Abstract
Background
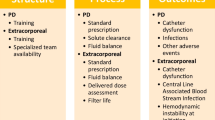
Infants with kidney failure (KF) demonstrate poor growth partly due to obligate fluid and protein restrictions. Delivery of liberalized nutrition on continuous kidney replacement therapy (CKRT) is impacted by clinical instability, technical dialysis challenges, solute clearance, and nitrogen balance. We analyzed delivered nutrition and growth in infants receiving CKRT with the Cardio-Renal, Pediatric Dialysis Emergency Machine (Carpediem™).
Methods
Single-center observational study of infants receiving CKRT with the Carpediem™ between June 1 and December 31, 2021. We collected prospective circuit characteristics, delivered nutrition, anthropometric measurements, and illness severity Score for Neonatal Acute Physiology-II. As a surrogate to normalized protein catabolic rate in maintenance hemodialysis, we calculated normalized protein nitrogen appearance (nPNA) using the Randerson II continuous dialysis model. Descriptive statistics, Spearman correlation coefficient, Mann Whitney, Wilcoxon signed rank, receiver operating characteristic curves, and Kruskal–Wallis analysis were performed using SAS version 9.4.
Results
Eight infants received 31.9 (22.0, 49.7) days of CKRT using mostly (90%) regional citrate anticoagulation. Delivered nutritional volume, protein, total calories, enteral calories, nPNA, and nitrogen balance increased on CKRT. Using parenteral nutrition, 90 ml/kg/day should meet caloric and protein needs. Following initial weight loss of likely fluid overload, exploratory sensitivity analysis suggests weight gain occurred after 14 days of CKRT. Despite adequate nutritional delivery, goal weight (z-score = 0) and growth velocity were not achieved until 6 months after CKRT start. Most (5 infants, 62.5%) survived and transitioned to peritoneal dialysis (PD).
Conclusions
Carpediem™ is a safe and efficacious bridge to PD in neonatal KF. Growth velocity of infants on CKRT appears delayed despite delivery of adequate calories and protein.
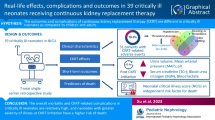
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the Baylor College of Medicine IRB on reasonable request.
References
Misurac J (2017) Chronic kidney disease in the neonate: etiologies, management, and outcomes. Semin Fetal Neonatal Med 22:98–103. https://doi.org/10.1016/j.siny.2016.09.003
Sanderson KR, Warady BA (2020) End-stage kidney disease in infancy: an educational review. Pediatr Nephrol 35:229–240. https://doi.org/10.1007/s00467-018-4151-8
Ranchin B, Plaisant F, Demède D et al (2021) Review: neonatal dialysis is technically feasible but ethical and global issues need to be addressed. Acta Paediatr 110:781–788. https://doi.org/10.1111/apa.15539
Symons JM, Brophy PD, Gregory MJ et al (2003) Continuous renal replacement therapy in children up to 10 kg. Am J Kidney Dis 41:984–989. https://doi.org/10.1016/S0272-6386(03)00195-1
Hepponstall M, Chan A, Monagle P (2017) Anticoagulation therapy in neonates, children and adolescents. Blood Cells Mol Dis 67:41–47. https://doi.org/10.1016/j.bcmd.2017.05.008
Inder TE, Perlman JM, Volpe JJ (2018) Intracranial hemorrhage. In: Volpe J, Inder T, Darras B et al (eds) Volpe’s neurology of the newborn. Elsevier, Philadelphia, pp 593–622
Garzotto F, Zanella M, Ronco C (2014) The evolution of pediatric continuous renal replacement therapy. Nephron Clin Pract 127:172–175. https://doi.org/10.1159/000363204
Garzotto F, Vidal E, Ricci Z et al (2020) Continuous kidney replacement therapy in critically ill neonates and infants: a retrospective analysis of clinical results with a dedicated device. Pediatr Nephrol 35:1699–1705. https://doi.org/10.1007/s00467-020-04562-y
