Abstract
Objective
With the increased adoption of robotic pancreaticoduodenectomy, the effects of unplanned conversions to an ‘open’ operation are ill-defined. This study aims to describe the impact of unplanned conversions of robotic pancreaticoduodenectomy on short-term outcomes and suggest a stepwise approach for safe unplanned conversions during robotic pancreaticoduodenectomy.
Methods
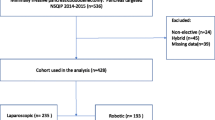
This is an analysis of 400 consecutive patients undergoing robotic pancreaticoduodenectomy in a single high-volume institution. Data are presented as median (mean ± SD), and significance is accepted with 95% probability.
Results
Between November 2012 and February 2023, 184 (46%) women and 216 (54%) men, aged 70 (68 ± 11.0) years, underwent a robotic pancreaticoduodenectomy. Unplanned conversions occurred in 42 (10.5%) patients; 18 (5%) were converted due to unanticipated vascular involvement, 13 (3%) due to failure to obtain definitive control of bleeding, and 11 (3%) due to visceral obesity. Men were more likely to require a conversion than women (29 vs. 13, p = 0.05). Conversions were associated with shorter operative time (376 (323 ± 182.2) vs. 434 (441 ± 98.7) min, p < 0.0001) but higher estimated blood loss (675 (1010 ± 1168.1) vs. 150 (196 ± 176.8) mL, p < 0.0001). Patients that required an unplanned conversion had higher rates of complications with Clavien–Dindo scores of III-V (31% vs. 12%, p = 0.003), longer length of stay (8 (11 ± 11.6) vs. 5 (7 ± 6.2), p = 0.0005), longer ICU length of stay (1 (2 ± 5.1) vs. 0 (0 ± 1.3), p < 0.0001) and higher mortality rates (21% vs. 4%, p = 0.0001). The conversion rate significantly decreased over time (p < 0.0001).
Conclusions
Unplanned conversions of robotic pancreaticoduodenectomy significantly and negatively affect short-term outcomes, including postoperative mortality. Men were more likely to require a conversion than women. The unplanned conversions rates significantly decreased over time, implying that increased proficiency and patient selection may prevent unplanned conversions. An unplanned conversion should be undertaken in an organized stepwise approach to maximize patient safety.




Similar content being viewed by others
References
Rosemurgy AS, Ross SB, Espeut A, Nguyen D, Crespo K, Syblis C, Vasanthakumar P, Sucandy I (2022) Survival and robotic approach for pancreaticoduodenectomy: a propensity score-match study. J Am Coll Surg 234(4):677–684. https://doi.org/10.1097/XCS.0000000000000137
Mazzola M, Giani A, Veronesi V, Bernasconi DP, Benedetti A, Magistro C, Bertoglio CL, De Martini P, Ferrari G (2023) Multidimensional evaluation of the learning curve for totally laparoscopic pancreaticoduodenectomy: a risk-adjusted cumulative summation analysis. HPB (Oxford). https://doi.org/10.1016/j.hpb.2023.02.008
Wang X, Cai Y, Jiang J, Peng B (2020) Laparoscopic pancreaticoduodenectomy: outcomes and experience of 550 patients in a single institution. Ann Surg Oncol 27(11):4562–4573. https://doi.org/10.1245/s10434-020-08533-3
Aziz H, Khan M, Khan S, Serra GP, Goodman MD, Genyk Y, Sheikh MR (2022) Assessing the perioperative complications and outcomes of robotic pancreaticoduodenectomy using the National Cancer Database: is it ready for prime time? J Robot Surg 16(3):687–694. https://doi.org/10.1007/s11701-021-01296-3
Rosemurgy A, Ross S, Bourdeau T, Jacob K, Thomas J, Przetocki V, Luberice K, Sucandy I (2021) Cost analysis of pancreaticoduodenectomy at a high-volume robotic hepatopancreaticobiliary surgery program. J Am Coll Surg 232(4):461–469. https://doi.org/10.1016/j.jamcollsurg.2020.12.062
Mungo B, Hammad A, AlMasri S, Dogeas E, Nassour I, Singhi AD, Zeh HJ 3rd, Hogg ME, Lee KKW, Zureikat AH, Paniccia A (2022) Pancreaticoduodenectomy for benign and premalignant pancreatic and ampullary disease: is robotic surgery the better approach? Surg Endosc. https://doi.org/10.1007/s00464-022-09632-w
Davis CH, Grandhi MS, Gazivoda VP, Greenbaum A, Kennedy TJ, Langan RC, Alexander HR, Pitt HA, August DA (2023) Robotic pancreatoduodenectomy: trends in technique and training challenges. Surg Endosc 37(1):266–273. https://doi.org/10.1007/s00464-022-09469-3
Choi M, Rho SY, Kim SH, Hwang HK, Lee WJ, Kang CM (2022) Total laparoscopic versus robotic-assisted laparoscopic pancreaticoduodenectomy: which one is better? Surg Endosc 36(12):8959–8966. https://doi.org/10.1007/s00464-022-09347-y
Da Dong X, Felsenreich DM, Gogna S, Rojas A, Zhang E, Dong M, Azim A, Gachabayov M (2021) Robotic pancreaticoduodenectomy provides better histopathological outcomes as compared to its open counterpart: a meta-analysis. Sci Rep 11(1):3774. https://doi.org/10.1038/s41598-021-83391-x
Abd El Aziz MA, Grass F, Behm KT, D’Angelo AL, Mathis KL, Dozois EJ, Larson DW (2022) Trends and consequences of surgical conversion in the United States. Surg Endosc. 36(1):82–90. https://doi.org/10.1007/s00464-020-08240-w
