Abstract
Background
Laparoscopic sleeve gastrectomy (LSG) has become the preferred bariatric procedure in many countries. However, new onset erosive esophagitis (EE) is a major shortcoming. Current recommendation is esophago-gastro-duodenoscopy (EGD) should be performed routinely at 1 year and subsequently every 2–3 years to enable the early detection of Barrett’s or esophageal adenocarcinoma. This would put significant strains on resources and costs of bariatric program. Our study assesses the association between and diagnostic value of salivary pepsin concentration and endoscopically proven EE in post-LSG patients as a surrogate for EGD.
Methods
Twenty patients on routine post-LSG endoscopy between June and September 2022 were recruited for this correlational pilot study. Under supervision, fasting and post-prandial saliva sample was collected and analyzed by Peptest lateral flow device. EGD examinations were performed, and patients completed a validated 25-item QoLRAD questionnaire.
Results
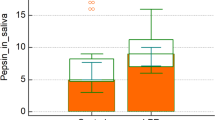
We found a significant correlation between positive endoscopy findings of EE and salivary pepsin concentrations. The normal group had a lower mean fasting pepsin level (13.13 ng/mL ± 18.97) versus the EE-group (90.55 ng/mL ± 81.28, p = 0.009) and lower mean post-prandial pepsin level (30.50 ng/mL ± 57.72) versus the EE-group (135.09 ng/mL ± 130.17, p = 0.02). The predictive probabilities from the binary regression of fasting and post-prandial pepsin concentrations yield AUC of 0.955 ± 0.044 (95% CI 0.868 to 1.000, p < 0.001).
Conclusion
Our study distinctively identified salivary pepsin to have excellent sensitivity and negative predictive value in EE, potentially useful to preclude the need for post-LSG EGD in asymptomatic patients with low salivary pepsin.



Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J et al (2018) IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg 28(12):3783–3794
Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Kow L (2021) Bariatric surgery survey 2018: similarities and disparities among the 5 IFSO chapters. Obes Surg 31(5):1937–1948
Sheppard CE, Sadowski DC, de Gara CJ, Karmali S, Birch DW (2015) Rates of reflux before and after laparoscopic sleeve gastrectomy for severe obesity. Obes Surg 25(5):763–768
Tai C-M, Huang C-K, Lee Y-C, Chang C-Y, Lee C-T, Lin J-T (2013) Increase in gastroesophageal reflux disease symptoms and erosive esophagitis 1 year after laparoscopic sleeve gastrectomy among obese adults. Surg Endosc 27(4):1260–1266
Vakil N, Van Zanten S, Kahrilas P, Dent J, Jones R (2007) The Montreal definition and classification of gastroesophageal reflux disease: a global, evidence-based consensus paper. Z Gastroenterol 45(11):1125–1140
Lim CH, Lee PC, Lim E, Tan J, Chan WH, Tan HC et al (2019) Correlation between symptomatic gastro-esophageal reflux disease (GERD) and erosive esophagitis (EE) post-vertical sleeve gastrectomy (VSG). Obes Surg 29(1):207–214
Brown WA, Johari Halim Shah Y, Balalis G, Bashir A, Ramos A, Kow L et al (2020) IFSO position statement on the role of esophago-gastro-duodenal endoscopy prior to and after bariatric and metabolic surgery procedures. Obes Surg 30(8):3135–3153. https://doi.org/10.1007/s11695-020-04720-z
Campos GM, Mazzini GS, Altieri MS, Docimo S Jr, DeMaria EJ, Rogers AM et al (2021) ASMBS position statement on the rationale for performance of upper gastrointestinal endoscopy before and after metabolic and bariatric surgery. Surg Obes Relat Dis 17(5):837–847
Ben-Menachem T, Decker GA, Early DS, Evans J, Fanelli RD, Fisher DA et al (2012) Adverse events of upper GI endoscopy. Gastrointest Endosc 76(4):707–718. https://doi.org/10.1016/j.gie.2012.03.252
Bardhan KD, Strugala V, Dettmar PW (2012) Reflux revisited: advancing the role of pepsin. Int J Otolaryngol 2012:1–13
Goldberg HI, Dodds WJ, Gee S, Montgomery C, Zboralske FF (1969) Role of acid and pepsin in acute experimental esophagitis. Gastroenterology 56(2):223–230
Lim CH, Lee PC, Lim E, Eng A, Chan WH, Tan HC et al (2020) Resolution of erosive esophagitis after conversion from vertical sleeve gastrectomy to Roux-en-Y gastric bypass. Obes Surg 30(12):4751–4759
