Abstract
Purpose
Survivors of breast cancer (BC) on the non-dominant side have more persistent deficits than those with cancer on the dominant limb. What is not known is whether those with BC use their involved upper limbs more, less, or at the same level as women without BC. Accelerometer use offers a quantifiable method to measure activity levels of upper limbs. The purpose of this study was to quantify the activity levels of the non-dominant involved limb among survivors of BC and compare these values to their dominant limb, as well as the non-dominant limb of a control group.
Methods
Participants (n = 30) were women with unilateral BC on the non-dominant limb, diagnosed between 6 and 24 months prior to data collection, and a matched healthy group of women as controls. Participants completed the following questionnaires: medical and demographics, Brief Fatigue Inventory, Brief Pain Inventory – Short form, Disabilities of the Arm, Shoulder and Hand (DASH), and Beck Depression Index. Participants wore an accelerometer on each wrist during waking hours for 7 days. Arm activity was measured using vector magnitude activity counts extracted from the accelerometers.
Results
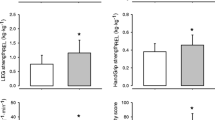
There were no significant differences in total vector magnitude activity counts between groups for either limb. Within group dominant to non-dominant comparison was significantly different (p ≤ 0.001). No significant difference in pain was present but significant differences for fatigue (p = 0.002), depression (p = 0.004), and DASH scores (p = 0.035) were present.
Conclusions
Women with non-dominant BC use their involved limb similar to healthy controls but less than their dominant limb.
Similar content being viewed by others
References
Howlader N, Noone AM, Krapcho M, et al (eds) (2020) SEER Cancer Statistics Review, 1975-2016, National Cancer Institute. Bethesda, https://seer.cancer.gov/csr/1975_2016/, based on November 2018 SEER data submission, posted to the SEER web site, April 2019. Accessed Oct 2019
National Coalition for Cancer Survivorship (NCCS) Our Mission. NCCS - National Coalition for Cancer Survivorship. https://www.canceradvocacy.org/about-us/our-mission/. Accessed January 9, 2020
Ganz PA (2011) The ‘three Ps’ of cancer survivorship care. BMC Med 9:14. https://doi.org/10.1186/1741-7015-9-14
Kootstra J, Hoekstra-Weebers JEHM, Rietman H, de Vries J, Baas P, Geertzen JH, Hoekstra HJ (2008) Quality of life after sentinel lymph node biopsy or axillary lymph node dissection in stage I/II breast cancer patients: a prospective longitudinal study. Ann Surg Oncol 15(9):2533–2541
Mutrie N, Campbell AM, Whyte F, McConnachie A, Emslie C, Lee L, Kearney N, Walker A, Ritchie D (2007) Benefits of supervised group exercise programme for women being treated for early stage breast cancer: pragmatic randomised controlled trial. BMJ. 334(7592):517–517
Blomqvist L, Stark B, Engler N, Malm M (2004) Evaluation of arm and shoulder mobility and strength after modified radical mastectomy and radiotherapy. Acta Oncol 43(3):280–283
Rietman JS, Dijkstra PU, Geertzen JHB, Baas P, de Vries J, Dolsma W, Groothoff JW, Eisma WH, Hoekstra HJ (2003) Short-term morbidity of the upper limb after sentinel lymph node biopsy or axillary lymph node dissection for stage I or II breast carcinoma. Cancer. 98(4):690–696
Hayes S, Battistutta D, Newman B (2005) Objective and subjective upper body function six months following diagnosis of breast cancer. Breast Cancer Res Treat 94(1):1–10
Tengrup I, Tennvall-Nittby L, Christiansson I, Laurin M (2000) Arm morbidity after breast-conserving therapy for breast cancer. Acta Oncol 39(3):393–397
Merchant CR, Chapman T, Kilbreath SL, Refshauge KM, Krupa K (2008) Decreased muscle strength following management of breast cancer. Disabil Rehabil 30(15):1098–1105
Schmitz KH, Speck RM, Rye SA, DiSipio T, Hayes SC (2012) Prevalence of breast cancer treatment sequelae over 6 years of follow-up: the Pulling Through Study. Cancer. 118(8 Suppl):2217–2225
Hayes SC, Johansson K, Stout NL, Prosnitz R, Armer JM, Gabram S, Schmitz KH (2012) Upper-body morbidity after breast cancer: incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer. 118(8 Suppl):2237–2249
Peintinger F, Reitsamer R, Stranzl H, Ralph G (2003) Comparison of quality of life and arm complaints after axillary lymph node dissection vs sentinel lymph node biopsy in breast cancer patients. Br J Cancer 89(4):648–652
Nesvold I, Dahl AA, Lokkevik E, Mengshoel AM, Fossa SD (2008) Arm and shoulder morbidity in breast cancer patients after breast-conserving therapy versus mastectomy. Acta Oncol 47(5):835–842
Rietman JS, Geertzen JH, Hoekstra HJ et al (2006) Long term treatment related upper limb morbidity and quality of life after sentinel lymph node biopsy for stage I or II breast cancer. Eur J Surg Oncol 32(2):148–152
Nesvold I, Foss SD, Holm I, Naume B, Dahl AA (2010) Arm/shoulder problems in breast cancer survivors are associated with reduced health and poorer physical quality of life. Acta Oncol 49(3):347–353
