Abstract
Background
Redo fundoplication (RF) and Roux-en-Y diversion (RNY) are both accepted surgical treatments after failed fundoplication. However, due to higher reported morbidity, RNY is more commonly performed only after several surgical failures. In our experience, RNY at an earlier point of the disease progression seems to be related with better outcomes. The aim of this study was to investigate this aspect by comparing the results between RF and RNY performed by a single surgeon over 3 years at our institution.
Methods
A prospectively maintained database was reviewed to identify patients who underwent RF or RNY at our institution between 2016 and 2019 by a single surgeon (author SKM). Patients with previous bariatric surgery were excluded.
Results
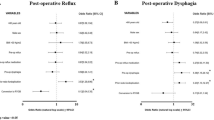
Of 43 patients, 28 underwent RF and 15 underwent RNY (mean body mass index 28.6 and 32.7 kg/m2, respectively, p = 0.01). The number of previous antireflux surgeries for the RF and RNY groups was 1 (82% vs 80%, p > 0.99), 2 (18% vs 7%, p = 0.4), and more than 2 (0% vs 13%, p = 0.1). RNY took longer than RF (median, 165 vs 137 min, p = 0.02), but both groups had a median estimated blood loss of 50 ml (p = 0.82). There was no difference in intraoperative complications (25% vs 20% for RF and RYN, respectively, p > 0.99). Postoperative complications were more common in the RF than in the RYN group (21% vs 7%, p = 0.39). Median hospital stay was 3 days for both groups (p = 0.78). At short-term follow-up, the mean quality of life score was similar for the RF and RYN groups (11.5 vs 12.2, p = 0.8).
Conclusions
RNY diversion, if performed by experienced hands and at an earlier point of disease progression, has comparable perioperative morbidity to RF and should be considered as a feasible and safe option for definitive treatment of failed antireflux surgery.

Similar content being viewed by others
References
Katz PO, Gerson LB, Vela MF (2013) Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 108:308–328 (quiz 329)
Dallemagne B, Weerts J, Markiewicz S, Dewandre JM, Wahlen C, Monami B, Jehaes C (2006) Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc 20:159–165
Granderath FA, Kamolz T, Schweiger UM, Pasiut M, Haas CF, Wykypiel H, Pointner R (2002) Long-term results of laparoscopic antireflux surgery. Surg Endosc 16:753–757
DeMeester TR, Bonavina L, Albertucci M (1986) Nissen fundoplication for gastroesophageal reflux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg 204:9–20
Iqbal A, Awad Z, Simkins J, Shah R, Haider M, Salinas V, Turaga K, Karu A, Mittal SK, Filipi CJ (2006) Repair of 104 failed anti-reflux operations. Ann Surg 244:42–51
Peters JH, Heimbucher J, Kauer WK, Incarbone R, Bremner CG, DeMeester TR (1995) Clinical and physiologic comparison of laparoscopic and open Nissen fundoplication. J Am Coll Surg 180:385–393
Furnée EJ, Draaisma WA, Broeders IA, Gooszen HG (2009) Surgical reintervention after failed antireflux surgery: a systematic review of the literature. J Gastrointest Surg 13:1539–1549
van Beek DB, Auyang ED, Soper NJ (2011) A comprehensive review of laparoscopic redo fundoplication. Surg Endosc 25:706–712
Booth MI, Jones L, Stratford J, Dehn TC (2002) Results of laparoscopic Nissen fundoplication at 2–8 years after surgery. Br J Surg 89:476–481
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg 193:428–439
Dallemagne B, Weerts JM, Jehaes C, Markiewicz S (1996) Causes of failures of laparoscopic antireflux operations. Surg Endosc 10:305–310
Hunter JG, Smith CD, Branum GD, Waring JP, Trus TL, Cornwell M, Galloway K (1999) Laparoscopic fundoplication failures: patterns of failure and response to fundoplication revision. Ann Surg 230:595–604 (discussion 604-596)
