Abstract
Background
In primarily unresectable liver tumors, ALPPS (Associating Liver Partition and Portal Vein Ligation for Staged hepatectomy) may offer curative two-stage hepatectomy trough a fast and extensive hypertrophy. However, concerns have been raised about the invasiveness of the procedure. Full robotic ALPPS has the potential to reduce the postoperative morbidity trough a less invasive access. The aim of this study was to compare the perioperative outcomes of open and full robotic ALPPS.
Methods
The bicentric study included open ALPPS cases from the University Hospital Zurich, Switzerland and robotic ALPPS cases from the University of Modena and Reggio Emilia, Italy from 01/2015 to 07/2022. Main outcomes were intraoperative parameters and overall complications.
Results
Open and full robotic ALPPS were performed in 36 and 7 cases. Robotic ALPPS was associated with less blood loss after both stages (418 ± 237 ml vs. 319 ± 197 ml; P = 0.04 and 631 ± 354 ml vs. 258 ± 53 ml; P = 0.01) as well as a higher rate of interstage discharge (86% vs. 37%; P = 0.02). OT was longer with robotic ALPPS after both stages (371 ± 70 min vs. 449 ± 81 min; P = 0.01 and 282 ± 87 min vs. 373 ± 90 min; P = 0.02). After ALPPS stage 2, there was no difference for overall complications (86% vs. 86%; P = 1.00) and major complications (43% vs. 39%; P = 0.86). The total length of hospital stay was similar (23 ± 17 days vs. 26 ± 13; P = 0.56).
Conclusion
Robotic ALPPS was safely implemented and showed potential for improved perioperative outcomes compared to open ALPPS in an experienced robotic center. The robotic approach might bring the perioperative risk profile of ALPPS closer to interventional techniques of portal vein embolization/liver venous deprivation.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
The need of inducing future liver remnant (FLR) hypertrophy to prevent post-hepatectomy liver failure (PHLF) and adequate oncologic outcomes after liver resection is a key point in dealing with bilobar or large unilobar primary and secondary liver cancers [1,2,3]. The two-staged hepatectomy called ALPPS (Associating Liver Partition and Portal Vein Ligation for Staged hepatectomy) offers fast and extensive hypertrophy of the FLR after portal vein occlusion and in situ splitting of the liver in a first stage, followed by completion hepatectomy one or 2 weeks later [4, 5]. In patients with primarily unresectable liver tumors, ALPPS may offer curative surgery. Compared to PVE, the proposed advantages of ALPPS are a faster growth resulting in a higher resectability rate and therefore, preventing progression of cancer in the interstage interval.
However, despite initial enthusiasm, concerns have been raised about the invasiveness of the procedure represented by a severe morbidity of up to 60% and high mortality rates of 10–20% [6,7,8,9].
Recently, robotic liver surgery has gained wide acceptance in specialized hepato-biliary (HPB) centers due to its minimally invasive access with several intraoperative advantages such as enhanced 3D vision with stability and full control of the operative field by the console surgeon and instruments with seven degrees of freedom, which translates to a faster postoperative recovery and less postoperative morbidity. [10, 11] Yet, full robotic ALPPS is a highly demanding procedure that has only been reported in some case reports [12, 13]. The aim of the present bicentric study was to compare a case series of full robotic with open ALPPS in terms of short-term perioperative outcomes.
Methods
Study design
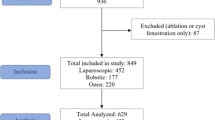
This retrospective bicentric study was conducted at two high-volume referral centers for HPB surgery between January 2015 and July 2022. Cases for open ALPPS were included from the University hospital Zurich, Switzerland and full robotic ALPPS cases were included from the HPB and liver transplant unit of the University of Modena and Reggio Emilia, Italy. Data were extracted from a prospectively maintained database, the international ALPPS registry. The ALPPS registry is maintained by the Department of Surgery, University of Zurich, Switzerland, approved by the Cantonal Ethics Committee of Zurich (KEK 2013–0326) and is registered at ClinicalTrials.gov (NCT01924741). All patients provided written informed consent. Included were consecutive adult patients with any indication for ALPPS after discussion of the clinical, laboratory and radiology investigations in a multidisciplinary tumor board. After 5 years of robotic HPB surgery and an initial experience of 123 cases of robotic liver resection, robotic ALPPS was started in 2019 (Fig. 1). Since robotic ALPPS was introduced, no more cases of open ALPPS were performed at the HPB and liver transplant unit of the University of Modena and Reggio Emilia. Tumor entity, tumor location, proximity to major vascular structures, and previous abdominal surgery were not considered an exclusion criterion for the robotic approach. Exclusion criteria for the robotic approach were anticipated major vascular resection and reconstruction.