Hay WW, Thureen P (2010) Protein for preterm infants: how much is needed? How much is enough? How much is too much? Pediatr Neonatol 51:198–207. https://doi.org/10.1016/S1875-9572(10)60039-3
Frondas-Chauty A, Simon L, Branger B et al (2014) Early growth and neurodevelopmental outcome in very preterm infants: impact of gender. Arch Dis Child Fetal Neonatal Ed 99:F366–F372. https://doi.org/10.1136/archdischild-2013-305464
Ehrenkranz RA, Dusick AM, Vohr BR et al (2006) Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 117:1253–1261. https://doi.org/10.1542/peds.2005-1368
Murphy HJ, Cahill JB, Twombley KE, Kiger JR (2018) Early continuous renal replacement therapy improves nutrition delivery in neonates during extracorporeal life support. J Ren Nutr 28:64–70. https://doi.org/10.1053/j.jrn.2017.06.008
Zappitelli M, Goldstein SL, Symons JM et al (2008) Protein and calorie prescription for children and young adults receiving continuous renal replacement therapy: a report from the Prospective Pediatric Continuous Renal Replacement Therapy Registry Group. Crit Care Med 36:3239–3245. https://doi.org/10.1097/CCM.0b013e31818f3f40
Wong Vega M, Juarez Calderon M, Tufan Pekkucuksen N et al (2019) Feeding modality is a barrier to adequate protein provision in children receiving continuous renal replacement therapy (CRRT). Pediatr Nephrol 34:1147–1150. https://doi.org/10.1007/s00467-019-04211-z
Ganesan MV, Annigeri RA, Shankar B et al (2009) The protein equivalent of nitrogen appearance in critically ill acute renal failure patients undergoing continuous renal replacement therapy. J Ren Nutr 19:161–166. https://doi.org/10.1053/j.jrn.2008.11.009
Macias WL, Alaka KJ, Murphy MH et al (1996) Impact of the nutritional regimen on protein catabolism and nitrogen balance in patients with acute renal failure. J Parenter Enteral Nutr 20:56–62. https://doi.org/10.1177/014860719602000156
Johnson RJ, Warady BA (2013) Long-term neurocognitive outcomes of patients with end-stage renal disease during infancy. Pediatr Nephrol 28:1283–1291. https://doi.org/10.1007/s00467-013-2458-z
Juarez-Congelosi M, Orellana P, Goldstein SL (2007) Normalized protein catabolic rate versus serum albumin as a nutrition status marker in pediatric patients receiving hemodialysis. J Ren Nutr 17:269–274. https://doi.org/10.1053/j.jrn.2007.04.002
Morse S, Groer M, Shelton MM et al (2015) A systematic review: the utility of the revised version of the score for neonatal acute physiology among critically ill neonates. J Perinat Neonatal Nurs 29:315–344. https://doi.org/10.1097/JPN.0000000000000135
van Stralen KJ, Borzych-Dużalka D, Hataya H et al (2014) Survival and clinical outcomes of children starting renal replacement therapy in the neonatal period. Kidney Int 86:168–174. https://doi.org/10.1038/ki.2013.561
Fenton TR, Chan HT, Madhu A et al (2017) Preterm infant growth velocity calculations: a systematic review. Pediatrics 139:e20162045. https://doi.org/10.1542/peds.2016-2045
Simon L, Hanf M, Frondas-Chauty A et al (2019) Neonatal growth velocity of preterm infants: the weight Z-score change versus Patel exponential model. PLoS One 14:e0218746. https://doi.org/10.1371/journal.pone.0218746
Sutherland SM, Davis AS, Powell D et al (2022) Kidney replacement therapy in low birth weight preterm newborns. Pediatrics 150:e2022056570. https://doi.org/10.1542/peds.2022-056570
Shaw V, Anderson C, Desloovere A et al (2023) Nutritional management of the infant with chronic kidney disease stages 2–5 and on dialysis. Pediatr Nephrol 38:87–103. https://doi.org/10.1007/s00467-022-05529-x
Shaw V, Polderman N, Renken-Terhaerdt J et al (2020) Energy and protein requirements for children with CKD stages 2–5 and on dialysis–clinical practice recommendations from the Pediatric Renal Nutrition Taskforce. Pediatr Nephrol 35:519–531. https://doi.org/10.1007/s00467-019-04426-0
