Abstract
Background
Dialysis in children as well as adults is prescribed to achieve a target spKt/Vurea, where Vurea is the volume of distribution of urea. Waste solute production may however be more closely correlated with body surface area (BSA) than Vurea which rises in proportion with body weight. Plasma levels of waste solutes may thus be higher in smaller patients when targeting spKt/Vurea since they have higher BSA relative to body weight. This study measured levels of pseudouridine (PU), a novel marker solute whose production is closely proportional to BSA, to test whether prescription of dialysis to a target spKt/Vurea results in higher plasma levels of PU in smaller children.
Methods
PU and urea nitrogen (ureaN) were measured in plasma and dialysate at the midweek hemodialysis session in 20 pediatric patients, with BSA ranging from 0.65–1.87m2. Mathematical modeling was employed to estimate solute production rates and average plasma solute levels.
Results
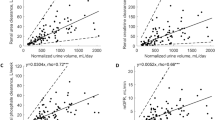
The dialytic clearance (Kd) of PU was proportional to that of ureaN (average KdPU/KdUreaN 0.69 ± 0.13, r2 0.84, p < 0.001). Production of PU rose in proportion with BSA (r2 0.57, p < 0.001). The pretreatment plasma level of PU was significantly higher in smaller children (r2 0.20, p = 0.051) while the pretreatment level of ureaN did not vary with size.
Conclusions
Prescribing dialysis based on urea kinetics may leave uremic solutes at higher levels in small children. Measurement of a solute produced proportional to BSA may provide a better index of dialysis adequacy than measurement of urea.




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
References
Kaur A, Davenport A (2014) Hemodialysis for infants, children, and adolescents. Hemodial Int 18:573–582
Warady BA, Neu AM, Schaefer F (2014) Optimal care of the infant, child, and adolescent on dialysis: 2014 update. Am J Kidney Dis 64:128–142
Daugirdas JT, Depner TA, Inrig J, et al (2015) KDOQI Clinical Practice Guideline for Hemodialysis Adequacy: 2015 Update. Am J Kidney Dis 66:884–930
Gotch FA, Sargent JA (1985) A mechanistic analysis of the National Cooperative Dialysis Study (NCDS). Kidney Int 28:526–534
Meyer TW, Sirich TL, Hostetter TH (2011) Dialysis cannot be dosed. Semin Dial 24:471–479
Rees L (2019) Assessment of dialysis adequacy: beyond urea kinetic measurements. Pediatr Nephrol 34:61–69
Vanholder R, Biesen WV, Lameire N (2019) A swan song for Kt/V urea. Seminars in Dialysis 32:424–437
Lowrie EG, Li Z, Ofsthun N, Lazarus JM (2005) The online measurement of hemodialysis dose (Kt): clinical outcome as a function of body surface area. Kidney Int 68:1344–1354
Morton AR, Singer MA (2007) The problem with Kt/V: dialysis dose should be normalized to metabolic rate not volume. Semin Dial 20:12–15
Daugirdas JT, Levin NW, Kotanko P, Depner TA, Kuhlmann MK, Chertow GM, Rocco MV (2008) Comparison of proposed alternative methods for rescaling dialysis dose: resting energy expenditure, high metabolic rate organ mass, liver size, and body surface area. Semin Dial 21:377–384
Daugirdas JT, Hanna MG, Becker-Cohen R, Langman CB (2010) Dose of dialysis based on body surface area is markedly less in younger children than in older adolescents. Clin J Am Soc Nephrol 5:821–827
Vanholder R, Schepers E, Pletinck A, Nagler EV, Glorieux G (2014) The uremic toxicity of indoxyl sulfate and p-cresyl sulfate: a systematic review. J Am Soc Nephrol 25:1897–1907
Meyer TW, Sirich TL, Fong KD, Plummer NS, Shafi T, Hwang S, Banerjee T, Zhu Y, Powe NR, Hai X, Hostetter TH (2016) Kt/Vurea and nonurea small solute levels in the hemodialysis study. J Am Soc Nephrol 27:3469–3478
Topp H, Armbrust S, Lengger C, Schoch G, Davies J, Stichler W, Manz F, Fusch C (2002) Renal excretion of 8-oxo-7,8-dihydro-2(')-deoxyguanosine: degradation rates of RNA and metabolic rate in humans. Arch Biochem Biophys 402:31–37
