Abstract
Purpose
Perioperative oral care is effective for the prevention and reduction of complications following surgery. However, oral cancer patients’ oral health is often poor. During hospitalization, oral cancer patients frequently receive oral care from ward nurses as well as professional oral care from dental hygienists. Maintenance of good oral hygiene in these patients ideally requires cooperation between nurses and dental hygienists. Consequently, communication tools used to share information about the status of patients’ oral health are needed. One such tool is the Oral Assessment Guide (OAG). However, the inter-rater reliability of the OAG has not been consistently reported; therefore, we examined this between nurses and dental hygienists.
Methods
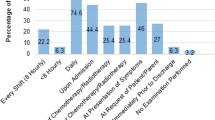
Participants comprised 76 patients hospitalized for oral cancer treatment. After surgery, a nurse and a dental hygienist performed oral assessments using the OAG. Comparative statistical analyses were conducted to examine differences and consistencies in the scores of nurses and dental hygienists.
Results
Although almost all patients’ oral health status was poor, none were given the worst score in the mucous membrane or gingiva categories. Further, the tongue, saliva, mucous membrane, gingiva, and teeth/denture categories had low κ coefficients, indicating poor nurse–dental hygienist inter-rater reliability. In contrast, the κ coefficients and agreement rates for voice and swallowing were high. Dental hygienists’ scores were significantly higher for the tongue, gingiva, and teeth/denture categories than were nurses’ scores.
Conclusions
This study showed low nurse–dental hygienist inter-rater reliability for the OAG and highlighted the difficulties in objectively assessing patients’ symptoms and oral health conditions. Therefore, rather than only relying on an objective assessment of symptoms by a clinician, assessments should also include patients’ subjective reporting of symptoms. OAG will likely be used until a new assessment tool is developed. Objective assessment training and/or user manual development may be required to improve the reliability of OAG. The present training of one lesson a year is insufficient, and efforts should be made to improve this to get more reliable outcomes.
Similar content being viewed by others
References
Mori H, Hirasawa H, Oda S, Shiga H, Matsuda K, Nakamura M (2006) Oral care reduces incidence of ventilator-associated pneumonia in ICU populations. Intensive Care Med 32:230–236. https://doi.org/10.1007/s00134-005-0014-4
Yoneyama T, Yoshida M, Matsui T, Sasaki H (1999) Oral care and pneumonia. Oral care working group. Lancet 354:515. https://doi.org/10.1016/s0140-6736(05)75550-1
McGuire DB, Fulton JS, Park J, Brown CG, Correa ME, Eilers J, Elad S, Gibson F, Oberle-Edwards LK, Bowen J, Lalla RV (2013) Systematic review of basic oral care for the management of oral mucositis in cancer patients. Support Care Cancer 21:3165–3177. https://doi.org/10.1007/s00520-013-1942-0
Saito H, Watanabe Y, Sato K, Ikawa H, Yoshida Y, Katakura A, Takayama S, Sato M (2014) Effects of professional oral health care on reducing the risk of chemotherapy-induced oral mucositis. Support Care Cancer 22:2935–2940. https://doi.org/10.1007/s00520-014-2282-4
Yoneyama T, Yoshida M, Ohrui T, Mukaiyama H, Okamoto H, Hoshiba K, Ihara S, Yanagisawa S, Ariumi S, Morita T, Mizuno Y, Ohsawa T, Akagawa Y, Hashimoto K, Sasaki H (1996) Oral hygiene reduces respiratory infections in elderly bed-bound nursing home patients. Arch Gerontol Geriatr 22:11–19. https://doi.org/10.1046/j.1532-5415.2002.50106.x
Schwendicke F, Stolpe M, Müller F (2017) Professional oral healthcare for preventing nursing home-acquired pneumonia: a cost-effectiveness and value of information analysis. J Clin Periodontol 13:1236–1244. https://doi.org/10.1111/jcpe.12775
Pfister DG, Spencer S, Brizel DM, Burtness B, Busse PM, Caudell JJ, Cmelak AJ, Colevas AD, Dunphy F, Eisele DW, Foote RL, Gilbert J, Gillison ML, Haddad RI, Haughey BH, Hicks WL Jr, Hitchcock YJ, Jimeno A, Kies MS, Lydiatt WM, Maghami E, McCaffrey T, Mell LK, Mittal BB, Pinto HA, Ridge JA, Rodriguez CP, Samant S, Shah JP, Weber RS, Wolf GT, Worden F, Yom SS, McMillian N, Hughes M (2015) Head and neck cancers, version 1.2015. J Natl Compr Cancer Netw 13:847–855. https://doi.org/10.6004/jnccn.2015.0102