Haffner D (2020) Strategies for optimizing growth in children with chronic kidney disease. Front Pediatr 8:399. https://doi.org/10.3389/fped.2020.00399
Mehls O, Wühl E, Tönshoff B et al (2008) Growth hormone treatment in short children with chronic kidney disease. Acta Paediatr 97:1159–1164. https://doi.org/10.1111/j.1651-2227.2008.00845.x
Drube J, Wan M, Bonthuis M et al (2019) Clinical practice recommendations for growth hormone treatment in children with chronic kidney disease. Nat Rev Nephrol 15:577–589. https://doi.org/10.1038/s41581-019-0161-4
Mekahli D, Shaw V, Ledermann SE, Rees L (2010) Long-term outcome of infants with severe chronic kidney disease. Clin J Am Soc Nephrol 5:10–17. https://doi.org/10.2215/CJN.05600809
Greenbaum LA, Muñoz A, Schneider MF et al (2011) The association between abnormal birth history and growth in children with CKD. Clin J Am Soc Nephrol 6:14–21. https://doi.org/10.2215/CJN.08481109
Goldstein SL, Akcan-Arikan A, Alobaidi R et al (2022) Consensus-based recommendations on priority activities to address acute kidney injury in children: a modified Delphi consensus statement. JAMA Netw Open 5:e2229442. https://doi.org/10.1001/jamanetworkopen.2022.29442
Nelms CL, Shaw V, Greenbaum LA et al (2021) Assessment of nutritional status in children with kidney diseases—clinical practice recommendations from the Pediatric Renal Nutrition Taskforce. Pediatr Nephrol 36:995–1010. https://doi.org/10.1007/s00467-020-04852-5
Young A, Brown LK, Ennis S et al (2021) Total body water in full-term and preterm newborns: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 106:542–548. https://doi.org/10.1136/archdischild-2020-321112
Laakkonen H, Happonen J-M, Marttinen E et al (2010) Normal growth and intravascular volume status with good metabolic control during peritoneal dialysis in infancy. Pediatr Nephrol 25:1529–1538. https://doi.org/10.1007/s00467-010-1535-9
Slagle CL, Riddle SL, McNelis K, Claes D (2022) Single-center experience on growth in infants born with end-stage kidney disease. J Ren Nutr 33:236–242. https://doi.org/10.1053/j.jrn.2022.09.007. (S1051227622001686)
Kritmetapak K, Peerapornratana S, Srisawat N et al (2016) The impact of macro-and micronutrients on predicting outcomes of critically ill patients requiring continuous renal replacement therapy. PLoS One 11:e0156634. https://doi.org/10.1371/journal.pone.0156634
Kalantar-Zadeh K, Supasyndh O, Lehn RS et al (2003) Normalized protein nitrogen appearance is correlated with hospitalization and mortality in hemodialysis patients with Kt/V greater than 1.20. J Ren Nutr 13:15–25. https://doi.org/10.1053/jren.2003.50005
Iglesias SBDO, Leite HP, Meneses JFSE, De Carvalho WB (2007) Enteral nutrition in critically ill children: are prescription and delivery according to their energy requirements? Nutr Clin Pract 22:233–239. https://doi.org/10.1177/0115426507022002233
Ainsworth S, Furness J, Fenton A (2007) Randomized comparative trial between percutaneous longlines and peripheral cannulae in the delivery of neonatal parenteral nutrition. Acta Paediatr 90:1016–1020. https://doi.org/10.1111/j.1651-2227.2001.tb01357.x
Rico MP, Fernández Sarmiento J, Rojas Velasquez AM et al (2017) Regional citrate anticoagulation for continuous renal replacement therapy in children. Pediatr Nephrol 32:703–711. https://doi.org/10.1007/s00467-016-3544-9
Funding
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development [1R13HD104433-01].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vuong, K.T., Vega, M.R., Casey, L. et al. Clearance and nutrition in neonatal continuous kidney replacement therapy using the Carpediem™ system. Pediatr Nephrol 39, 1937–1950 (2024). https://doi.org/10.1007/s00467-023-06237-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06237-w