Dzurik R, Lajdova I, Spustova V, Opatrny K Jr (1992) Pseudouridine excretion in healthy subjects and its accumulation in renal failure. Nephron 61:64–67
Dlugajczyk A, Eiler JJ (1966) Lack of catabolism of 5-ribosyluracil in man. Nature 212:611–612
Sirich TL, Funk BA, Plummer NS, Hostetter TH, Meyer TW (2014) Prominent accumulation in hemodialysis patients of solutes normally cleared by tubular secretion. J Am Soc Nephrol 25:615–622
Daugirdas JT, Depner TA, Greene T, Silisteanu P (2009) Solute-solver: a web-based tool for modeling urea kinetics for a broad range of hemodialysis schedules in multiple patients. Am J Kidney Dis 54:798–809
Gehan EA, George SL (1970) Estimation of human body surface area from height and weight. Cancer Chemother Rep 54:225–235
Daniewska-Michalska D, Motyl T, Gellert R, Kukulska W, Podgurniak M, Opechowska-Pacocha E, Ostrowski K (1993) Efficiency of hemodialysis of pyrimidine compounds in patients with chronic renal failure. Nephron 64:193–197
Sirich TL, Plummer NS, Gardner CD, Hostetter TH, Meyer TW (2014) Effect of increasing dietary fiber on plasma levels of colon-derived solutes in hemodialysis patients. Clin J Am Soc Nephrol 9:1603–1610
Sirich TL, Meyer TW (2018) Intensive hemodialysis fails to reduce plasma levels of uremic solutes. Clin J Am Soc Nephrol 13:361–362
Johnson WJ, Hagge WW, Wagoner RD, Dinapoli RP, Rosevear JW (1972) Effects of urea loading in patients with far-advanced renal failure. Mayo Clin Proc 47:21–29
Depner TA (2001) Uremic toxicity: urea and beyond. Semin Dial 14:246–251
Daugirdas JT, Depner TA, Greene T, Kuhlmann MK, Levin NW, Chertow GM, Rocco MV (2008) Surface-area-normalized Kt/V: a method of rescaling dialysis dose to body surface area-implications for different-size patients by gender. Semin Dial 21:415–421
Depner TA (2003) Prescribing hemodialysis: the role of gender. Adv Ren Replace Ther 10:71–77
Depner T, Daugirdas J, Greene T, Allon M, Beck G, Chumlea C, Delmez J, Gotch F, Kusek J, Levin N, Macon E, Milford E, Owen W, Star R, Toto R, Eknoyan G (2004) Dialysis dose and the effect of gender and body size on outcome in the HEMO study. Kidney Int 65:1386–1394
Eloot S, Van Biesen W, Roels S, Delrue W, Schepers E, Dhondt A, Vanholder R, Glorieux G (2017) Spontaneous variability of pre-dialysis concentrations of uremic toxins over time in stable hemodialysis patients. PLoS One 12:e0186010
Rintala-Dempsey AC, Kothe U (2017) Eukaryotic stand-alone pseudouridine synthases – RNA modifying enzymes and emerging regulators of gene expression? RNA Biology 14:1185–1196
Song J, Yi C (2017) Chemical modifications to RNA: a new layer of gene expression regulation. ACS Chem Biol 12:316–325
Pane F, Oriani G, Kuo KC, Gehrke CW, Salvatore F, Sacchetti L (1992) Reference intervals for eight modified nucleosides in serum in a healthy population from Italy and the United States. Clin Chem 38:671–677
Topp H, Unverzagt S, Rudloff S, Schoch G, Manz F, Fusch C (2003) Diurnal variation in the renal excretion of modified RNA catabolites in humans. Clin Sci 105:195–202
Topp H, Fusch G, Schoch G, Fusch C (2008) Noninvasive markers of oxidative DNA stress, RNA degradation and protein degradation are differentially correlated with resting metabolic rate and energy intake in children and adolescents. Pediatr Res 64:246–250
Struijk DG, Schoots AC, Koole LH, van der Reijden HJ, Koomen GC, Krediet RT, Arisz L (1991) Transport kinetics of pseudouridine during hemodialysis and continuous ambulatory peritoneal dialysis. J Lab Clin Med 118:74–80
Vanholder RC, De Smet RV, Ringoir SM (1992) Assessment of urea and other uremic markers for quantification of dialysis efficacy. Clin Chem 38:1429–1436
