and Ministry of Health of Malaysia. (NMRR-18–373-39791(IIR)).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chanmekun, S.B., Zulkifli, M.M., Muhamad, R. et al. Managing sexual dysfunction for women with breast cancer: the perspective of healthcare providers in North East Malaysia. Support Care Cancer 30, 401–411 (2022). https://doi.org/10.1007/s00520-021-06417-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06417-0