Abstract
Background
Rare autopsy studies have described smaller kidneys as well as urinary tract anomalies in Down syndrome. This observation has never been investigated in vivo and little is known about the possible consequences upon kidney function. Here we wish to confirm whether children with Down syndrome have smaller kidneys and to evaluate their kidney function in vivo.
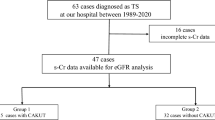
Methods
This retrospective cohort study enrolled 49 children with Down syndrome, as well as 49 age- and sex-matched controls at the Queen Fabiola Children’s University Hospital in Brussels, Belgium. Doppler and kidney ultrasonography, spot urine albumin to creatinine ratio, estimated glomerular filtration rate (eGFR), and anthropometric data were recorded.
Results
Kidney size in children with Down syndrome was smaller than age- and sex-matched controls in terms of length (p < 0.001) and volume (p < 0.001). Kidney function based on eGFR was also decreased in Down syndrome compared to historical normal. Twenty-one of the children with Down syndrome (42%) had eGFR < 90 mL/min/1.73 m2, with 5 of these (10%) having an eGFR < 75 mL/min/1.73 m2. In addition, 7 of the children with Down syndrome (14%) had anomalies of the kidney and/or urinary tract that had previously been undiagnosed.
Conclusions
Children with Down syndrome have significantly smaller kidneys than age-matched controls as well as evidence of decreased kidney function. These findings, in addition to well-noted increased kidney and urologic anomalies, highlight the need for universal anatomical and functional assessment of all individuals with Down syndrome.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
Data Availability
All data are available upon request.
Abbreviations
- eGFR:
-
Estimated glomerular filtration rate
- CKD:
-
Chronic kidney disease
- BSA:
-
Body surface area
- IDMS:
-
Isotope-dilution mass spectrometry
- PACS:
-
Picture archiving and communication system
- SD:
-
Standard deviation
References
Kallen B, Mastroiacovo P, Robert E (1996) Major congenital malformations in Down syndrome. Am J Med Gen 65:160–166
Cleves MA, Hobbs CA, Cleves PA, Tilford JM, Bird TM, Robbins JM (2007) Congenital defects among liveborn infants with Down syndrome. Birth Defects Res A Clin Mol Teratol 79:657–663
Kupferman JC, Druschel CM, Kupchik GS (2009) Increased prevalence of renal and urinary tract anomalies in children with Down syndrome. Pediatrics 124:e615–e621
Malaga S, Pardo R, Malaga I, Orejas G, Fernandez-Toral J (2005) Renal involvement in Down syndrome. Pediatr Nephrol 20:614–617
Kitamura A, Kondoh T, Noguchi M, Hatada T, Tohbu S, Mori KI, Matsuo M, Kunitsugu I, Kanetake H, Moriuchi H (2014) Assessment of lower urinary tract function in children with Down syndrome. Pediatr Int 56:902–908
Jain M, Singh A, Mantan M, Kapoor S (2014) Evaluation of structural anomalies of kidney and urinary tract in children with Down syndrome. Indian J Pediatr 81:734
Niamien-Attai C, Bacchetta J, Ranchin B, Sanlaville D, Cochat P (2017) Renal abnormalities in Down syndrome: a review. Arch Pediatr 24:1013–1018
Jaeger EA (1980) Ocular findings in Down’s syndrome. Trans Am Ophthalmolo Soc 78:808–845
da Cunha RP, Moreira JB (1996) Ocular findings in Down’s syndrome. Am J Ophthalmol 122:236–244
Postolache L (2019) Abnormalities of the optic nerve in Down syndrome and associations with visual acuity. Front Neurol 10:633
Woodhouse JM, Meades JS, Leat SJ, Saunders KJ (1993) Reduced accommodation in children with Down syndrome. Invest Ophthalmol Vis Sci 34:2382–2387
Parsa CF, Almer Z (2008) Supranumerary optic disc vessels may indicate reduced systemic angiogenesis in Down syndrome. Br J Ophthalmol 92:432–433
Postolache L, Parsa CF (2018) Brushfield spots and Wölfflin nodules unveiled in dark irides using near-infrared light. Sci Rep 8:18040
Parsa CF, Silva ED, Sundin OH, Goldberg MF, De Jong MR, Sunness JS, Zeimer R, Hunter DG (2001) Redefining papillorenal syndrome: an underdiagnosed cause of ocular and renal morbidity. Ophthalmology 108:738–749
Parsa CF (2008) Of Pax2 laboratory mice and human papillorenal investigations: maintaining the distinctions between cause and effect. J AAPOS 12:113–114
Parsa CF, Parsa A (2008) Diagnosing papillorenal syndrome: see the optic papilla. Pediatr Nephrol 23:1893–1894