Perioperative assessment
Preoperative and interstage volumetric assessment was done in collaboration with the radiology departments. All patients underwent preoperative volumetric analyses on the basis of the computed tomography (CT) scan or magnetic resonance imaging (MRI). Volume of the tumor lesions were excluded from the total liver volume (TLV). Estimated total liver volume (eTLV) was calculated using the Vauthey formula [14]. The two parameters used to evaluate necessity of inducing FLR hypertrophy were FLR/eTLV and FLR to body-weight ratio (BWR). After stage 1, FLR hypertrophy was routinely assessed after 5 and 10 days. If hypertrophy was inadequate re-assessment was done every 7–10 days. The aim was to reach at least a FLR/ eTLV of 30% in case of normal liver function tests. In cases of abnormal liver function tests, this threshold was elevated to 35%–40%. Completion of ALPPS stage 2 was always decided after multidisciplinary evaluation of FLR hypertrophy, liver function tests, and general status of the patient.
Outcome assessment
Primary outcome
The main outcome were major complications after both ALPPS stage 1 and 2 defined as grade 3 or higher according to the Clavien–Dindo classification [15].
Secondary outcomes
Secondary outcomes were operative time, estimated blood loss (EBL), liver growth rate, post-hepatectomy liver failure (PHLF) according to the International Study Group of Liver Surgery [16], postoperative complications classified according to the Clavien–Dindo classification [15], and the comprehensive complication index (CCI) [17]. The CCI represents an index to assess the cumulative postoperative morbidity. This novel metric measures the overall morbidity on a scale from 0.
(no complication) to 100 (death) [17, 18]. Furthermore, ALPPS completion rate, R0 resection rate, ICU, and hospital stay were assessed.
Surgical technique of robotic ALPPS (Supplementary video 1)
Stage 1
The robotic platforms used for the cases performed was the da Vinci Xi Surgical System (Intuitive Surgical Inc., Sunnyvale, California, United States). Patients were put in supine position, 10–15° anti-Trendelenburg, and 5–10° tilt left. Access to abdominal cavity was obtained through open laparoscopy on the left side of the umbilical scar, introducing the trocar of the AirSeal™ system. Four robotic, 8-mm trocars were placed from right to left hypochondria in a straight line, with a minimum of 8 cm distance in between. Pneumoperiotneum pressure was kept at 12 mmHg. An additional 12-mm trocar was introduced under vision in the right flank. Intraoperative ultrasound (IOUS) was used as needed to identify vascular structure and define relations between lesions and major vessels. After cholecystectomy, hilar dissection was performed until the right hepatic artery and portal vein were encircled with vessel loops.
Infrared visualization was used to enhance ICG fluorescence and visualize bile ducts. ICG was routinely administrated 12 h prior to the procedure with a dose of 0.25 mg/kg. Then the right portal vein was divided between hem-o-lok clips or with a stapling device. Liver transection was performed with the harmonic scalpel, bipolar and monopolar currents aiming for complete or near-complete division (Fig. 2A).
Hem-o-lok, titanium clips, ligatures, and sutures were used to achieve division of vasculo-biliary structures within the parenchyma and to obtain hemostasis and biliostasis. At the end of the transection a drain was usually left in between the cut surface.
Stage 2
After adequate hypertrophy (see above) stage 2 started using the same incisions as of the stage 1. Adhesiolysis was conducted. Full right mobilization was then performed. The right hepatic artery was divided between clips, then the hilar plate was divided, and both the right and middle hepatic vein were divided with a stapling device. If necessary, biliary reconstruction was performed (Fig. 2B). The specimen was extracted through a Pfannenstiel incision.
