Abstract
Background
Taxane acute pain syndrome (TAPS) is a clinically significant side-effect of taxane chemotherapy, often described as arthralgia and myalgia that occurs 2–3 days after infusion. The aim of this study was to assess pain descriptors used by patients during their experience of TAPS.
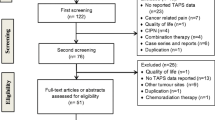
Methods
A clinical prospective cohort study was conducted on breast cancer patients who had not received prior chemotherapy and were asked to complete diaries on three consecutive docetaxel treatment cycles on days 1–7, 14, and 21 (acute phase). Questionnaires to assess pain severity, descriptors of pain, and the interference in activities due to pain were adapted from the Brief Pain Inventory and the McGill Pain Questionnaire. Telephone questionnaire follow-up was done at 1, 3, 6, 9, and 12 months following docetaxel (delayed phase).
Results
The most commonly used descriptor for acute and chronic pain was “aching” (90–96%). However, in the delayed phase of the study, “burning” (32–50%), “radiating” (39–48%), and “sharp” (40–69%) were used more often. In both acute and chronic pain phases, most patients experienced moderate/severe pain regardless of the location. Pain in cycle 1 was predictive of pain in subsequent taxane cycles (p < 0.0001). Pain in cycle 3 was predictive of chronic pain (p < 0.002).
Conclusions
The descriptors used by patients experiencing chemotherapy-induced pain (ChIP) may be reflective of the underlying mechanisms. It is suspected that TAPS initiates as an acute inflammatory pain, which over time develops into neuropathic pain, known as chemotherapy-induced peripheral neuropathy (CIPN). However, the subjective pain experience varies from patient to patient.


Similar content being viewed by others
References
Fernandes R, Mazzarello S, Hutton B, Shorr R, Majeed H, Ibrahim MFK, Jacobs C, Ong M, Clemons M (2016) Taxane acute pain syndrome (TAPS) in patients receiving taxane-based chemotherapy for breast cancer—a systematic review. Support Care Cancer 24(8):3633–3650. https://doi.org/10.1007/s00520-016-3256-5
Addington J, Freimer M (2016) Chemotherapy-induced peripheral neuropathy: an update on the current understanding. F1000Research 5:1466. https://doi.org/10.12688/f1000research.8053.1
Shinde SS, Seisler D, Soori G, Atherton PJ, Pachman DR, Lafky J, Ruddy KJ, Loprinzi CL (2016) Can pregabalin prevent paclitaxel-associated neuropathy - an ACCRU pilot trial. Support Care Cancer 24(2):547–553. https://doi.org/10.1007/s00520-015-2807-5
Chiu N, Zhang L, Dent R, Giotis A, van Draanen J, Gallo-Hershberg D, Chiu L, Chow R, Wan BA, Pasetka M, Stinson J, Stacey E, Verma S, Lam H, Chow E, DeAngelis C (2018) A prospective study of docetaxel-associated pain syndrome. Support Care Cancer 26(1):203–211. https://doi.org/10.1007/s00520-017-3836-z
Fernandes R, Mazzarello S, Hutton B, Shorr R, Ibrahim MFK, Jacobs C et al (2016) A systematic review of the incidence and risk factors for taxane acute pain syndrome in patients receiving taxane-based chemotherapy for prostate cancer. Clin Genitourin Cancer 15(1):1–6. https://doi.org/10.1016/j.clgc.2016.07.018
Chiu N, Chiu L, Chow R, Lam H, Verma S, Pasetka M, Chow E, DeAngelis C (2017) Taxane-induced arthralgia and myalgia: a literature review. J Oncol Pharm Pract 23(1):56–67. https://doi.org/10.1177/1078155215627502
Song SJ, Min J, Suh SY, Jung SH, Hahn HJ, Im SA, Lee JY (2017) Incidence of taxane-induced peripheral neuropathy receiving treatment and prescription patterns in patients with breast cancer. Support Care Cancer 25(7):2241–2248. https://doi.org/10.1007/s00520-017-3631-x
Hellerstedt-Börjesson S, Nordin K, Fjällskog M-L, Holmström IK, Arving C (2015) Women with breast cancer experience of chemotherapy-induced pain: triangulation of methods. Cancer Nurs 38(1):31–39. https://doi.org/10.1097/NCC.0000000000000124
Davis LL, Carpenter JS, Otte JL (2016) State of the science: taxane-induced musculoskeletal pain. Cancer Nurs 39(3):187–196. https://doi.org/10.1097/NCC.0000000000000273
