Abstract
Purpose
The incorporation of three-dimensional (3D) planning for the treatment of bone metastases has been embraced in many North American practices with assumed superior tumor targeting, sparing of normal structures, and improvement in patient outcomes. The goal of our project was to evaluate the dosimetric and clinical impact of 3D vs. two-dimensional (2D) planning for patients who require simple palliative radiotherapy techniques (≤2 beams) for bone metastases.
Methods
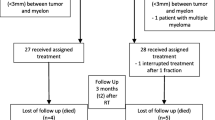
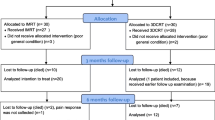
Patients undergoing palliative radiation therapy for bone metastases were eligible. The study oncologists first documented the intended treatment target, defined the treatment target/field using digital radiographs (2D), followed by using full 3D planning computerized tomography volumetric datasets. Treatment plans were compared dosimetrically, and patient-reported outcomes (pain, fatigue, anorexia, and nausea) were compared against a historical cohort treated with 2D plans.
Results
Eighty-five patients were enrolled in the study group. Review of the 3D datasets led to changes in the target area of interest in 44/85 (52 %) of cases, of which 21/85 (25 %) were clinically significant. 3D plans resulted in superior target coverage and normal tissue sparing. There was no significant difference in patient-reported outcomes however.
Conclusion
3D radiotherapy planning resulted in superior treatment plans but we were unable to demonstrate a significant benefit in clinical outcomes. Prospective study designs are needed to describe the contemporary expectation of palliative radiotherapy for bone metastases in the modern era of 3D planning.



Similar content being viewed by others
References
Mackillop WJ (1996) The principles of palliative radiotherapy: a radiation oncologist’s perspective. Can J Oncol 6(Suppl 1):5–11
Haddad P et al (2004) Computed tomographic simulation in palliative radiotherapy: the Princess Margaret Hospital experience. Clin Oncol (R Coll Radiol) 16(6):425–8
Aird EG, Conway J (2002) CT simulation for radiotherapy treatment planning. Br J Radiol 75(900):937–49
Jaffray D et al (2007) Review of image-guided radiation therapy. Expert Rev Anticancer Ther 7(1):89–103
Haddad P et al (2006) Computerized tomographic simulation compared with clinical mark-up in palliative radiotherapy: a prospective study. Int J Radiat Oncol Biol Phys 65(3):824–9
McJury M et al (2001) The impact of virtual simulation in palliative radiotherapy for non-small-cell lung cancer. Radiother Oncol 59(3):311–8
Gripp S et al (1999) The role of CT simulation in whole-brain irradiation. Int J Radiat Oncol Biol Phys 45(4):1081–8
Feuvret L et al (2006) Conformity index: a review. Int J Radiat Oncol Biol Phys 64(2):333–42
Lefkopoulos, D., et al. (2000) Determination of dose-volumes parameters to characterise the conformity of stereotactic treatment plans. In: XIIIth International Conference on: “Computers in Radiation Therapy.” Heidelberg, Germany. p. 356–358
Lomax NJ, Scheib SG, Scheib SG (2003) Quantifying the degree of conformity in radiosurgery treatment planning. Int J Radiat Oncol Biol Phys 55(5):1409–19
Caraceni A et al (2002) Pain measurement tools and methods in clinical research in palliative care: recommendations of an Expert Working Group of the European Association of Palliative Care. J Pain Symptom Manag 23(3):239–55
Chow E et al (2012) Update of the international consensus on palliative radiotherapy endpoints for future clinical trials in bone metastases. Int J Radiat Oncol Biol Phys 82(5):1730–7
Chow E et al (2012) Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol) 24(2):112–24
Ratanatharathorn V et al (1999) Bone metastasis: review and critical analysis of random allocation trials of local field treatment. Int J Radiat Oncol Biol Phys 44(1):1–18
Grabarz D et al (2011) Quantifying interobserver variation in target definition in palliative radiotherapy. Int J Radiat Oncol Biol Phys 80(5):1498–504
Lutz S et al (2011) Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys 79(4):965–76
Andic F et al (2009) A dosimetric comparison of different treatment plans of palliative spinal bone irradiation: analysis of dose coverage with respect to ICRU 50 Report. J Exp Clin Cancer Res 28:2
Sutton DS et al (2010) The use of palliative radiotherapy for bone metastasis. Radiother Oncol 97(3):548–53
Acknowledgments
This study was supported in part by the Kerbel Research Fund. The authors would like to thank Ms. Shawde Harris for her editorial support.
Conflict of interest
The authors have no conflict of interest to report. The authors have full control of all primary data. The authors would allow the journal to review data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pope, K., Fitzpatrick, D., Potter, A. et al. Dosimetric and clinical impact of 3D vs. 2D planning in palliative radiotherapy for bone metastases. Support Care Cancer 21, 2229–2235 (2013). https://doi.org/10.1007/s00520-013-1777-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1777-8