Stiles ZE, Dickson PV, Deneve JL, Glazer ES, Dong L, Wan JY, Behrman SW (2018) The impact of unplanned conversion to an open procedure during minimally invasive pancreatectomy. J Surg Res 227:168–177. https://doi.org/10.1016/j.jss.2018.02.028
Halpern AL, Friedman C, Torphy RJ, Al-Musawi MH, Mitchell JD, Scott CD, Meguid RA, McCarter MD, Weyant MJ, Gleisner AL (2020) Conversion to open surgery during minimally invasive esophagectomy portends worse short-term outcomes: an analysis of the National Cancer Database. Surg Endosc 34(8):3470–3478. https://doi.org/10.1007/s00464-019-07124-y
Stiles ZE, Behrman SW, Glazer ES, Deneve JL, Dong L, Wan JY, Dickson PV (2017) Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB (Oxford) 19(11):957–965. https://doi.org/10.1016/j.hpb.2017.06.012
Nassour I, Wang SC, Porembka MR, Augustine MM, Yopp AC, Mansour JC, Minter RM, Choti MA, Polanco PM (2017) Conversion of minimally invasive distal pancreatectomy: predictors and outcomes. Ann Surg Oncol 24(12):3725–3731. https://doi.org/10.1245/s10434-017-6062-5
Lee YF, Albright J, Akram WM, Wu J, Ferraro J, Cleary RK (2018) Unplanned robotic-assisted conversion-to-open colorectal surgery is associated with adverse outcomes. J Gastrointest Surg 22(6):1059–1067. https://doi.org/10.1007/s11605-018-3706-0
Ross S, Downs D, Rosemurgy A (2018) Robotic pylorus-preserving pancreaticoduodenectomy. In: Fong Y, Woo Y, Hyung W et al (eds) The SAGES Atlas of robotic surgery. Springer, Cham, pp 319–334
Ross SB, Bourdeau T, Sucandy I, Rosemurgy A (2021) Robotic pylorus-preserving pancreaticoduodenectomy and cholecystectomy. In: Novitsky Y (ed) Atlas of robotic general surgery. Elsevier, Amsterdam, pp 309–322
Rosemurgy A, Ross S, Bourdeau T, Craigg D, Spence J, Alvior J, Sucandy I (2019) robotic pancreaticoduodenectomy is the future: here and now. J Am Coll Surg 228(4):613–624. https://doi.org/10.1016/j.jamcollsurg.2018.12.040
van Veldhuisen E, Klompmaker S, Janssen QP, Hilal MA, Alseidi A, Balduzzi A, Balzano G, Bassi C, Berrevoet F, Bonds M, Busch OR, Butturini G, Conlon KC, Frigerio IM, Fusai GK, Gagnière J, Griffin O, Hackert T, Halimi A, Keck T, Kleeff J, Klaiber U, Labori KJ, Lesurtel M, Malleo G, Marino MV, Molenaar IQ, Mortensen MB, Nikov A, Pagnanelli M, Pandé R, Pfeiffer P, Pietrasz D, Rangelova E, Roberts KJ, Cunha AS, Salvia R, Strobel O, Tarvainen T, Wilmink JW, Koerkamp BG, Besselink MG, Scientific Committee of the European-African Hepato-Pancreato-Biliary Association (2023) Surgical and oncological outcomes after preoperative FOLFIRINOX chemotherapy in resected pancreatic cancer: an international multicenter cohort study. Ann Surg Oncol. 30(3):1463–1473. https://doi.org/10.1245/s10434-022-12387-2
de Geus SWL, Sachs TE (2023) A paradigm shifts: neoadjuvant therapy for clearly resectable pancreatic cancer. Ann Surg Oncol. https://doi.org/10.1245/s10434-023-13281-1
Tanaka K, Yamada S, Sonohara F, Takami H, Hayashi M, Kanda M, Kobayashi D, Tanaka C, Nakayama G, Koike M, Fujiwara M, Kodera Y (2021) Pancreatic fat and body composition measurements by computed tomography are associated with pancreatic fistula after pancreatectomy. Ann Surg Oncol 28(1):530–538. https://doi.org/10.1245/s10434-020-08581-9
Greenblatt DY, Kelly KJ, Rajamanickam V, Wan Y, Hanson T, Rettammel R, Winslow ER, Cho CS, Weber SM (2011) Preoperative factors predict perioperative morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol 18(8):2126–2135. https://doi.org/10.1245/s10434-011-1594-6
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
Moran Slavin MD, Sharona B. Ross MD, Iswanto Sucandy MD, Sneha Saravanan BS, Cameron Syblis BS, Kaitlyn Crespo BS, Michael Trotto BS, and Alexander Rosemurgy MD have contributed to the conception & design of the study, the analysis & interpretation of data, critical revision of contents, and approval of the final version. The authors agree to be accountable for this manuscript’s contents.
Corresponding author
Ethics declarations
Disclosures
Sharona B. Ross, MD, is a consultant for Intuitive Surgical, Inc. (Sunnyvale, CA) and Ethicon (Cincinnati, OH). Dr. Ross receives educational grants for her Annual Women in Surgery Career Symposium from Intuitive Surgical, Inc. and Medtronic (Minneapolis, MN). Moran Slavin MD, Iswanto Sucandy MD, Sneha Saravanan BS, Cameron Syblis BS, Kaitlyn Crespo BS, Michael Trotto BS, and Alexander Rosemurgy MD have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Oral presentation during the 2023 SAGES Annual Meeting, Montreal, Canada—March 29th, 2023.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Slavin, M., Ross, S.B., Sucandy, I. et al. Unplanned conversions of robotic pancreaticoduodenectomy: short-term outcomes and suggested stepwise approach for a safe conversion. Surg Endosc 38, 964–974 (2024). https://doi.org/10.1007/s00464-023-10527-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10527-7