Abstract
Background
Long-term steroid treatment in children is known to cause obesity and negatively affect growth. The objective of this study was to determine the prevalence of obesity and overweight and analyze linear growth in children with nephrotic syndrome.
Methods
The study involved 265 children treated with glucocorticoids for nephrotic syndrome for a mean duration of 43 months (range: 6–167, IQR: 17, 63.3). Height, weight, and BMI SDS were recorded at each visit. Rate of change between the final and initial height, weight, and BMI was calculated (Δ score). The cumulative steroid dose (mg/kg/day) during follow-up was calculated. Relapses without significant edema were treated with low-dose steroids and steroid-sparing drugs were used in children with steroid dependency/frequent relapses.
Results
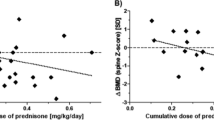
Mean first BMI SDS was + 1.40 ± 1.30 and final + 0.79 ± 1.30. At initial assessment, 41.4% of the patients were obese (BMI ≥ 95th percentile) and 19.5% were overweight (BMI 85th–95th percentile). At the last clinical visit, 24% were obese and 17% overweight. The children had lower BMI SDS at last clinical visit compared to initial assessment. Mean first height SDS of the cohort was − 0.11 ± 1.22 and final score 0.078 ± 1.14 (p < 0.0001). Almost 85% of patients were treated with steroid-sparing drugs.
Conclusions
Our results indicate that children with nephrotic syndrome, despite a need for steroid treatment for active disease, can improve their obesity and overweight and also improve their linear growth from their first to last visit with us.
Graphical abstract




Similar content being viewed by others
References
Chanchlani R, Parekh RS (2016) Ethnic differences in childhood nephrotic syndrome. Front Pediatr 4:39. https://doi.org/10.3389/fped.2016.00039
Hahn D, Hodson EM, Willis NS, Craig JC (2015) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev 18:CD001533. https://doi.org/10.1002/14651858.CD001533.pub5
Sinha A, Hari P, Sharma PK, Gulati A et al (2012) Disease course in steroid sensitive nephrotic syndrome. Indian Pediatr 49:881–887. https://doi.org/10.1007/s13312-012-0220-4
Rüth EM, Kemper MJ, Leumann EP, Laube GF et al (2005) Children with steroid-sensitive nephrotic syndrome come of age: long term outcome. J Pediatr 147:202–207. https://doi.org/10.1016/j.jpeds.2005.03.050
Skrzypczk P, Panczyk-Tomaszewska M, Roskowska-Blaim M, Wawer Z et al (2014) Long-term outcomes in idiopathic nephrotic syndrome: from childhood to adulthood. Clin Nephrol 81:166–173. https://doi.org/10.5414/CN108044
Ishikura K, Yoshikawa N, Nakazato H, Sasaki S, Nakanishi K, Matsuyama T, Ito S, Hamasaki Y, Yata N, Ando T, Iijima K, Honda M, Japanese Study Group of Renal Disease in Children (2015) Morbidity in children with frequently relapsing nephrosis: 10-year follow-up of a randomized controlled trial. Pediatr Nephrol 30:459–468. https://doi.org/10.1007/s00467-014-2955-8
Larkins N, Kim S, Craig J, Hodson E (2016) Steroid-sensitive nephrotic syndrome: an evidence-based update of immunosuppressive treatment in children. Arch Dis Child 101:404–408. https://doi.org/10.1136/archdischild-2015-308924
Chan EY, Tullus K (2021) Rituximab in children with steroid sensitive nephrotic syndrome: in quest of the optimal regimen. Pediatr Nephrol 36:1397–1405. https://doi.org/10.1007/s00467-020-04609-0
Azib S, Macher MA, Kwon T, Dechatres A et al (2011) Cyclophosphamide in steroid dependant nephrotic syndrome. Pediatr Nephrol 26:927–932. https://doi.org/10.1007/s00467-011-1830-0
Gruppen MP, Bouts AH, Jansen-van der Weide MC, Merkus MP et al (2018) A randomized clinical trial indicates that levamisole increases the time to relaps in children with steroid-sensitive nephrotic syndrome. Kidney Int 93:510–518. https://doi.org/10.1016/j.kint.2017.08.011
Boudin V, Alberti C, Lepayraque AL, Bensman A et al (2012) Mycophenolate mofetil for steroid-dependant nephrotic syndrome: a phase II Bayesian trial. Pediatr Nephrol 389-396https://doi.org/10.1007/s00467-011-2006-7
Raya K, Parikh A, Webb H, Hothi D (2017) Use of a low-dose prednisolone regimen to treat a relapse of steroid-sensitive nephrotic syndrome in children. Pediatr Nephrol 32:99–105. https://doi.org/10.1007/s00467-016-3458-6
Korsgaard T, Andersen RF, Joshi S, Hagstrom S et al (2019) Childhood onset steroid sensitive nephrotic syndrome continues into adulthood. Pediatr Nephrol 34:641–648. https://doi.org/10.1007/s00467-018-4119-8
Foster BJ, Shults J, Zemel BS, Leonard MB (2006) Risk factors for glucocorticoid-induced obesity in children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol 21:973–980. https://doi.org/10.1007/s00467-006-0100-z
Merritt RJ, Hack SL, Kalsch M, Olson D (1986) Corticosteroid therapy-induced obesity in children. Clin Pediatr 25:149–152. https://doi.org/10.1177/000992288602500304
WHO Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization. https://www.who.int/publications/i/item/924154693X. Accessed 11 November 2006
