Abstract
Background
Three randomized controlled trials have reported improved functional recovery after Laparoscopic pancreatoduodenectomy (LPD), as compared to open pancreatoduodenectomy (OPD). Long-term results regarding quality of life (QoL) are lacking. The aim of this study was to compare long-term QoL of LPD versus OPD.
Methods and patients
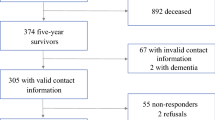
A monocentric retrospective cross-sectional study was performed among patients < 75 years old who underwent LPD or OPD for a benign or premalignant pathology in a high-volume center (2011–2021). An electronic three-part questionnaire was sent to eligible patients, including two diseases specific QoL questionnaires (the European Organization for Research and Treatment in Cancer Quality of Life Questionnaire for cancer (QLQ-C30) and a pancreatic cancer module (PAN26) and a body image questionnaire. Patient demographics and postoperative data were collected and compared between LPD and OPD.
Results
Among 948 patients who underwent PD (137 LPD, 811 OPD), 170 were eligible and 111 responded (58 LPD and 53 OPD). LPD versus OPD showed no difference in mean age (51 vs. 55 years, p = 0.199) and female gender (40% vs. 45%, p = 0.631), but LPD showed lower BMI (24 vs 26; p = 0.028) and higher preoperative pancreatitis (29% vs 13%; p = 0.041). The postoperative outcome showed similar Clavien–Dindo ≥ III morbidity (19% vs. 23%; p = 0.343) and length of stay (24 vs. 21 days, p = 0.963). After a similar median follow-up (3 vs. 3 years; p = 0.122), LPD vs OPD patients reported higher QoL (QLQ-C30: 49.6 vs 56.3; p = 0.07), better pancreas specific health status score (PAN20: 50.5 vs 55.5; p = 0.002), physical functioning (p = 0.002), and activities limitations (p = 0.02). Scar scores were better after LPD regarding esthetics (p = 0.001), satisfaction (p = 0.04), chronic pain at rest (p = 0.036), moving (p = 0.011) or in daily activities (p = 0.02). There was no difference in digestive symptoms (p = 0.995).
Conclusion
This monocentric study found improved long-term QoL in patients undergoing LPD, as compared to OPD, for benign and premalignant diseases. These results could be considered when choosing the surgical approach in these patients.

Similar content being viewed by others
References
Lin D, Yu Z, Chen X, Chen W, Zou Y, Hu J (2020) Laparoscopic versus open pancreatoduodenectomy: a meta-analysis of randomized controlled trials. Rev Esp Enfermedades Dig 112(1):34–40
De Rooij T, Lu MZ, Steen MW, Gerhards MF, Dijkgraaf MG, Busch OR et al (2016) Minimally invasive versus open pancreatoduodenectomy: systematic review and meta-analysis of comparative cohort and registry studies. Ann Surg 264(2):257–267
Nassour I, Wang SC, Christie A, Augustine MM, Porembka MR, Yopp AC et al (2018) Minimally invasive versus open pancreaticoduodenectomy. Ann Surg 268(1):151–157
van Hilst J, De Rooij T, Bosscha K, Brinkman DJ, Van Dieren S, Dijkgraaf MG et al (2019) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4(3):199–207
Asbun HJ, Stauffer JA (2012) Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the accordion severity grading system. J Am Coll Surg 215(6):810–819
Dembinski J, Yoh T, Aussilhou B, Ftériche FS, Hounkonnou CPA, Hentic O et al (2022) The long-term outcomes of laparoscopic versus open pancreatoduodenectomy for ampullary carcinoma showed similar survival: a case-matched comparative study. Surg Endosc 36(7):1–22
Senthilnathan P, Srivatsan Gurumurthy S, Gul SI, Sabnis S, Natesan AV, Palanisamy NV et al (2015) Long-term results of laparoscopic pancreaticoduodenectomy for pancreatic and periampullary cancer—experience of 130 cases from a tertiary-care center in South India. J Laparoendosc Adv Surg Tech 25(4):295–300