Ariel I, Wells TR, Landing BH, Singer DB (1991) The urinary system in Down syndrome: a study of 124 autopsy cases. Pediatr Pathol 11:879–888
Naeye RL (1967) Prenatal organ and cellular growth with various chromosomal disorders. Biol Neonat 11:248–260
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317:1098
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Jaffe M (1886) Über den Niederschlag, welchen Pikrinsäure in normalen Harn erzeugt und über eine neue Reaktion des Kreatinins. Z Physiol Chem 10
Varley H, Gowenlock AH, Bell M (1980) Practical clinical biochemistry, 5th edn. William Heinemann Medical Books, London
Ezeofor SN, Anyanwu GE, Obikili EN (2020) Reference indices for evaluating kidney dimensions in children using anthropometric measurements. SA J Radiol 24:1882
Stoll C, Dott B, Alembik Y, Roth MP (2015) Associated congenital anomalies among cases with Down syndrome. Eur J Med Genet 58:674–680
Ahmed S (1990) Vesico-ureteric reflux in Down’s syndrome: poor prognosis. Aust N Z J Surg 60:113–116
Hicks JA, Carson C, Malone PS (2007) Is there an association between functional bladder outlet obstruction and Down’s syndrome? J Pediatr Urol 3:369–374
Chicoine B, Sulo S (2015) Rate of urinary retention in adults with Down syndrome: a prospective study. J Am Board Fam Med 28:115–117
Pottel H, Hoste L, Delanaye P (2015) Abnormal glomerular filtration rate in children, adolescents and young adults starts below 75 mL/min/1.73 m(2). Pediatr Nephrol 30:821–828
Yamakawa S, Nagai T, Uemura O (2018) Down syndrome and mild kidney dysfunction. Pediatr Int 60:391–393
Coburn SP, Seidenberg M, Mertz ET (1967) Clearance of uric acid, urea, and creatinine in Down’s syndrome. J Appl Physiol 23:579–580
Nishida Y, Akaoka I, Kobayashi M, Maruki K, Oshima Y (1979) Renal impairment in urate excretion in patients with Down’s syndrome. J Rheumatol 6:103–107
Zorick TS, Mustacchi Z, Bando SY, Zatz M, Moreira-Filho CA, Olsen B, Passos-Bueno MR (2001) High serum endostatin levels in Down syndrome: implications for improved treatment and prevention of solid tumours. Eur J Hum Genet 9:811–814
Ryeom S, Folkman J (2009) Role of endogenous angiogenesis inhibitors in Down syndrome. J Craniofac Surg 20:595–596
Baek KH, Zaslavsky A, Lynch RC, Britt C, Okada Y, Siarey RJ, Lensch MW, Park IH, Yoon SS, Minami T, Korenberg JR, Folkman J, Daley GQ, Aird WC, Galdzicki Z, Ryeom S (2009) Down’s syndrome suppression of tumour growth and the role of the calcineurin inhibitor DSCR1. Nature 459:1126–1130
Karihaloo A, Karumanchi SA, Cantley WL, Venkatesha S, Cantley LG, Kale S (2005) Vascular endothelial growth factor induces branching morphogenesis/tubulogenesis in renal epithelial cells in a neuropilin-dependent fashion. Mol Cell Biol 25:7441–7448
Marlier A, Schmidt-Ott KM, Gallagher AR, Barasch J, Karihaloo A (2009) Vegf as an epithelial cell morphogen modulates branching morphogenesis of embryonic kidney by directly acting on the ureteric bud. Mech Dev 126:91–98
Schwentner C, Oswald J, Lunacek A, Schlenck B, Berger AP, Deibl M, Fritsch H, Bartsch G, Radmayr C (2006) Structural changes of the intravesical ureter in children with vesicoureteral reflux-does ischemia have a role? J Urol 176:2212–2218
Murer L, Benetti E, Artifoni L (2007) Embryology and genetics of primary vesico-ureteric reflux and associated renal dysplasia. Pediatr Nephrol 22:788–797
Desogus M, Crobe A, Fraschini M, Ottonello G, Puddu M, Faa G, Fanos V (2016) Morphological changes in the kidney of fetuses with Down syndrome. J Pediatr Neonat Ind Med 5:e050125
Lo A, Brown HG, Fivush BA, Neu AM, Racusen LC (1998) Renal disease in Down syndrome: autopsy study with emphasis on glomerular lesions. Am J Kidney Dis 31:329–335
Smith DS (2001) Health care management of adults with Down syndrome. Am Fam Physician 64:1031–1038
American Academy of Pediatrics.Committee on Genetics (2001) Health supervision for children with Down syndrome. Pediatrics 107:442-449
Kute VB, Vanikar AV, Shah PR, Gumber MR, Patel HV, Engineer DP, Thakkar UG, Trivedi HL (2013) Down syndrome with end-stage renal disease. Indian J Clin Biochem 28:429–432
Jafar TH, Schmid CH, Landa M, Giatras I, Toto R, Remuzzi G, Maschio G, Brenner BM, Kamper A, Zucchelli P, Becker G, Himmelmann A, Bannister K, Landais P, Shahinfar S, de Jong PE, de Zeeuw D, Lau J, Levey AS (2001) Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Intern Med 135:73–87