Shigeishi H, Ohta K, Fujimoto S, Nakagawa T, Mizuta K, Ono S, Shimasue H, Ninomiya Y, Higashikawa K, Tada M, Ishida F, Okui G, Okumura T, Fukui A, Kubozono K, Yamamoto K, Ishida Y, Seino S, Hashikata M, Sasaki K, Naruse T, Rahman MZ, Uetsuki R, Nimiya A, Takamoto M, Dainobu K, Tokikazu T, Nishi H, Sugiyama M, Takechi M (2016) Preoperative oral health care reduces postoperative inflammation and complications in oral cancer patients. Exp Ther Med 12:1922–1928. https://doi.org/10.3892/etm.2016.3532
Sakamoto H, Sasaki J, Nord CE (1999) Association between bacterial colonization on the tumor, bacterial translocation to the cervical lymph nodes and subsequent postoperative infection in patients with oral cancer. Clin Microbiol Infect 5:612–616. https://doi.org/10.1111/j.1469-0691.1999.tb00417.x
Eilers J, Berger AM, Peterson MC (1988) Development, testing, and application of the oral assessment guide. Oncol Nurs Forum 15:325–330
Knoos MM, Ostman M (2010) Oral assessment guide—test of reliability and validity for patients receiving radiotherapy to the head and neck region. Eur J Cancer Care 19:53–60. https://doi.org/10.1111/j.1365-2354.2008.00958.x
Andersson P, Persson L, Hallberg IR, Renvert S (1999) Testing an oral assessment guide during chemotherapy treatment in a Swedish care setting: a pilot study. J Clin Nurs 8:150–158. https://doi.org/10.1046/j.1365-2702.1999.00237.x
Andersson P, Hallberg IR, Renvert S (2002) Inter-rater reliability of an oral assessment guide for elderly patients residing in a rehabilitation ward. Spec Care Dentist 22:181–186. https://doi.org/10.1111/j.1754-4505.2002.tb00268.x
Paulsson G, Wårdh I, Andersson P, Ohrn K (2008) Comparison of oral health assessments between nursing staff and patients on medical wards. Eur J Cancer Care 17:49–55. https://doi.org/10.1111/j.1365-2354.2007.00802.x
Shiraishi A, Yoshimura Y, Wakabayashi H, Tsuji Y (2017) Poor oral status is associated with rehabilitation outcome in older people. Geriatr Gerontol Int 17:598–604. https://doi.org/10.1111/ggi.12763
Basch E (2014) New frontiers in patient-reported outcomes: adverse event reporting, comparative effectiveness, and quality assessment. Ann Rev Med 65:307–317. https://doi.org/10.1146/annurev-med-010713-141500
U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Biologics Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health (2006) Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes 4:79
Basch E (2010) The missing voice of patients in drug-safety reporting. N Engl J Med 362:865–869. https://doi.org/10.1056/nejmp0911494
Basch E, Iasonos A, McDonough T, Barz A, Culkin A, Kris MG, Scher HI, Schrag D (2006) Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: results of a questionnaire-based study. Lancet Oncol 7:903–909. https://doi.org/10.1016/s1470-2045(06)70910-x
Basch EM, Reeve BB, Mitchell SA, Clauser SB, Minasian L, Sit L, Chilukuri R, Baumgartner P, Rogak L, Blauel E, Abernethy AP, Bruner D (2011) Electronic toxicity monitoring and patient-reported outcomes. Cancer J 17:231–234. https://doi.org/10.1097/ppo.0b013e31822c28b3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Board for Clinical Research at Tokai University School of Medicine (16R-163). This clinical research was conducted in accordance with the Declaration of Helsinki as well as the Ethical Guidelines for Clinical Research by the Japanese Ministry of Health, Labour and Welfare. Written informed consent was obtained from each patient after an explanation of the study protocol. To protect personal information, the obtained data was managed by “anonymity with linking capability.”
Competing interests
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Aoki, T., Kudo, M., Endo, M. et al. Inter-rater reliability of the Oral Assessment Guide for oral cancer patients between nurses and dental hygienists: the difficulties in objectively assessing oral health. Support Care Cancer 27, 1673–1677 (2019). https://doi.org/10.1007/s00520-018-4412-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4412-x