Abstract
Purpose
This study investigated satisfaction with treatment decision (SWTD), decision-making preferences (DMP), and main treatment goals, as well as evaluated factors that predict SWTD, in patients receiving palliative cancer treatment at a Swiss oncology network.
Patients and methods
Patients receiving a new line of palliative treatment completed a questionnaire 4–6 weeks after the treatment decision. Patient questionnaires were used to collect data on sociodemographics, SWTD (primary outcome measure), main treatment goal, DMP, health locus of control (HLoC), and several quality of life (QoL) domains. Predictors of SWTD (6 = worst; 30 = best) were evaluated by uni- and multivariate regression models.
Results
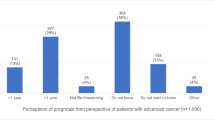
Of 480 participating patients in eight hospitals and two private practices, 445 completed all questions regarding the primary outcome measure. Forty-five percent of patients preferred shared, while 44 % preferred doctor-directed, decision-making. Median duration of consultation was 30 (range: 10–200) minutes. Overall, 73 % of patients reported high SWTD (≥24 points). In the univariate analyses, global and physical QoL, performance status, treatment goal, HLoC, prognosis, and duration of consultation were significant predictors of SWTD. In the multivariate analysis, the only significant predictor of SWTD was duration of consultation (p = 0.01). Most patients indicated hope for improvement (46 %), followed by hope for longer life (26 %) and better quality of life (23 %), as their main treatment goal.
Conclusion
Our results indicate that high SWTD can be achieved in most patients with a 30-min consultation. Determining the patient’s main treatment goal and DMP adds important information that should be considered before discussing a new line of palliative treatment.


Similar content being viewed by others
References
Korsch BM, Gozzi EK, Francis V (1968) Gaps in doctor–patient communication. 1. Doctor–patient interaction and patient satisfaction. Pediatrics 42:855–871
Zachariae R, Pedersen CG, Jensen AB et al (2003) Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br J Cancer 88:658–665
Hall JA, Roter DL, Katz NR (1988) Meta-analysis of correlates of provider behavior in medical encounters. Med Care 26:657–675
Epstein RM, Street R Jr (2007) Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, Bethesda
Leighl NB, Shepherd HL, Butow PN et al (2011) Supporting treatment decision making in advanced cancer: a randomized trial of a decision aid for patients with advanced colorectal cancer considering chemotherapy. J Clin Oncol 29:2077–2084
Degner LF, Kristjanson LJ, Bowman D et al (1997) Information needs and decisional preferences in women with breast cancer. JAMA 277:1485–1492
Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, Schrag D (2012) Patients’ expectations about effect of chemotherapy for advanced cancer. NEJM 367:1616–1625
Leighl NB, Butow PN, Tattersall MHN (2004) Treatment decision aids in advanced cancer: when the goal is not cure and the answer is not clear. J Clin Oncol 22:1759–1762
O’Connor AM, Rostom A, Fiset V, Tetroe J, Entwistle V, Llewellyn-Thomas H, Holmes-Rovner M, Barry M, Jones J (1999) Decision aids for patients facing health treatment or screening decisions: systemic review. BMJ 319:731–734
Molenaar S, Sprangers MA, Postma- Schmit FC et al (2000) Feasibility and effects of decision aids. Med Decis Making 20:112–127
Committee on Quality of Health Care in America IoM (2001) Crossing the quality chasm: a new health system for the 21st century. National Academies Press, Washington, DC
Kuehn BM (2012) Patient-centered care model demands better physician–patient communication. JAMA 307:441–442
Kissane DW, Bylund CL, Banerjee SC, Bialer PA, Levin TT, Maloney EK, D’Agostino TA (2012) Communication skills training for oncology professionals. J Clin Oncol 30:1242–1247
Haidet P, Fecile ML, West HF et al (2009) Reconsidering the team concept: educational implications for patient-centered cancer care. Patient Educ Couns 77:450–455
Politi MC, Studts JL, Hayslip JW (2012) Shared decision making in oncology practice: what do oncologists need to know? Oncologist 17:91–100
Daneault S, Dion D, Sicotte C, Yelle L, Mongeau S, Lussier V, Coulombe M, Paillé P (2010) Hope and noncurative chemotherapies: which affects the other? J Clin Oncol 28:2310–2313
Ware JE Jr, Snyder MK, Wright WR et al (1983) Defining and measuring patient satisfaction with medical care. Eval Program Plann 6:247–263
Holmes-Rovner M, Kroll J, Schmitt N et al (1996) Patient satisfaction with health care decisions: the satisfaction with decision scale. Med Decis Making 16:58–64
Degner LF, Sloan JA, Venkatesh P (1997) The Control Preferences scale. Can J Nurs Res 29:21–43
Lohaus A, Schmitt GM (1989) Control beliefs concerning illness and health: report on the development of a testing procedure. Diagnostica 35:59–72