Statistics
Continuous variables were compared with Student’s t test and Mann–Whitne test as appropriate. Differences between proportions derived from categorical data were compared with chi-square or Fisher’s exact test. The software used is STATA 15.
Results
During the study period, 36 patients underwent open- and 7 full robotic ALPPS. Patients in the open group had a higher body mass index (27 ± 4 vs. 23 ± 4 kg/m2; P = 0.05) and open ALPPS was mainly performed for CRLM (89% vs. 29%), whereas robotic ALPPS was more often performed for cholangiocarcinoma (57% vs. 3%; P < 0.01). Other baseline characteristics such as age, sex, American Society of Anesthesiologists score, comorbidities, and model for end-stage liver disease score were similar. Before stage 1, both TLV (1655 ± 282 ml vs. 1398 ± 223 ml; P = 0.02) and FLR (495 ± 177 ml vs. 340 ± 99 ml; P = 0.03) were higher in the open ALPPS group, resulting in a higher FLR/eTLV (30 ± 10% vs. 25 ± 6%; P = 0.16). Preoperative functional liver test with ICG testing were comparable (Table 1).
Intraoperative outcomes
In both groups, most patients underwent right trisectionectomy (61% vs. 71%; P = 0.69). EBL after both stage 1 (418 ± 237 ml vs. 319 ± 197 ml; P = 0.04) and stage 2 (631 ± 354 ml vs. 258 ± 53 ml; P = 0.01) was less in the robotic ALPPS group. On the other hand, OT was longer in the robotic ALPPS group after both stage 1 (371 ± 70 min vs. 449 ± 81 min; P = 0.01) and stage 2 (282 ± 87 min vs. 373 ± 90 min; P = 0.02). Details are shown in Table 2.
Post-operative outcomes
After ALPPS stage 1, there was no difference for overall complications (50% vs. 57%; P = 1.00) as well as major complications (8% vs. 14%; P = 0.62). In line with those results, the cumulative postoperative morbidity assessed by the CCI after stage 1 was not different (12 ± 19 vs. 13 ± 15; P = 0.83). There was no difference in terms of occurrence of PHLF after stage 1. One fatality was recorded in the open group after ALPPS stage 1 due to sepsis and multi-organ failure in the setting of PHLF grade C.
There was a higher rate of interstage discharge in the robotic group (37% vs. 86%; P = 0.02). Both groups demonstrated adequate FLR increase (53 ± 39% vs. 82 ± 44%; P = 0.08) in a similar amount of time (24 days vs. 16 days; P = 0.66). Completion of the ALPPS procedure was possible in most cases (97% vs. 100%; P = 0.65).
Again, after ALPPS stage 2, there was no difference for overall complications (86% vs. 86%; P = 1.00) as well as major complications (39% vs. 43%; P = 0.86). The CCI after stage 2 was not different (30 ± 23 vs. 27 ± 12; P = 0.79). There was no difference in terms of PHLF after stage 2. After ALPPS stage 2, two casualties occurred in the open cohort, one due to PHLF grade C and the other due to intraoperative myocardial infarction immediately after laparotomy. There was no difference in R0 resection rate (91% vs. 100%; P = 0.72), total length of ICU stay (3 ± 2 days vs. 2 ± 2 days; P = 0.48) nor total length of hospital stay (26 ± 13 days vs. 23 ± 17 days; P = 0.56). Post-operative outcomes are reported in Table 3.
Discussion
This is the first study comparing a case series of full robotic with open ALPPS. The analysis shows that robotic ALPPS offers distinct advantages over the open approach, such as reduced blood loss during both ALPPS stages as well as a higher rate of interstage discharge. Even though little selection criteria were applied from the start of the robotic ALPPS program and the results therefore include the learning curve of an experienced robotic HPB center, the surgical morbidity and mortality were comparable for the robotic and open approach. Except for a longer operation time of the robotic approach, robotic ALPPS was associated with similar postoperative outcomes, while no conversion to an open approach was necessary.