Simmonds J, Grundy N, Trompeter R, Tullus K (2010) Long-term steroid treatment and growth: a study in steroid-dependant nephrotic syndrome. Arch Dis Child 95:146–149. https://doi.org/10.1136/adc.2007.129957
Emma F, Sesto A, Rizzoni G (2003) Long term growth of children with severe steroid-responsive nephrotic syndrome. Pediatr Nephrol 18:783–788. https://doi.org/10.1007/s00467-003-1176-3
Deschenes G, Dossier C, Hogan J (2019) Treating the idiopathic nephrotic syndrome: are steroids the answer? Pediatr Nephrol 34:777–785. https://doi.org/10.1007/s00467-018-3963-x
Feld SM, Hirschberg R (1996) Insulin-like growth factor-I and insulin-like growth factor-binding proteins in the nephrotic syndrome. Pediatr Nephrol 10:355–358. https://doi.org/10.1007/BF00866783
Leonard MB, Feldman H, Shults J, Zemel BS et al (2004) Long-term, high-dose glucocorticoids and bone mineral content in childhood glucocorticoid sensitive nephrotic syndrome. N Eng J Med 351:868–875. https://doi.org/10.1056/nejmoa040367
Motoyama O, Itaka K (2007) Final height in children with steroid-sensitive nephrotic syndrome. Pediatr Int 49:623–625. https://doi.org/10.1111/j.1442-200x.2007.02429.x
Rüth EM, Kemper MJ, Leumann EP, Laube GF et al (2005) Children with steroid-sensitive nephroic syndrome come of age: long-term outcome. J Pediatr 147:202–207. https://doi.org/10.1016/j.jpeds.2005.03.050
Donatti LT, Koch VH (2009) Final height of adults with childhood-onset steroid-responsive idiopathic nephrotic syndrome. Pediatr Nephrol 24:2401–2408. https://doi.org/10.1007/s00467-009-1301-z
Valavi E, Aminzadeh M, Amouri P, Rezazadeh A et al (2018) Effecs of prednisolone on linear growth in children with nephrotic syndrome. J Pediatr 96:117–124. https://doi.org/10.1016/j.jped.2018.07.014
Gafni RI, Baron J (2000) Catch-up growth: possible mechanisms. Pediatr Nephrol 14:616–619. https://doi.org/10.1007/s004670000338
Berns JS, Gaudio KM, Krassner LS, Anderson FP et al (1987) Steroid-responsive nephrotic syndrome of childhood: a long-term study of clinical course, histopathology, efficacy of cyclophosphamide therapy, and effects on growth. Am J Kidney Dis 9:108–114
Padilla R, Brem AS (1989) Linear growth of children with nephrotic syndrome: effect of alkylating agents. Pediatrics 84:495–499
Radhakrishnan J, Cattran DC (2012) The KDIGO practice guideline on glomerulonephritis: reading between the (guide)lines–application to the individual patient. Kidney Int 82:840–856. https://doi.org/10.1038/ki.2012.280
Ribeiro D, Zawadaynski S, Pittet LF, Chevalley T et al (2015) Effect of glucocorticoids on growth and bone mineral density in children with nephrotic syndrome. Eur J Pediatr 174:911–917
Sato M, Ito S, Ogura M, Kamei K (2014) Impact of rituximab on height and weight in children with refractory steroid-dependant nephrotic syndrome. Pediatr Nephrol 29:1373–1379. https://doi.org/10.1007/s00467-014-2792-9
Elzouki AY, Jaiswal OP (1988) Long-term, small dose prednisone therapy in frequently relapsing nephrotic syndrome of childhood. Effect on remission, statural growth, obesity and infection rate. Clin Pediatr (Phila) 27:387–392. https://doi.org/10.1177/000992288802700807
Fakhouri F, Bocquet N, Taupin P, Presne C et al (2003) Steroid-sensitive nephrotic syndrome: from childhood to adulthood. Am J Kidney Dis 41:550–557. https://doi.org/10.1053/ajkd.2003.50116
Scharer K, Essigman HC, Schaefer F (1999) Body growth of children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 13:829–834. https://doi.org/10.1007/s004670050709
Hahn D, Hodson EM, Willis NS, Craig JC (2015) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev 2015:CD001533. https://doi.org/10.1002/14651858.CD001533.pub5
Sinha A, Saha A, Kumar M, Sharma S et al (2015) Extending initial prednisolone treatment in a randomized control trial from 3 to 6 months did not significantly influence the course of illness in children with steroid sensitive nephrotic syndrome. Kidney Int 87:217–224. https://doi.org/10.1038/ki.2014.240
Webb NJ, Woolley RL, Lambe T, Frew W et al (2019) Sixteen-week versus standard eight-week prednisolone therapy for childhood nephrotic syndrome: the Prednos RCT. Health Technol Assess 23:1–108. https://doi.org/10.3310/hta23260
Acknowledgements
We thank the Turkish Society of Nephrology for funding a research travel grant to Dr. Nilüfer Göknar for travel to the UK, and Prof. Dr. Türkay Sarıtaş for assistance with the statistics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study complied with the Declaration of Helsinki and was approved by the institutional audit review committee of Great Ormond Street Children’s Hospital.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Göknar, N., Webb, H., Waters, A. et al. Long-term obesity prevalence and linear growth in children with idiopathic nephrotic syndrome: is normal growth and weight control possible with steroid-sparing drugs and low-dose steroids for relapses?. Pediatr Nephrol 37, 1575–1584 (2022). https://doi.org/10.1007/s00467-021-05288-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05288-1