Faul F, Erdfelder E, Lang A-G, Buchner A (2007) G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39(2):175–191
Hayat JO, Gabieta-Somnez S, Yazaki E, Kang J-Y, Woodcock A, Dettmar P et al (2015) Pepsin in saliva for the diagnosis of gastro-oesophageal reflux disease. Gut 64(3):373–380
Lundell L, Dent J, Bennett J, Blum A, Armstrong D, Galmiche J et al (1999) Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 45(2):172–180
Du X, Wang F, Hu Z, Wu J, Wang Z, Yan C et al (2017) The diagnostic value of pepsin detection in saliva for gastro-esophageal reflux disease: a preliminary study from China. BMC Gastroenterol 17(1):1–9
Boulton KH, Fisher J, Woodcock AD, Dettmar PW (2021) Pepsin as a biomarker for self-diagnosing reflux associated symptoms in UK and USA individuals. Ann Esophagus 4:23
Bor S, Capanoglu D, Vardar R, Woodcock AD, Fisher J, Dettmar PW (2019) Validation of Peptest™ in patients with gastro-esophageal reflux disease and laryngopharyngeal reflux undergoing impedance testing. J Gastrointest Liver Dis 28(4):383–387
Guo Z, Jiang J, Wu H, Zhu J, Zhang S, Zhang C (2021) Salivary Peptest for laryngopharyngeal reflux and gastroesophageal reflux disease: a systemic review and meta-analysis. Medicine (Baltim) 100(32):e26756. https://doi.org/10.1097/md.0000000000026756
Dettmar PW, Watson M, McGlashan J, Tatla T, Nicholaides A, Bottomley K et al (2020) A multicentre study in UK voice clinics evaluating the non-invasive reflux diagnostic Peptest in LPR patients. SN Compr Clin Med 2(1):57–65
Choi JE, Lyons KM, Kieser JA, Waddell NJ (2017) Diurnal variation of intraoral pH and temperature. BDJ Open 3(1):1–6
Fornari F, Blondeau K, Mertens V, Tack J, Sifrim D (2011) Nocturnal gastroesophageal reflux revisited by impedance-pH monitoring. J Neurogastroenterol Motil 17(2):148
Fass R, Sifrim D (2009) Management of heartburn not responding to proton pump inhibitors. Gut 58(2):295–309
Labenz J, Malfertheiner P (2005) Treatment of uncomplicated reflux disease. World J Gastroenterol 11(28):4291
Johnston N, Wells CW, Blumin JH, Toohill RJ, Merati AL (2007) Receptor-mediated uptake of pepsin by laryngeal epithelial cells. Ann Otol Rhinol Laryngol 116(12):934–938
Tutuian R, Castell DO (2004) Nocturnal acid breakthrough—approach to management. Medscape Gen Med 6(4):11
Peghini PL, Katz PO, Castell DO (1998) Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects. Gastroenterology 115(6):1335–1339
Martínek J, Pantoflícková D, Hucl T, Beneš M, Dorta G, Lukáš M et al (2004) Absence of nocturnal acid breakthrough in Helicobacter pylori-positive subjects treated with twice-daily omeprazole. Eur J Gastroenterol Hepatol 16(5):445–450
Koufman JA, Johnston N (2012) Potential benefits of pH 8.8 alkaline drinking water as an adjunct in the treatment of reflux disease. Ann Otol Rhinol Laryngol 121(7):431–434
Roberts N, Taylor W (2003) Comparative pepstatin inhibition studies on individual human pepsins and pepsinogens 1, 3 and 5 (gastricsin) and pig pepsin A. J Enzyme Inhib Med Chem 18(3):209–217
Umezawa H, Aoyagi T, Morishima H, Hazime Matsuzaki M, Hamada M, Takeuchi T (1970) Pepstatin, a new pepsin inhibitor produced by agtinomygetes. J Antibiot 23(5):259–262
Kunimoto S, Aoyagi T, Morishima H, Takeuchi T, Umezawa H (1972) Mechanism of inhibition of pepsin by pepstatin. J Antibiot 25(4):251–255
Wang CP, Wang CC, Lien HC, Lin WJ, Wu SH, Liang KL et al (2019) Saliva pepsin detection and proton pump inhibitor response in suspected laryngopharyngeal reflux. Laryngoscope 129(3):709–714
Funding
This work is supported by SGH Health Development Fund (FZGRBARSUR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jinyuan Gan, Yarn Kit Chan, Deepa Chandra Segaran, Jean-Paul Kovalik, Alvin Eng, Phong Ching Lee, Jeremy Tan, and Chin Hong Lim have no conflict of interest or financial ties to disclose.
Informed consent
Written informed consent was obtained from all patients for recruitment into this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gan, J., Chan, Y.K., Segaran, D.C. et al. Pepsin in saliva for the diagnosis of erosive esophagitis post-sleeve gastrectomy: a prospective observational study. Surg Endosc 37, 5816–5824 (2023). https://doi.org/10.1007/s00464-023-10050-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10050-9