Snauwaert E, Van Biesen W, Raes A, Glorieux G, Vanholder R, Vande Walle J, Eloot S (2018) A plea for more uremic toxin research in children with chronic kidney disease. Pediatr Nephrol 33:921–924
Snauwaert E, Holvoet E, Van Biesen W, Raes A, Glorieux G, Vande Walle J, Roels S, Vanholder R, Askiti V, Azukaitis K, Bayazit A, Canpolat N, Fischbach M, Godefroid N, Krid S, Litwin M, Obrycki L, Paglialonga F, Ranchin B, Samaille C, Schaefer F, Schmitt CP, Spasojevic B, Stefanidis CJ, Van Dyck M, Van Hoeck K, Collard L, Eloot S, Shroff R (2019) Uremic toxin concentrations are related to residual kidney function in the pediatric hemodialysis population. Toxins (Basel) 11(4). https://doi.org/10.3390/toxins11040235
Snauwaert E, Van Biesen W, Raes A, Glorieux G, Vande Walle J, Roels S, Vanholder R, Askiti V, Azukaitis K, Bayazit A, Canpolat N, Fischbach M, Saoussen K, Litwin M, Obrycki L, Paglialonga F, Ranchin B, Samaille C, Schaefer F, Schmitt CP, Spasojevic B, Stefanidis CJ, Shroff R, Eloot S (2019) Haemodiafiltration does not lower protein-bound uraemic toxin levels compared with haemodialysis in a paediatric population. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfz132
Shroff R, Bayazit A, Stefanidis CJ, Askiti V, Azukaitis K, Canpolat N, Agbas A, Anarat A, Aoun B, Bakkaloglu S, Bhowruth D, Borzych-Duzalka D, Bulut IK, Buscher R, Dempster C, Duzova A, Habbig S, Hayes W, Hegde S, Krid S, Licht C, Litwin M, Mayes M, Mir S, Nemec R, Obrycki L, Paglialonga F, Picca S, Ranchin B, Samaille C, Shenoy M, Sinha M, Smith C, Spasojevic B, Vidal E, Vondrak K, Yilmaz A, Zaloszyc A, Fischbach M, Schaefer F, Schmitt CP (2018) Effect of haemodiafiltration vs conventional haemodialysis on growth and cardiovascular outcomes in children - the HDF, heart and height (3H) study. BMC Nephrol 19:199
Shroff R, Smith C, Ranchin B, Bayazit AK, Stefanidis CJ, Askiti V, Azukaitis K, Canpolat N, Agbas A, Aitkenhead H, Anarat A, Aoun B, Aofolaju D, Bakkaloglu SA, Bhowruth D, Borzych-Duzalka D, Bulut IK, Buscher R, Deanfield J, Dempster C, Duzova A, Habbig S, Hayes W, Hegde S, Krid S, Licht C, Litwin M, Mayes M, Mir S, Nemec R, Obrycki L, Paglialonga F, Picca S, Samaille C, Shenoy M, Sinha MD, Spasojevic B, Stronach L, Vidal E, Vondrak K, Yilmaz A, Zaloszyc A, Fischbach M, Schmitt CP, Schaefer F (2019) Effects of Hemodiafiltration versus conventional hemodialysis in children with ESKD: the HDF, heart and height study. J Am Soc Nephrol 30:678–691
Morgenstern BZ, Wuhl E, Nair KS, Warady BA, Schaefer F (2006) Anthropometric prediction of total body water in children who are on pediatric peritoneal dialysis. J Am Soc Nephrol 17:285–293
Acknowledgments
This work was supported by National Institutes of Health award R01 DK101674 to T.W.M. F.J.O’B. and L.L.G. were supported by fellowships from the Child Health Research Institute (CHRI) at Stanford. T.L.S. was supported by a Veterans Affairs Career Development Award (CX-001036-01A1). The authors thank the dialysis staffs of the Lucile Packard Children’s Hospital at Stanford and the UCSF Benioff Children’s Hospital for help with recruiting patients and collecting samples.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Institutional Review Boards of Stanford University and the University of California, San Francisco and was conducted in accordance with the Declaration of Helsinki. Consent was provided by subjects and/or their legally authorized representatives.
Conflict of interest
The authors have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 244 kb)
Rights and permissions
About this article
Cite this article
O’Brien, F.J., Sirich, T.L., Taussig, A. et al. Plasma pseudouridine levels reflect body size in children on hemodialysis. Pediatr Nephrol 35, 305–312 (2020). https://doi.org/10.1007/s00467-019-04369-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04369-6