Patient safety is of utmost importance when introducing a novel surgical approach. Both the similar major morbidity rate and a lower mortality rate in the robotic group (0% vs. 8%) demonstrate the safe implementation of the robotic ALPPS approach. Most important, no complications were directly attributable to the robotic approach. Of note, robotic ALPPS was implemented after an institutional robotic HPB learning period of 5 years with a previous institutional experience of 123 HPB procedures, including major robotic liver resections and living kidney donation, demonstrating the broad experience with robotic surgery before ALPPS [19].
In a large Italian registry study, open and laparoscopic ALPPS were compared and the minimally invasive approach decreased the overall complication rate after stage 1, lowered the PHLF rate, and was even associated with a reduced in-hospital mortality rate in multivariate analysis [20]. A similar or even more pronounced effect could be expected for the robotic ALPPS approach after surpassing the learning curve of around 20–60 cases for major liver resections [11, 21]. Both centers included in this study have not implemented laparoscopic ALPPS and therefore, a direct comparison to laparoscopic ALPPS is missing. However, due to an improved 3D vision with magnification of the operative field and enhanced versatility of the robotic instruments the robotic approach offers several potential benefits as already demonstrated in hepato-biliary surgery [22, 23].
While in the current study no cases had to be converted to an open approach, the main contributing factors for a significant conversion rate were adhesions and bleeding especially in the technically more challenging stage 2 (Stage 1: 4% and stage 2: 28%) [20]. The second stage of ALPPS, which typically includes an extensive adhesiolysis, followed by a right or extended right hemihepatectomy is technically much more complex. In the Italian registry study, after minimally invasive stage one, two-third of patients were operated with a laparoscopic approach showing the growing interest of surgeons in minimizing the operative trauma for the patient. Irrespective of the approach for stage 2, minimally invasive stage 1 decreased the overall surgical impact on patients as demonstrated by a lower overall complication rate and in line with this finding, a higher interstage discharge rate. In our own experience, patients requiring complex vasculo-biliary resections and reconstructions, therefore undergoing robotic ALPPS stage 1 with open stage 2, equally benefitted from the reduced surgical trauma as demonstrated by a low postoperative morbidity.
In the current study, the liver regeneration was not affected by the surgical approach. Both the open and robotic approach showed adequate liver hypertrophy and a similar PHLF rate. These findings are somehow contradictory to the two largest series of minimally invasive, laparoscopic ALPPS, where the minimally invasive approach was associated with significantly less clinically relevant PHLF in both studies [20, 24]. While the sample size of the current study does not allow a statistically sound comparison, it has to be kept in mind, that the FLR/eTLV rate was considerably lower in the robotic group before stage 1 (25% vs. 30%), a factor that might have mitigated beneficial effects of the robotic approach on PHLF rate.
The study is certainly limited by the sample size of the robotic group, limiting statistical comparisons. However, currently the literature consists of some single-case reports, therefore, this study represents the largest consecutive series of full robotic ALPPS. The limited application of the robotic ALPPS approach introduces potential bias with regard to patient selection and uncontrolled baseline differences of the groups. Confounders such as different ALPPS indications (CRLM vs. primary liver tumors) and differences in the FLR may have further affected the outcomes of this study. Furthermore, the cost of the two approaches was not directly compared. However, several studies on robotic hepato-pancreato-biliary surgery showed that the robotic instruments are more expensive. If patients experience less complications and therefore have a shorter hospital stay, the robotic approach is cost effective. [25,26,27] Given the higher rate of interstage discharge and a 3-day difference in length of stay, we assume cost effectiveness of the robotic approach even with the longer operation time in this cohort.
Conclusion
In a highly experienced robotic HPB center, full robotic ALPPS was safely implemented and showed potential for improved perioperative outcomes compared to open ALPPS including a higher rate of interstage discharge potentially a surrogate for a lower surgical trauma. The robotic approach might help to transform the ALPPS method into a less invasive technique, bringing its perioperative risk profile closer to the interventional techniques of portal vein embolization and liver venous deprivation while allowing for a fast and extensive FLR hypertrophy.
