Summary
Background/aim
The relationship between nonalcoholic fatty liver disease (NAFLD) and coronary heart disease (CHD) is poorly understood. In the present study, we aimed to assess the frequency of NAFLD in CHD patients by using a new diagnostic tool: transient elastography (TE; Fibroscan®-CAP). Clarification of the present study may help to provide a new noninvasive tool for the assessment of NAFLD in this specific population of patients and may be of clinical importance in planning preventive strategies in high-risk patients.
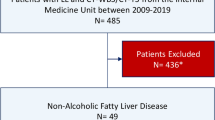
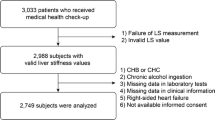
Patients and methods
A total of 75 patients with proven CHD were enrolled. Liver stiffness was used to assess liver fibrosis, and controlled attenuation parameter (CAP) was used to detect and quantify liver steatosis by using Fibroscan® (Echosens, Paris, France). By CAP being implemented on TE, both liver steatosis and fibrosis can be evaluated simultaneously.
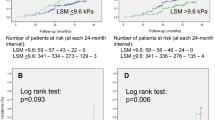
Results
Of the 75 patients, 45 (60 %) had CAP > 238 dBm−1 and, by definition, NAFLD. Among the patients with NAFLD, 24 (53.3 %) had, in addition, liver stiffness > 7 kPa. Analyzing the influence of the degree of liver steatosis (expressed by CAP values) on the degree of CHD (defined by single or multiple vessels involved), we found that patients with multiple vessels involved had higher CAP values (p = 0.002). Furthermore, we noticed that significantly more patients with multiple vessels involved had liver stiffness > 7 kPa (p < 0.0001) indicating the more severe form of NAFLD in those patients.
Conclusion
The main finding of our study is that TE provides the opportunity of noninvasive screening for NAFLD in CHD patients, as it is a quick, simple, reliable, and repeatable method and more cost-effective than liver biopsy.
Zusammenfassung
Hintergrund/Ziel der Studie
Der Zusammenhang zwischen der NAFLD und der CHD ist unklar. In der vorliegenden Studie wollten wir die Häufigkeit einer NAFLD bei Patienten mit einer CHD unter Verwendung eines neuen diagnostischen Gerätes (TE – Transiente Elastographie; Fibroscan®- CAP) erheben. Die Ergebnisse unserer Studie könnten helfen, ein neues nicht-invasives Gerät zur Erfassung einer NAFLD bei dieser besonderen Patientenpopulation einzusetzen. Der klinische Nutzen könnte in der darauf basierenden Planung einer präventiven Strategie bei Hochrisikopatienten liegen.
Patienten und Methodik
Es wurden 75 Patienten mit nachgewiesener CHD in die Studie aufgenommen. Die Steifheit der Leber wurde zur Beurteilung einer möglichen Leberfibrose herangezogen. Der „Controlled Attenuation Parameter (CAP)“ wurde mit Hilfe eines Fibroscan® (Echosens, Paris, Frankreich) erhoben und zur Erkennung und Quantifizierung einer möglichen Lebersteatose eingesetzt. Durch die Einbeziehung der CAP in die TE kann sowohl die Steatose als auch die Fibrose der Leber beurteilt werden.
Ergebnisse
Von den 75 Patienten hatten 45 (= 60 %) ein CAP > 238 dBm−1 und damit per definitionem eine NAFLD. Von diesen Patienten mit NAFLD hatten 24 (= 53,3 %) eine Lebersteife > 7 kPa.Die Analyse eines möglichen Zusammenhangs zwischen dem Grad der Lebersteatose (ausgedrückt in CAP Werten) mit dem Schweregrad der CHD (definiert durch die Anzahl der befallenen Gefäße) ergab, dass Patienten mit einer Mehrgefäßerkrankung höhere CAP Werte (p = 0,002) aufwiesen. Auch eine Lebersteife > 7 kPa wurde bei diesen Patienten mit Mehrgefäßbefall signifikant häufiger erhoben.
Schlussfolgerung
Unsere Studie zeigt, dass die TE die Möglichkeit eines nicht-invasiven Screenings auf NAFLD bei CHD Patienten bietet. Die Methode ist ein rasches, einfaches, verlässliches und reproduzierbares Verfahren, – kosteneffizienter als eine Leberbiopsie.
Similar content being viewed by others
References
Milic S, Stimac D. Nonalcoholic fatty liver disease/steatohepatitis: epidemiology, pathogenesis, clinical presentation and treatment. Dig Dis. 2012;30:158–62.