Rietman JS, Dijkstra PU, Debreczeni R, Geertzen JH, Robinson DP, De Vries J (2004) Impairments, disabilities and health related quality of life after treatment for breast cancer: a follow-up study 2.7 years after surgery. Disabil Rehabil 26(2):78–84
Shamley D, Srinaganathan R, Oskrochi R, Lascurain-Aguirrebeña I, Sugden E (2009) Three-dimensional scapulothoracic motion following treatment for breast cancer. Breast Cancer Res Treat 118:315–322. https://doi.org/10.1007/s10549-008-0240-x
Shamley D, Lascurain-Aguirrebena I, Oskrochi R, Srinaganathan R (2012) Shoulder morbidity after treatment for breast cancer is bilateral and greater after mastectomy. Acta Oncol 51(8):1045–1053
Fisher MI, Capilouto G, Malone T, Bush H, Uhl TL (2019) An observational study comparing upper extremity function in women with and without a history of breast cancer. Phys Ther. https://doi.org/10.1093/ptj/pzaa015
Acuna M, Karduna AR (2012) Wrist activity monitor counts are correlated with dynamic but not static assessments of arm elevation exposure made with a triaxial accelerometer. Ergonomics. 55(8):963–970
Lawinger E, Uhl TL, Abel M, Kamineni S (2015) Assessment of accelerometers for measuring upper-extremity physical activity. J Sport Rehabil 24(3):236–243
Hurd WJ, Morrow MM, Kaufman KR (2013) Tri-axial accelerometer analysis techniques for evaluating functional use of the extremities. J Electromyogr Kinesiol 23(4):924–929
Tokuda K, Lee B, Kurihara J et al (2013) Analysis of laterality in upper limb function during simulated range of motion limitation using long-term portable accelerometer recordings. Rigakuryoho Kagaku 28(1):15–20
Stout NL, Pfalzer LA, Springer B, Levy E, McGarvey C, Danoff JV, Gerber LH, Soballe PW (2012) Breast cancer-related lymphedema: comparing direct costs of a prospective surveillance model and a traditional model of care. Phys Ther 92(1):152–163
United States Department of Labor. United States Employment Service, and the North Carolina Occupational Analysis Field Center. Dictionary of Occupational Titles (DOT): Revised Fourth Edition, 1991. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2006-01-12. https://doi.org/10.3886/ICPSR06100.v1
Cella D, Viswanathan HN, Hays RD, Mendoza TR, Stein KD, Pasta DJ, Foreman AJ, Vadhan-Raj S, Kallich JD (2008) Development of a fatigue and functional impact scale in anemic cancer patients receiving chemotherapy. Cancer. 113(6):1480–1488
Farnen Price W, Doherty D, Adams A, Bohde E (2014) Breast Cancer EDGE Task Force Outcomes: evidence-based cancer-related fatigue measurement tools. Rehabil Oncol 32(3):32–39 38p
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the brief pain inventory. Ann Acad Med Singap 23(2):129–138
Harrington S, Gilchrist L, Sander A (2014) Breast Cancer EDGE Task Force Outcomes: clinical measures of pain. Rehabil Oncol. 32(1):13–21
Beck AT, Steer RA, Carbin MG (1988) Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 8(1):77–100
Solway S, Beaton D, McConnell S, Bombardier C (2002) The DASH outcome user’s manual, 2nd edn. Toronto, Institute for Work and Health
Miale S, Harrington S, Kendig T (2013) Oncology section task force on breast cancer outcomes: clinical measures of upper extremity function. Rehabil Oncol 31(1):27–34
de Jong N, Candel MJ, Schouten HC, Abu-Saad HH, Courtens AM (2004) Prevalence and course of fatigue in breast cancer patients receiving adjuvant chemotherapy. Ann Oncol 15(6):896–905
Lis CG, Gupta D, Grutsch JF (2008) The relationship between insomnia and patient satisfaction with quality of life in cancer. Support Care Cancer 16(3):261–266
Schultz SL, Dalton SO, Christensen J, Carlsen K, Ross L, Johansen C (2011) Factors correlated with fatigue in breast cancer survivors undergoing a rehabilitation course, Denmark, 2002-2005. Psychooncology. 20(4):352–360
Gerber LH, Stout N, McGarvey C, Soballe P, Shieh CY, Diao G, Springer BA, Pfalzer LA (2011) Factors predicting clinically significant fatigue in women following treatment for primary breast cancer. Support Care Cancer 19(10):1581–1591
Acknowledgements
This study was funded in part by a grant from the Academy of Oncologic Physical Therapy of the American Physical Therapy Association.
Funding
This study was funded by grant from the Academy of Oncologic Physical Therapy of the American Physical Therapy Association for the purchase of the equipment used in this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Mary Insana Fisher, Claire C Davies, and Timothy L Uhl. The first draft of the manuscript was written by Mary Insana Fisher, Claire C Davies, and Timothy L Uhl, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Mary I Fisher, PT, PhD received a research grant for equipment from the Academy of Oncologic Physical Therapy of the American Physical Therapy Association. Claire Davies, PT, PhD, and Timothy Uhl, PhD, ATC, PT, declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fisher, M.I., Davies, C.C. & Uhl, T.L. A quantitative comparison of arm activity between survivors of breast cancer and healthy controls: use of accelerometry. Support Care Cancer 28, 5307–5313 (2020). https://doi.org/10.1007/s00520-020-05365-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05365-5