References
Müller PC, Linecker M, Kirimker EO, Oberkofler CE, Clavien P-A, Balci D et al (2021) Induction of liver hypertrophy for extended liver surgery and partial liver transplantation: state of the art of parenchyma augmentation–assisted liver surgery. Langenbecks Arch Surg 406:2201–2215. https://doi.org/10.1007/s00423-021-02148-2
Petrowsky H, Linecker M, Raptis DA, Kuemmerli C, Fritsch R, Kirimker OE et al (2020) first long-term oncologic results of the ALPPS Procedure in a large cohort of patients with colorectal liver metastases. Ann Surg 272:793–800. https://doi.org/10.1097/SLA.0000000000004330
Raptis DA, Linecker M, Kambakamba P, Tschuor C, Müller PC, Hadjittofi C et al (2019) Defining benchmark outcomes for ALPPS. Ann Surg 270:835–841. https://doi.org/10.1097/SLA.0000000000003539
Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA et al (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 255:405–414. https://doi.org/10.1097/SLA.0b013e31824856f5
Hasselgren K, Røsok BI, Larsen PN, Sparrelid E, Lindell G, Schultz NA et al (2019) ALPPS improves survival compared with TSH in patients affected of CRLM: survival analysis from the randomized controlled trial LIGRO. Ann Surg. https://doi.org/10.1097/SLA.0000000000003701
Schadde E, Ardiles V, Slankamenac K, Tschuor C, Sergeant G, Amacker N et al (2014) ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg 38:1510–1519. https://doi.org/10.1007/s00268-014-2513-3
Nadalin S, Capobianco I, Li J, Girotti P, Königsrainer I, Königsrainer A (2014) Indications and limits for associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Lessons learned from 15 cases at a single centre. Z Gastroenterol 52:35–42. https://doi.org/10.1055/s-0033-1356364
Truant S, Scatton O, Dokmak S, Regimbeau J-M, Lucidi V, Laurent A et al (2015) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): impact of the inter-stages course on morbi-mortality and implications for management. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 41:674–682. https://doi.org/10.1016/j.ejso.2015.01.004
Wanis KN, Linecker M, Madenci AL, Müller PC, Nüssler N, Brusadin R et al (2021) Variation in complications and mortality following ALPPS at early-adopting centers. HPB 23:46. https://doi.org/10.1016/j.hpb.2020.04.009
McCarron F, Cochran A, Ricker A, Mantha R, Driedger M, Beckman M et al (2023) 10 years, 100 robotic major hepatectomies: a single-center experience. Surg Endosc. https://doi.org/10.1007/s00464-023-10459-2
Görgec B, Zwart M, Nota CL, Bijlstra OD, Bosscha K, de Boer MT et al (2022) Implementation and outcome of robotic liver surgery in the Netherlands: a nationwide analysis. Ann Surg 277:e1269-1277. https://doi.org/10.1097/SLA.0000000000005600
Vicente E, Quijano Y, Ielpo B, Fabra I (2016) First ALPPS procedure using a total robotic approach. Surg Oncol 25:457. https://doi.org/10.1016/j.suronc.2015.10.001
Di Benedetto F, Magistri P, Guerrini GP, Di Sandro S (2022) Robotic liver partition and portal vein embolization for staged hepatectomy for perihilar cholangiocarcinoma. Updat Surg 74:773–777. https://doi.org/10.1007/s13304-021-01209-x
Vauthey J-N, Abdalla EK, Doherty DA, Gertsch P, Fenstermacher MJ, Loyer EM et al (2002) Body surface area and body weight predict total liver volume in Western adults. Liver Transplant Off Publ Am Assoc Study Liver Dis Int Liver Transplant Soc 8:233–240. https://doi.org/10.1053/jlts.2002.31654
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724. https://doi.org/10.1016/j.surg.2010.10.001
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien P-A (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7. https://doi.org/10.1097/SLA.0b013e318296c732