Targher G, Marra F, Marchesini G. Increased risk of cardiovascular disease in non-alcoholic fatty liver disease: causal effect or epiphenomenon? Diabetologia. 2008;51:1947–53.
Villanova N, Moscatiello S, Ramilli S, et al. Endothelial dysfunction and cardiovascular risk profile in nonalcoholic fatty liver disease. Hepatology. 2005;42:473–80.
Dowman JK, Tomlinson JW, Newsome PN. Systematic review: the diagnosis and staging of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2011;33:525–40.
Targher G, Arcaro G. Non-alcoholic fatty liver disease and increased risk of cardiovascular disease. Atherosclerosis. 2007;191:235–40.
Kim CH, Younossi ZM. Non alcoholic fatty liver disease: a manifestation of metabolic syndrome. Cleve Clin J Med. 2008;75:721–8.
Targher G. Non-alcoholic fatty liver disease, the metabolic syndrome and the risk of cardiovascular disease: the plot thickens. Diabet Med. 2007;24:1–6.
Martinez SM, Crespo G, Navasa M, Forns X. Noninvasive assessment of liver fibrosis. Hepatology. 2011;53:325–35.
Chowdhury SD, Ramakrishna B, Eapen CE, Goel A, Zachariah UG, Chandramohan A, et al. Fibrosis in non-alcoholic fatty liver disease: correlation with simple blood indices and association with tumor necrosis factor-alpha polymorphisms. Trop Gastroenterol. 2013;34:31–5.
Celikbilek M, Dogan S, Gursoy S, Zararsız G, Yurci A, Ozbakır O, et al. Noninvasive assessment of liver damage in chronic hepatitis B. World J Hepatol. 2013;5:439–45.
Leroy V, Hilleret MN, Sturm N, Trocme C, Renversez JC, Faure P, et al. Prospective comparison of six non-invasive scores for the diagnosis of liver fibrosis in chronic hepatitis C. J Hepatol. 2007;46:775–82.
Angulo P, Bugianesi E, Bjornsson ES, Charatcharoenwitthaya P, Mills PR, Barrera F, et al. Simple noninvasive systems predict long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2013;145:782–9.
Sasso M, Beaugrand M, dee Ledinghen V, et al. Controlled attenuation parameter (CAP): a novel VCTE guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol. 2010;36:1825–35.
Wong Lai-Hung G. Update of liver fibrosis and steatosis with transiet elastography (Fibroscan®). Gastroenterol Rep. 2013:1–8. doi:10.1093/gastro/got007.
Grundy SM, Cleeman JI, Daniels SR, et al; American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112:2735–52.
Inci MF, Özkan F, Ark B, et al. Sonographic evaluation for predicting the presence and severity of coronary artery disease. Ultrasound Q. 2013;29:125–30.
Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 2013;5:1544–60.
Ahmed MH, Barakat S, Almobarak AO. Nonalcoholic fatty liver disease and cardiovascular disease: has the time come for cardiologists to be hepatologists. J Obes. 2012;2012:483135.
Schindhelm RK, Diamant M, Bakker SJ, et al. Liver alanine aminotransferase, insulin resistance and endothelial dysfunction in normotriglyceridaemic subjects with type 2 diabetes mellitus. Eur J Clin Invest. 2005;35:369–74.
Goland S, Shimoni S, Zornitzki T, et al. Cardiac abnormalities as a new manifestation of nonalcoholic fatty liver disease: echocardiographic and tissue Doppler imaging assessment. J Clin Gastroenterol. 2006;40:949–55.
Targher G, Bertolini L, Padovani R, et al. Relations between carotid artery wall thickness and liver histology in subjects with nonalcoholic fatty liver disease. Diabetes Care. 2006;29:1325–30.
Fracanzani AL, Burdick L, Raselli S, et al. Carotid artery intima-media thickness in nonalcoholic fatty liver disease. Am J Med. 2008;121:72–8.
Cervera-Lizardi J, Zapata-Aguilar D. Nonalcoholic fatty liver disease and its association with cardiovascular disease. Ann Hepatol. 2009;8:40–3.
Schwimmer JB, Deutsch R, Behling C, et al. Fatty liver as a determinant of atherosclerosis. Hepatology. 2005;42:610A (abstract).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mikolasevic, I., Orlic, L., Milic, S. et al. Nonalcoholic fatty liver disease (NAFLD) proven by transient elastography in patients with coronary heart disease. Wien Klin Wochenschr 126, 474–479 (2014). https://doi.org/10.1007/s00508-014-0538-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0538-0