Abstract
Background
Endoluminal functional impedance planimetry and panometry assesses secondary peristalsis in response to volumetric distention under sedation. We hypothesize that impedance planimetry and panometry can replace high-resolution manometry in the preoperative assessment prior to anti-reflux surgery.
Methods
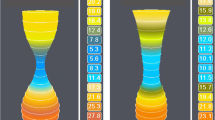
Single institution prospective data were collected from patients undergoing anti-reflux surgery between 2021 and 2023. A 16-cm functional luminal imaging probe (FLIP) assessed planimetry and panometry prior to surgery under general anesthesia at the start of each case. Panometry was recorded and esophageal contractile response was classified as normal (NCR), diminished or disordered (DDCR), or absent (ACR) in real time by a single panometry rater, blinded to preoperative HRM results. FLIP results were then compared to preoperative HRM.
Results
Data were collected from 120 patients, 70.8% female, with mean age of 63 ± 3 years. There were 105 patients with intraoperative panometry, and 15 with panometry collected during preoperative endoscopy. There were 60 patients (50%) who had peristaltic dysfunction on HRM, of whom 57 had FLIP dysmotility (55 DDCR, 2 ACR) resulting in 95.0% sensitivity. There were 3 patients with normal secondary peristalsis on FLIP with abnormal HRM, all ineffective esophageal motility (IEM). No major motility disorder was missed by FLIP. A negative predictive value of 91.9% was calculated from 34/37 patients with normal FLIP panometry and normal HRM. Patients with normal HRM but abnormal FLIP had larger hernias compared to patients with concordant studies (7.5 ± 2.8 cm vs. 5.4 ± 3.2 cm, p = 0.043) and higher preoperative dysphagia scores (1.5 ± 0.7 vs. 1.1 ± 0.3, p = 0.021).
Conclusion
Impedance planimetry and panometry can assess motility under general anesthesia or sedation and is highly sensitive to peristaltic dysfunction. Panometry is a novel tool that has potential to streamline and improve patient care and therefore should be considered as an alternative to HRM, especially in patients in which HRM would be inaccessible or poorly tolerated.




Similar content being viewed by others
References
Carlson DA, Kahrilas PJ, Lin Z et al (2016) Evaluation of esophageal motility utilizing the functional lumen imaging probe (FLIP). Am J Gastroenterol 111(12):1726–1735. https://doi.org/10.1038/ajg.2016.454
Carlson DA, Gyawali CP, Khan A et al (2021) Classifying esophageal motility by FLIP panometry: a study of 722 subjects with manometry. Am J Gastroenterol 116(12):2357–2366. https://doi.org/10.14309/ajg.0000000000001532
Baumann AJ, Donnan EN, Triggs JR et al (2021) Normal functional luminal imaging probe panometry findings associate with lack of major esophageal motility disorder on high-resolution manometry. Clin Gastroenterol Hepatol 19(2):259-268.e1. https://doi.org/10.1016/j.cgh.2020.03.040
Pauwels A, Boecxstaens V, Andrews CN et al (2019) How to select patients for anti-reflux surgery? The ICARUS guidelines (international consensus regarding preoperative examinations and clinical characteristics assessment to select adult patients for antireflux surgery). Gut 68(11):1928–1941. https://doi.org/10.1136/gutjnl-2019-318260
Yadlapati R, Kahrilas PJ, Fox MR et al (2021) Esophageal motility disorders on high resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil 33(1):e14058. https://doi.org/10.1111/nmo.14058
Knyrim K, Wagner HJ, Bethge N, Keymling M, Vakil N (1993) A controlled trial of an expansile metal stent for palliation of esophageal obstruction due to inoperable cancer. N Engl J Med 329(18):1302–1307. https://doi.org/10.1056/NEJM199310283291803
Mellow MH, Pinkas H (1985) Endoscopic laser therapy for malignancies affecting the esophagus and gastroesophageal junction. Analysis of technical and functional efficacy. Arch Intern Med 145(8):1443–1446
Su B, Dunst C, Gould J et al (2021) Experience-based expert consensus on the intra-operative usage of the EndoFLIP impedance planimetry system. Surg Endosc 35(6):2731–2742. https://doi.org/10.1007/s00464-020-07704-3