Slankamenac K, Nederlof N, Pessaux P, de Jonge J, Wijnhoven BPL, Breitenstein S et al (2014) The comprehensive complication index: a novel and more sensitive endpoint for assessing outcome and reducing sample size in randomized controlled trials. Ann Surg 260:757–763. https://doi.org/10.1097/SLA.0000000000000948
Magistri P, Assirati G, Ballarin R, Di Sandro S, Di Benedetto F (2021) Major robotic hepatectomies: technical considerations. Updat Surg 73:989–997. https://doi.org/10.1007/s13304-020-00940-1
Serenari M, Ratti F, Guglielmo N, Zanello M, Mocchegiani F, Lenzi J et al (2023) Evolution of minimally invasive techniques and surgical outcomes of ALPPS in Italy: a comprehensive trend analysis over 10 years from a national prospective registry. Surg Endosc 37:5285–5294. https://doi.org/10.1007/s00464-023-09937-4
Ahmad A, Freeman HD, Corn SD (2023) Robotic major and minor hepatectomy: critical appraisal of learning curve and its impact on outcomes. Surg Endosc 37:2915–2922. https://doi.org/10.1007/s00464-022-09809-3
Chen W, Zhang X, Jiang J, Ye Y, Zhai Z, Hu W et al (2023) Robotic versus laparoscopic liver resection in posterosuperior region: a retrospective study of consecutive cases. Surg Endosc 37:4728–4736. https://doi.org/10.1007/s00464-023-09952-5
Müller PC, Breuer E, Nickel F, Zani S, Kauffmann E, De Franco L et al (2023) Robotic distal pancreatectomy: a novel standard of care? benchmark values for surgical outcomes from 16 international expert centers. Ann Surg 278:253–259. https://doi.org/10.1097/SLA.0000000000005601
Michal K, Sau M, Tamara GMH, Long JR (2020) A better route to ALPPS: minimally invasive vs open ALPPS. Surg Endosc 34:2379–2389. https://doi.org/10.1007/s00464-020-07437-3
Shapera E, Sucandy I, Syblis C, Crespo K, Ja’Karri T, Ross S et al (2022) Cost analysis of robotic versus open hepatectomy: is the robotic platform more expensive? J Robot Surg 16:1409–1417. https://doi.org/10.1007/s11701-022-01375-z
Stewart C, Wong P, Warner S, Raoof M, Singh G, Fong Y et al (2021) Robotic minor hepatectomy: optimizing outcomes and cost of care. HPB 23:700–706. https://doi.org/10.1016/j.hpb.2020.09.005
Klotz R, Mihaljevic AL, Kulu Y, Sander A, Klose C, Behnisch R et al (2024) Robotic versus open partial pancreatoduodenectomy (EUROPA): a randomised controlled stage 2b trial. Lancet Reg Health Eur. https://doi.org/10.1016/j.lanepe.2024.100864
Acknowledgements
The authors want to thank Modena ARTS Foundation (Academy for Robotic and Transplant Surgery) for the support to clinical research.
Funding
Open access funding provided by Università degli Studi di Modena e Reggio Emilia within the CRUI-CARE Agreement. All authors have nothing to disclose.
Author information
Authors and Affiliations
Contributions
C.G. contributed to study design, statistical analysis, interpretation of data, and writing of the manuscript; P.C.M. contributed to study design, interpretation of data, and writing of the manuscript; P.M., J.P.J., R.O., P.K., G.G., C.E.O., S.D.S., P.A.C., and H.P. contributed to interpretation of data and critical revision of the manuscript; F.D.B. contributed to study design, interpretation of data, and critical revision of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Cristiano Guidetti, Philip C. Müller, Paolo Magistri, Jan Philipp Jonas, Roberta Odorizzi, Philipp Kron, Gianpiero Guerrini, Christian E. Oberkofler, Stefano Di Sandro, Pierre-Alain Clavien, Henrik Petrowsky, and Fabrizio Di Benedetto have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 313369 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guidetti, C., Müller, P.C., Magistri, P. et al. Full robotic versus open ALPPS: a bi-institutional comparison of perioperative outcomes. Surg Endosc 38, 3448–3454 (2024). https://doi.org/10.1007/s00464-024-10804-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10804-z