Wuhl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, Zurowska A, Testa S, Jankauskiene A, Emre S, Caldas-Afonso A, Anarat A, Niaudet P, Mir S, Bakkaloglu A, Enke B, Montini G, Wingen AM, Sallay P, Jeck N, Berg U, Caliskan S, Wygoda S, Hohbach-Hohenfellner K, Dusek J, Urasinski T, Arbeiter K, Neuhaus T, Gellermann J, Drozdz D, Fischbach M, Moller K, Wigger M, Peruzzi L, Mehls O, Schaefer F (2009) Strict blood-pressure control and progression of renal failure in children. N Engl J Med 361:1639–1650
Simeoni M, Armeni A, Summaria C, Cerantonio A, Fuiano G (2017) Current evidence on the use of anti-RAAS agents in congenital or acquired solitary kidney. Ren Fail 39:660–670
Schwartz GJ, Dana F (2009) Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol 4:1832–1843
Du L, Zukotynski K, Hsiao E, Zurakowski D, Treves ST, Grant F (2009) Pediatric reference ranges for glomerular filtration rate determined by a single injection of Tc-99m DTPA. J Nucl Med 50:1375
Uemura O, Nagai T, Ishikura Ito S, Hataya H, Gotoh Y, Fujita N, Akioka Y, Kaneko T, Honda M (2015) Reference glomerular filtration rate levels in Japanese children: using the creatinine and cystatin C based estimated glomerular filtration rate. Clin Exp Nephrol 19:683–687
Leion F, Hegbrant J, den Bakker E, Jonsson M, Abrahamson M, Nyman U, Björk J, Lindström V, Larsson A, Bökenkamp A, Grubb A (2017) Estimating glomerular filtration rate (GFR) in children. The average between a cystatin C- and a creatinine-based equation improves estimation of GFR in both children and adults and enables diagnosing Shrunken Pore Syndrome. Scand J Clin Lab Invest 77:338–344
Regnault N, Kleinman KP, Rifas-Shiman SL, Langenberg C, Lipshultz SE, Gillman MW (2014) Components of height and blood pressure in childhood. Int J Epidemiol 43:149–159
Ramoshaba NE, Monyeki KD, Mpya J, Monyeki MS (2018) The relationship between sitting height, sitting height to height ratio with blood pressure among Polokwane private school children aged 6–13 years. BMC Public Health 17:973
Jaswal S, Jaswal IJ (1981) An anthropometric study of body size in Down syndrome. Indian J Pediatr 48:81–84
Costa L, Freire F, Bertapelli F, Campos LF, Santos LGTF, Gorla J (2013) Body proportions in children and adolescents with Down’s syndrome. J Hum Growth Dev 23:198–202
Nishino T, Endo S, Miyano H, Umeda C, Tomii Y, Watanabe Y, Nakagawa M, Kakegawa D, Fujinaga S (2021) Is the estimated glomerular filtration rate formula useful for evaluating the renal function of Down syndrome? Pediatr Int 63:944–950
González-Agüero A, Ara I, Moreno LA, Vicente-Rodríguez G, Casajús JA (2011) Fat and lean masses in youths with Down syndrome: gender differences. Res Dev Disabil 32:1685–1693
Lee SC, Lim LM, Chang EE, Chiu YW, Hwang SJ, Chen HC (2019) Effect of differences in serum creatinine estimation methodologies on estimated glomerular filtration rate. Singapore Med J 60:468–473
Acknowledgements
The authors thank Olof H. Sundin, PhD, for suggestions regarding selection criteria for the control group, as well as Mrs. Laurence Seidel for her assistance with some of the statistical analyses.
Funding
This work was supported by The Belgian Kids’ Fund for Pediatric Research of the Queen Fabiola Children’s University Hospital and by the Department of Ophthalmology, Erasmus Hospital, Université Libre de Bruxelles, Brussels, Belgium. The funders had no role in the design and conduct of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Approval for this study was obtained from the Institutional Review Boards and Institutional Ethics Committees of both the Queen Fabiola Children’s University Hospital (CEH 69/17) and the Erasmus Hospital (P2017/391; B4062017329655). All examinations were performed in accordance with the principles and tenets of the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained for all subjects with both parents providing consent.
Consent for publication
NA
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Postolache, L., Parsa, A., Simoni, P. et al. Widespread kidney anomalies in children with Down syndrome. Pediatr Nephrol 37, 2361–2368 (2022). https://doi.org/10.1007/s00467-022-05455-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05455-y