Abstract
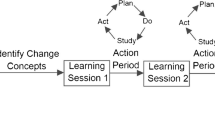
Improving quality of care delivery is an important focus for all practicing physicians. Frontline clinicians are in a great position to identify clinical problems and find innovative solutions. The current review describes the method used for quality improvement based on the Model for Improvement, a structural framework to guide improvement work. At its basis are three fundamental questions: What are we trying to accomplish? How will I know that a change will lead to improvement? And what changes could we make that will result in improvement? This preparation phase aims to identify and understand the problem, choose an intervention, and determine reliable measures to gauge improvement. The intervention is then tested using PLAN-DO-STUDY-ACT (PDSA) cycles, an iterative approach to systematically improve processes and outcomes. PLAN focuses on defining the goal of the cycle and describing in details what will be done. DO concentrates on the concrete application of the plan. STUDY focuses on data analyses as ACT identifies lessons learned from the cycle and orientate the goals of the following PDSA cycle. Learning from each cycle, developing an interdisciplinary team and repeated interventions are core principles involved in implementing a sustainable quality improvement program. The Model for Improvement will be illustrated by a common quality problem in pediatric nephrology.









Similar content being viewed by others
References
(2000) In: Kohn LT, Corrigan JM, Donaldson MS (eds) To err is human: building a safer health system, Washington (DC)
Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, Etchells E, Ghali WA, Hebert P, Majumdar SR, O'Beirne M, Palacios-Derflingher L, Reid RJ, Sheps S, Tamblyn R (2004) The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ 170:1678–1686
Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH (1991) Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard medical practice study I. N Engl J Med 324:370–376
Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD (1995) The quality in Australian health care study. Med J Aust 163:458–471
Vincent C, Neale G, Woloshynowych M (2001) Adverse events in British hospitals: preliminary retrospective record review. BMJ 322:517–519
Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, Howard KM, Weiler PC, Brennan TA (2000) Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care 38:261–271
Spencer E, Walshe K (2009) National quality improvement policies and strategies in European healthcare systems. Qual Saf Health Care 18(Suppl 1):i22–i27
Services USDoHaH (2011) National strategy for quality improvement in health care. In: Services USDoHaH (ed) p 27
Backman C, Vanderloo S, Forster AJ (2016) Measuring and improving quality in university hospitals in Canada: the collaborative for excellence in healthcare quality. Health Policy 120:982–986
Makary MA, Daniel M (2016) Medical error-the third leading cause of death in the US. BMJ 353:i2139
(2001) Crossing the Quality Chasm: A New Health System for the 21st Century, Washington (DC)
Berwick DM (1996) A primer on leading the improvement of systems. BMJ 312:619–622
Batalden PB, Davidoff F (2007) What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care 16:2–3
Ogrinc GSHL, Moore SM, Barton AJ, Dolansky MA, Madigosky WS (2012) In: Improvement IfH (ed) Fundamentals of health care improvement: a guide to improving your patient’s care. Joint Commission, Oak Brook Terrace
Provost LPMS (2011) The health care data guide: learning from data for improvement. Jossey-Bass, San Francisco
Neu AM (2012) Immunizations in children with chronic kidney disease. Pediatr Nephrol 27:1257–1263
Mitsnefes MM, Laskin BL, Dahhou M, Zhang X, Foster BJ (2013) Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990-2010. JAMA 309:1921–1929
Esposito S, Mastrolia MV, Prada E, Pietrasanta C, Principi N (2014) Vaccine administration in children with chronic kidney disease. Vaccine 32:6601–6606
Miyairi I, Funaki T, Saitoh A (2016) Immunization practices in solid organ transplant recipients. Vaccine 34:1958–1964
Chi C PP, Pilishvili T, Moore M, Murphy T, Strikas R (2012) Guidelines for vaccinating dialysis patients and chronic kidney disease patients—recommendations of the Advisory Committee on Immunization Practices (ACIP) https://www.cdc.gov/vaccines/pubs/downloads/dialysis-guide-2012.pdf. Accessed 26 Oct 2017
Collins AJ, Foley RN, Chavers B, Gilbertson D, Herzog C, Johansen K, Kasiske B, Kutner N, Liu J, St Peter W, Guo H, Gustafson S, Heubner B, Lamb K, Li S, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Thompson B, Wang C, Weinhandl E, Zaun D, Arko C, Chen SC, Daniels F, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L (2012) United States renal data system 2011 annual data report: atlas of chronic kidney disease & end-stage renal disease in the United States. Am J Kidney Dis 59(A7):e1–420
Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP (2009) The improvement guide: a practical approach to enhancing organizational performance. Jossey-Bass Pub, San Francisco
Silver SA, Harel Z, McQuillan R, Weizman AV, Thomas A, Chertow GM, Nesrallah G, Bell CM, Chan CT (2016) How to begin a quality improvement project. Clin J Am Soc Nephrol 11:893–900
Friedman AN, Fadem SZ (2011) Making measures count. Clin J Am Soc Nephrol 6:1507–1511
Moraros J, Lemstra M, Nwankwo C (2016) Lean interventions in healthcare: do they actually work? A systematic literature review. Int J Qual Health Care 28:150–165
Reed JE, Card AJ (2016) The problem with plan-do-study-act cycles. BMJ Qual Saf 25:147–152
Etchells E, Ho M, Shojania KG (2016) Value of small sample sizes in rapid-cycle quality improvement projects. BMJ Qual Saf 25:202–206
Baily MA, Bottrell M, Lynn J, Jennings B, Hastings C (2006) The ethics of using QI methods to improve health care quality and safety. Hast Cent Rep 36:S1–S40
Weller J, Boyd M, Cumin D (2014) Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J 90:149–154
Schiller C, Winters M, Hanson HM, Ashe MC (2013) A framework for stakeholder identification in concept mapping and health research: a novel process and its application to older adult mobility and the built environment. BMC Public Health 13:428
McQuillan RF, Silver SA, Harel Z, Weizman A, Thomas A, Bell C, Chertow GM, Chan CT, Nesrallah G (2016) How to measure and interpret quality improvement data. Clin J Am Soc Nephrol 11:908–914
Grol RP, Bosch MC, Hulscher ME, Eccles MP, Wensing M (2007) Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q 85:93–138
Varkey P, Reller MK, Resar RK (2007) Basics of quality improvement in health care. Mayo Clin Proc 82:735–739
Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE (2014) Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf 23:290–298
Perla RJ, Provost LP, Murray SK (2011) The run chart: a simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf 20:46–51
Birkinshaw J, Haas JB (2016) Increase your return on failure. Harv Bus Rev https://hbr.org/2016/05/increase-your-return-on-failure. Accessed 04 Jan 2018
Rubenstein LV, Hempel S, Farmer MM, Asch SM, Yano EM, Dougherty D, Shekelle PW (2008) Finding order in heterogeneity: types of quality-improvement intervention publications. Qual Saf Health Care 17:403–408
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D (2016) SQUIRE 2.0-standards for quality improvement reporting excellence-revised publication guidelines from a detailed consensus process. J Am Coll Surg 222:317–323
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D (2015) SQUIRE 2.0 (standards for quality improvement reporting excellence): revised publication guidelines from a detailed consensus process. Jt Comm J Qual Patient Saf 41:474–479
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Answers: 1b 2d 3e 4c 5d
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gaudreault-Tremblay, MM., McQuillan, R.F., Parekh, R.S. et al. Quality improvement in pediatric nephrology—a practical guide. Pediatr Nephrol 35, 199–211 (2020). https://doi.org/10.1007/s00467-018-4175-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4175-0