Persohn E, Canta A, Schoepfer S, Traebert M, Mueller L, Gilardini A, Galbiati S, Nicolini G, Scuteri A, Lanzani F, Giussani G, Cavaletti G (2005) Morphological and morphometric analysis of paclitaxel and docetaxel-induced peripheral neuropathy in rats. Eur J Cancer 41(10):1460–1466. https://doi.org/10.1016/j.ejca.2005.04.006
Lambertini M, Del Mastro L, Bellodi A, Pronzato P (2014) The five “Ws” for bone pain due to the administration of granulocyte-colony stimulating factors (G-CSFs). Crit Rev Oncol Hematol 89(1):112–128. https://doi.org/10.1016/j.critrevonc.2013.08.006
Melzac R (1975) The McGill pain questionnaire: major properties and scoring methods. Pain 1(3):277–299
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the brief pain inventory. Ann Acad Med Singap 23(2):129–138
Cleeland C (2009) The Brief Pain Inventory (BPI). In: The brief pain inventory user guide. The Brief Pain Inventory. https://doi.org/10.1016/j.jphys.2015.07.001
Stüve O, Zettl U (2014) Neuroinflammation of the central and peripheral nervous system: an update. Clin Exp Immunol 175(3):333–335. https://doi.org/10.1111/cei.12260
Loprinzi CL, Maddocks-Christianson K, Wolf SL, Rao RD, Dyck PJB, Mantyh P, Dyck PJ (2007) The paclitaxel acute pain syndrome: sensitization of nociceptors as the putative mechanism. Cancer J 13(6):399–403. https://doi.org/10.1097/PPO.0b013e31815a999b
Thakral M, Shi L, Foust JB, Patel KV, Shmerling RH, Bean JF, Leveille SG (2016) Pain quality descriptors in community-dwelling older adults with nonmalignant pain. Pain 157(12):2834–2842. https://doi.org/10.1097/j.pain.0000000000000719
Lin CP, Kupper AE, Gammaitoni AR, Galer BS, Jensen MP (2011) Frequency of chronic pain descriptors: implications for assessment of pain quality. Eur J Pain 15(6):628–633. https://doi.org/10.1016/j.ejpain.2010.11.006
Arning K, Baron R (2009) Evaluation of symptom heterogeneity in neuropathic pain using assessments of sensory functions. Neurotherapeutics 6(4):738–748. https://doi.org/10.1016/j.nurt.2009.07.002
Baron R, Tolle TR (2008) Assessment and diagnosis of neuropathic pain. Current Opinion in Supportive and Palliative Care 2(1):1–8
Mystakidou K, Parpa E, Tsilika E, Pathiaki M, Galanos A, Vlahos L (2007) Comparison of pain quality descriptors in cancer patients with nociceptive and neuropathic pain. In Vivo 21(1):93–98. https://doi.org/10.1016/S0885-3924(01)00351-7
Loprinzi CL, Reeves BN, Dakhil SR, Sloan JA, Wolf SL, Burger KN, Kamal A, le-Lindqwister NA, Soori GS, Jaslowski AJ, Novotny PJ, Lachance DH (2011) Natural history of paclitaxel-associated acute pain syndrome: prospective cohort study NCCTG N08C1. J Clin Oncol 29(11):1472–1478. https://doi.org/10.1200/JCO.2010.33.0308
Finnerup NB, Norrbrink C, Trok K, Piehl F, Johannesen IL, Sørensen JC, Jensen TS, Werhagen L (2014) Phenotypes and predictors of pain following traumatic spinal cord injury: a prospective study. J Pain 15(1):40–48. https://doi.org/10.1016/j.jpain.2013.09.008
Gibbs GF, Drummond PD, Finch PM, Phillips JK (2008) Unravelling the pathophysiology of complex regional pain syndrome: focus on sympathetically maintained pain. Clin Exp Pharmacol Physiol 35(7):717–724. https://doi.org/10.1111/j.1440-1681.2007.04862.x
Boureau F, Doubrere JF, Luu M (1990) Study of verbal description in neuropathic pain. Pain 42(2):145–152. https://doi.org/10.1016/0304-3959(90)91158-F
Wilkie DJ, Molokie R, Boyd-Seal D, Suarez ML, Kim YO, Zong S, Wittert H, Zhao Z, Saunthararajah Y, Wang ZJ (2010) Patient-reported outcomes: descriptors of nociceptive and neuropathic pain and barriers to effective pain management in adult outpatients with sickle cell disease. J Natl Med Assoc 102(1):18–27. https://doi.org/10.1016/S0027-9684(15)30471-5
Kramer BJ, Harker JO, Wong AL (2002) Descriptions of joint pain by American Indians: comparison of inflammatory and noninflammatory arthritis. Arthritis Rheum 47(2):149–154. https://doi.org/10.1002/art1.10325
Epstein JB, Wilkie DJ, Fischer DJ, Kim Y-O, Villines D (2009) Neuropathic and nociceptive pain in head and neck cancer patients receiving radiation therapy. Head & Neck Oncology 1(1):26–38. https://doi.org/10.1186/1758-3284-1-26
Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, Cunin G, Fermanian J, Ginies P, Grun-Overdyking A, Jafari-Schluep H, Lantéri-Minet M, Laurent B, Mick G, Serrie A, Valade D, Vicaut E (2005) Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 114(1–2):29–36. https://doi.org/10.1016/j.pain.2004.12.010
Butler S, Jonzon B, Branting-Ekenback C, Wadell C, Farahmand B (2013) Predictors of severe pain in a cohort of 5271 individuals with self-reported neuropathic pain. Pain 154(1):141–146. https://doi.org/10.1016/j.pain.2012.10.001
Wilkie DJ, Huang H-Y, Reilly NL, Cain KC (2001) Nociceptive and neuropathic pain in patients with lung cancer: a comparison of pain quality descriptors. J Pain Symptom Manag 22(5):899–910
Backonja MM, Stacey B (2004) Neuropathic pain symptoms relative to overall pain rating. J Pain 5(9):491–497. https://doi.org/10.1016/j.jpain.2004.09.001
Rasmussen PV, Sindrup SH, Jensen TS, Bach FW (2004) Symptoms and signs in patients with suspected neuropathic pain. Pain 110:461–469. https://doi.org/10.1016/j.pain.2004.04.034
Freeman R, Baron R, Bouhassira D, Cabrera J, Emir B (2014) Sensory profiles of patients with neuropathic pain based on the neuropathic pain symptoms and signs. Pain 155(2):367–376. https://doi.org/10.1016/j.pain.2013.10.023
Tofthagen CS, McMillan SC (2010) Pain, neuropathic symptoms, and physical and mental well-being in persons with cancer. Cancer Nurs 33(6):436–444. https://doi.org/10.1097/NCC.0b013e3181e212b4.Pain
Makker PGS, Duffy SS, Lees JG, Perera CJ, Tonkin RS, Butovsky O, Park SB, Goldstein D, Moalem-Taylor G (2017) Characterisation of immune and neuroinflammatory changes associated with chemotherapy-induced peripheral neuropathy. PLoS One 12(1):1–24. https://doi.org/10.1371/journal.pone.0170814
Chiu N, Zhang L, Gallo-Hershberg D, Dent R, Chiu L, Pasetka M, van Draanen J, Chow R, Lam H, Verma S, Stinson J, Stacey E, Chow E, DeAngelis C (2016) Which pain intensity scale from the brief pain inventory correlates most highly with functional interference scores in patients experiencing taxane-induced arthralgia and myalgia? Support Care Cancer 24(7):2979–2988. https://doi.org/10.1007/s00520-016-3106-5
Zheng FY, Xiao WH, Bennett GJ (2011) The response of spinal microglia to chemotherapy-evoked painful peripheral neuropathies is distinct from that evoked by traumatic nerve injuries. Neuroscience 176:447–454. https://doi.org/10.1016/j.neuroscience.2010.12.052
Ren K, Dubner R (2010) Interactions between the immune and nervous systems in pain. Nat Med 16(11):1267–1276. https://doi.org/10.1038/nm.2234
Ueda H (2006) Molecular mechanisms of neuropathic pain-phenotypic switch and initiation mechanisms. Pharmacol Ther 109(1–2):57–77. https://doi.org/10.1016/j.pharmthera.2005.06.003
Dahl JB, Møiniche S (2004) Pre-emptive analgesia. Br Med Bull 71(December):13–27. https://doi.org/10.1093/bmb/ldh030
Funding
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund. The funding sources were not involved in the study design, data collection, analyses and interpretation of the data, manuscript writing, and the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Conception and design: Carlo De Angelis, Edward Chow, Daniela Gallo-Hershberg, Angie Giotis, Jenna van Draanen.
Data management: Daniela Gallo-Hershberg, Angie Giotis, Jenna van Draanen, Shannon Goodall.
Analysis and interpretation: Carlo De Angelis, Rashi Asthana, Liying Zhang.
Drafting of the article: Rashi Asthana, Bo Angela Wan, Patrick Diaz.
Revision of the article: all authors.
Final approval of the version: all authors.
Agreement to be accountable for all aspects of the work: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 63 kb)
Rights and permissions
About this article
Cite this article
Asthana, R., Zhang, L., Wan, B.A. et al. Pain descriptors of taxane acute pain syndrome (TAPS) in breast cancer patients—a prospective clinical study. Support Care Cancer 28, 589–598 (2020). https://doi.org/10.1007/s00520-019-04845-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04845-7