Wallston KA, Wallston BS, DeVellis R (1978) Development of the Multidimensional Health Locus of Control (MHLC) scales. Health Educ Monogr 6:160–170
Butow P, Coates A, Dunn S, Bernhard J, Hurny C (1991) On the receiving end. IV: validation of quality of life indicators. Ann Oncol 2:597–603
Bernhard J, Maibach R, Thurlimann B et al (2002) Patients’ estimation of overall treatment burden: why not ask the obvious? J Clin Oncol 20:65–72
Hürny C, Wegberg B, Bacchi M, Bernhard J, Thürlimann B, Real O, Perey L, Bonnefoi H, Coates A (1998) Subjective health estimations (SHE) in patients with advanced breast cancer: an adapted utility concept for clinical trials. Br J Cancer 77:985–991
Bernhard J, Dietrich D, Scheithauer W et al (2008) Clinical benefit and quality of life in patients with advanced pancreatic cancer receiving gemcitabine plus capecitabine versus gemcitabine alone: a randomized multicenter phase III clinical trial—SAKK 44/00-CECOG/PAN.1.3.001. J Clin Oncol 26:3695–3701
Kollbrunner J, Zbaren P, Quack K (2001) Quality of life stress in patients with large tumors of the mouth. 2: Dealing with the illness: coping, anxiety and depressive symptoms. HNO 49:998–1007
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Taylor & Francis, New York
Cronbach LJ (1951) Coefficient alpha and the internal structure of tests. Psychometrika 16:297–334
Van Buuren S, Groothuis-Oudshoorn K (2011) Multivariate imputation by chained equations in R. J Stat Softw 45:1–67
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46
Deveugele M, Derese A, van den Brink-Muinen A et al (2002) Consultation length in general practice: cross sectional study in six European countries. BMJ 325:472
Hamidou Z, Dabakuyo TS, Bonnetain F (2011) Impact of response shift on longitudinal quality-of-life assessment in cancer clinical trials. Expert Rev Pharmacoecon Outcomes Res 11:549–559
Stewart M, Brown JB, Donner A (2000) The impact of patient-centered care on outcomes. J Fam Pract 49:796–804
Makoul G, Arntson P, Schofield T (1995) Health promotion in primary care: physician–patient communication and decision making about prescription medications. Soc Sci Med 41:1241–1254
Barry MJ, Edgman-Levitan S (2012) Shared decision making—pinnacle of patient-centered care. N Engl J Med 366:780–781
Bruera E, Sweeney C, Calder K, Palmer L, Benisch-Tolley S (2001) Patient preferences versus physician perceptions of treatment decisions in cancer care. J Clin Oncol 19:2883–2885
Elkin EB, Kim SH, Casper ES, Kissane DW, Schrag D (2007) Desire for information and involvement in treatment decisions: elderly cancer patients’ preferences and their physicians’ perceptions. J Clin Oncol 25:5275–5280
Bruera E, Willey JS, Palmer JL, Rosales M (2002) Treatment decisions for breast carcinoma: patient preferences and physician perceptions. Cancer 94:2076–2080
Mandelblatt J, Kreling B, Figeuriedo M, Feng S (2006) What is the impact of shared decision making on treatment and outcomes for older women with breast cancer? J Clin Oncol 24:4908–4913
Janz NK, Wren PA, Copeland LA, Lowery JC, Goldfarb SL, Wilkins EG (2004) Patient–physician concordance: preferences, perceptions, and factors influencing the breast cancer surgical decision. J Clin Oncol 22:3091–3098
Gattellari M, Butow PN, Tattersall MH (2001) Sharing decisions in cancer care. Soc Sci Med 52:1865–1878
Noble LM, Kubacki A, Martin J, Lloyd M (2007) The effect of professional skills training on patient-centredness and confidence in communicating with patients. Med Educ 41:432–440
Voogt E, van der Heide A, Rietjens JA et al (2005) Attitudes of patients with incurable cancer toward medical treatment in the last phase of life. J Clin Oncol 23:2012–2019
Stiggelbout AM, de Haes JC, Kiebert GM et al (1996) Tradeoffs between quality and quantity of life: development of the QQ Questionnaire for Cancer Patient Attitudes. Med Decis Making 16:184–192
Renz M, Koeberle D, Cerny T, Strasser F (2008) Between utter despair and essential hope. J Clin Oncol 27:146–149
Acknowledgments
The authors would like to thank Margit Hemetsberger (Hemetsberger Medical Services, Vienna, Austria), Eva Müller (Lifescience Texte, Vienna, Austria), and Julia Balfour (Northstar Medical Writing and Editing Services, Dundee, UK), who assisted with the preparation of this manuscript and were funded by the Kantonsspital St. Gallen, Switzerland. The authors also thank Ivo Betschard for data preparation, and all patients, oncologists, and nurses at each participating center.
Funding
This study was supported by OSKK (Ostschweizer Stiftung für Klinische Krebsforschung).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 108 kb)
Rights and permissions
About this article
Cite this article
Hitz, F., Ribi, K., Li, Q. et al. Predictors of satisfaction with treatment decision, decision-making preferences, and main treatment goals in patients with advanced cancer. Support Care Cancer 21, 3085–3093 (2013). https://doi.org/10.1007/s00520-013-1886-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1886-4