Stauffer JA, Coppola A, Villacreses D, Mody K, Johnson E, Li Z et al (2017) Laparoscopic versus open pancreaticoduodenectomy for pancreatic adenocarcinoma: long-term results at a single institution. Surg Endosc 31:2233–2241
Delitto D, Luckhurst CM, Black BS, Beck JL, George TJ, Sarosi GA et al (2016) Oncologic and perioperative outcomes following selective application of laparoscopic pancreaticoduodenectomy for periampullary malignancies. J Gastrointest Surg 20:1343–1349
Conrad C, Basso V, Passot G, Zorzi D, Li L, Chen HC et al (2017) Comparable long-term oncologic outcomes of laparoscopic versus open pancreaticoduodenectomy for adenocarcinoma: a propensity score weighting analysis. Surg Endosc 31:3970–3978
Kantor O, Talamonti MS, Sharpe S, Lutfi W, Winchester DJ, Roggin KK et al (2017) Laparoscopic pancreaticoduodenectomy for adenocarcinoma provides short-term oncologic outcomes and long-term overall survival rates similar to those for open pancreaticoduodenectomy. Am J Surg 213(3):512–515
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240(2):205–213
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ et al (1993) The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in International Clinical Trials in Oncology. J Natl Cancer Inst 85(5):365–376
Fong ZV, Sekigami Y, Qadan M, Fernandez-del Castillo C, Warshaw AL, Lillemoe KD et al (2021) Assessment of the long-term impact of pancreatoduodenectomy on health-related quality of life using the EORTC QLQ-PAN26 module. Ann Surg Oncol 28:4216–4224
van Hilst J, Korrel M, Lof S, de Rooij T, Vissers F, Al-Sarireh B et al (2021) Minimally invasive versus open distal pancreatectomy for pancreatic ductal adenocarcinoma (DIPLOMA): study protocol for a randomized controlled trial. Trials 22(1):1–11
1 BCR, Rahm BC, Madyunus Salayan 2. Google form. As-Salam I (2020) vol 9, no. 2. PANDEMI COVID 19.
The jamovi project (2021) jamovi (Version 2.2) [Computer Software]. https://www.jamovi.org
van Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499
Langan RC, Graham JA, Chin AB, Rubinstein AJ, Oza K, Nusbaum JA et al (2014) Laparoscopic-assisted versus open pancreaticoduodenectomy: early favorable physical quality-of-life measures. Surgery 156(2):379–384
Torphy RJ, Chapman BC, Friedman C, Nguyen C, Bartsch CG, Meguid C et al (2019) Quality of life following major laparoscopic or open pancreatic resection. Ann Surg Oncol 26:2985–2993
Moris D, Rushing C, McCracken E, Shah KN, Zani S, Perez A et al (2022) Quality of life associated with open vs minimally invasive pancreaticoduodenectomy: a prospective pilot study. J Am Coll Surg 234(4):632–644
Korrel M, Roelofs A, van Hilst J, Busch OR, Daams F, Festen S et al (2021) Long-term quality of life after minimally invasive vs open distal pancreatectomy in the LEOPARD randomized trial. J Am Coll Surg 233(6):730–739
Funding
No funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Claire Dagorno, Lancelot Marique, Maarten Korrel, Nine de Graaf, Camille Thouny, Gilles Renault, Fadhel Samir Ftériche, Béatrice Aussilhou, Frédérique Maire, Philippe Lévy, Vinciane Rebours, Mickael Lesurtel, Alain Sauvanet, and Safi Dokmak have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dagorno, C., Marique, L., Korrel, M. et al. Long-term quality of life is better after laparoscopic compared to open pancreatoduodenectomy. Surg Endosc 38, 769–779 (2024). https://doi.org/10.1007/s00464-023-10581-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10581-1