Su B, Novak S, Callahan ZM, Kuchta K, Carbray J, Ujiki MB (2020) Using impedance planimetry (EndoFLIP™) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc 34(4):1761–1768. https://doi.org/10.1007/s00464-019-06925-5
Wu H, Attaar M, Wong HJ, Campbell M, Kuchta K, Denham EW 3rd, Linn J, Ujiki MB (2022) Impedance planimetry (EndoFLIP) and ideal distensibility ranges for optimal outcomes after Nissen and Toupet fundoplication. J Am Coll Surg 235(3):420–429. https://doi.org/10.1097/XCS.0000000000000273
Mather C, Raftery S, Prys-Roberts C (1992) Somatic movement and oesophageal motility during isoflurane anaesthesia. Br J Anaesth 69(1):40–44. https://doi.org/10.1093/bja/69.1.40
Kuni DR, Silvay G (1989) Lower esophageal contractility: a technique for measuring depth of anesthesia. Biomed Instrum Technol 23(5):388–395
Carlson DA, Gyawali CP, Kahrilas PJ et al (2019) Esophageal motility classification can be established at the time of endoscopy: a study evaluating real-time functional luminal imaging probe panometry. Gastrointest Endosc 90(6):915-923.e1. https://doi.org/10.1016/j.gie.2019.06.039
Carlson DA, Baumann AJ, Donnan EN, Krause A, Kou W, Pandolfino JE (2021) Evaluating esophageal motility beyond primary peristalsis: assessing esophagogastric junction opening mechanics and secondary peristalsis in patients with normal manometry. Neurogastroenterol Motil 33(10):e14116. https://doi.org/10.1111/nmo.14116
Carlson DA, Kathpalia P, Craft J et al (2018) The relationship between esophageal acid exposure and the esophageal response to volumetric distention. Neurogastroenterol Motil. https://doi.org/10.1111/nmo.13240
Farina DA, Carlson DA (2021) Functional luminal imaging probe (FLIP) as an adjunctive modality in evaluation of esophageal dysmotility. Foregut 1(3):286–295. https://doi.org/10.1177/26345161211045617
Carlson DA, Baumann AJ, Prescott JE et al (2022) Validation of secondary peristalsis classification using FLIP panometry in 741 subjects undergoing manometry. Neurogastroenterol Motil 34(1):e14192. https://doi.org/10.1111/nmo.14192
Lee Y, Tahir U, Tessier L, Yang K, Hassan T, Dang J, Kroh M, Hong D (2023) Long-term outcomes following Dor, Toupet, and Nissen fundoplication: a network meta-analysis of randomized controlled trials. Surg Endosc 37(7):5052–5064. https://doi.org/10.1007/s00464-023-10151-5
Amundson JR, Kuchta K, VanDruff VN, Wu H, Campbell M, Hedberg HM, Ujiki MB (2023) Experience with impedance planimetry for surgical foregut disease in 1097 cases. J Am Coll Surg 237(1):35–48. https://doi.org/10.1097/XCS.0000000000000675
O’Rourke AK, Lazar A, Murphy B, Castell DO, Martin-Harris B (2016) Utility of esophagram versus high-resolution manometry in the detection of esophageal dysmotility. Otolaryngol-Head Neck Surg 154(5):888–891. https://doi.org/10.1177/0194599816629379
Ott D, Richter J, Chen Y, Wu W, Gelfand D, Castell D (1987) Esophageal radiography and manometry: correlation in 172 patients with dysphagia. AJR Am J Roentgenol 149:307–311. https://doi.org/10.2214/ajr.149.2.307
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Michael B. Ujiki, scientific advisory board member of Boston Scientific and Apollo, receives payment for lectures from Medtronic and Gore. Vanessa N. VanDruff, Julia R. Amundson, Stephanie Joseph, Simon Che, Chris Zimmermann, H. Mason Hedberg, and Kristine Kuchta have no conflict or financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript was accepted for an oral presentation at the 2023 Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Conference on March 29, 2023, in Montreal, Quebec, Canada.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
VanDruff, V.N., Amundson, J.R., Joseph, S. et al. Impedance planimetry and panometry (EndoFLIP™) can replace manometry in preoperative anti-reflux surgery assessment. Surg Endosc 38, 339–347 (2024). https://doi.org/10.1007/s00464-023-10419-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10419-w