Yamamoto SR, Hoshino M, Nandipati KC, Lee TH, Mittal SK (2014) Long-term outcomes of reintervention for failed fundoplication: redo fundoplication versus Roux-en-Y reconstruction. Surg Endosc 28:42–48
Wilshire CL, Louie BE, Shultz D, Jutric Z, Farivar AS, Aye RW (2016) Clinical outcomes of reoperation for failed antireflux operations. Ann Thorac Surg 101:1290–1296
Mittal SK, Légner A, Tsuboi K, Juhasz A, Bathla L, Lee TH (2013) Roux-en-Y reconstruction is superior to redo fundoplication in a subset of patients with failed antireflux surgery. Surg Endosc 27:927–935
Makris KI, Panwar A, Willer BL, Ali A, Sramek KL, Lee TH, Mittal SK (2012) The role of short-limb Roux-en-Y reconstruction for failed antireflux surgery: a single-center 5-year experience. Surg Endosc 26:1279–1286
Landreneau JP, Strong AT, Kroh MD, Rodriguez JH, El-Hayek K (2020) Minimally invasive Roux-en-Y reconstruction as a salvage operation after failed nissen fundoplication. Surg Endosc 34:2211–2218
Weber CE, Kanani Z, Schumm M, Helm M, Gould JC (2019) Roux-en-Y gastric bypass as a salvage procedure in complicated patients with failed fundoplication(s). Surg Endosc 33:738–744
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE (2015) The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20:130–134
Makris KI, Lee T, Mittal SK (2009) Roux-en-Y reconstruction for failed fundoplication. J Gastrointest Surg 13:2226–2232
Légner A, Tsuboi K, Bathla L, Lee T, Morrow LE, Mittal SK (2011) Reoperative antireflux surgery for dysphagia. Surg Endosc 25:1160–1167
Awais O, Luketich JD, Tam J, Irshad K, Schuchert MJ, Landreneau RJ, Pennathur A (2008) Roux-en-Y near esophagojejunostomy for intractable gastroesophageal reflux after antireflux surgery. Ann Thorac Surg 85:1954–1959 (discussion 1959-1961)
Williams VA, Watson TJ, Gellersen O, Feuerlein S, Molena D, Sillin LF, Jones C, Peters JH (2007) Gastrectomy as a remedial operation for failed fundoplication. J Gastrointest Surg 11:29–35
Frezza EE, Ikramuddin S, Gourash W, Rakitt T, Kingston A, Luketich J, Schauer P (2002) Symptomatic improvement in gastroesophageal reflux disease (GERD) following laparoscopic Roux-en-Y gastric bypass. Surg Endosc 16:1027–1031
Patterson EJ, Davis DG, Khajanchee Y, Swanström LL (2003) Comparison of objective outcomes following laparoscopic Nissen fundoplication versus laparoscopic gastric bypass in the morbidly obese with heartburn. Surg Endosc 17:1561–1565
Stefanidis D, Navarro F, Augenstein VA, Gersin KS, Heniford BT (2012) Laparoscopic fundoplication takedown with conversion to Roux-en-Y gastric bypass leads to excellent reflux control and quality of life after fundoplication failure. Surg Endosc 26:3521–3527
Coakley KM, Groene SA, Colavita PD, Prasad T, Stefanidis D, Lincourt AE, Augenstein VA, Gersin K, Heniford BT (2018) Roux-En-Y gastric bypass following failed fundoplication. Surg Endosc 32:3517–3524
Del Campo SEM, Mansfield SA, Suzo AJ, Hazey JW, Perry KA (2017) Laparoscopic redo fundoplication improves disease-specific and global quality of life following failed laparoscopic or open fundoplication. Surg Endosc 31:4649–4655
Pennathur A, Awais O, Luketich JD (2010) Minimally invasive redo antireflux surgery: lessons learned. Ann Thorac Surg 89:S2174-2179
Obeid NR, Altieri MS, Yang J, Park J, Price K, Bates A, Pryor AD (2018) Patterns of reoperation after failed fundoplication: an analysis of 9462 patients. Surg Endosc 32:345–350
Acknowledgements
The authors thank Kristine Nally for her expert editorial assistance.
Funding
No outside funding was obtained for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Luca Giulini, Deepika Razia and Sumeet K. Mittal have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These data were presented at the Resident and Fellows Research Conference, Society for Surgery of the Alimentary Tract (SSAT), Virtual Digestive Disease Week 2020 (May 2–5).
Rights and permissions
About this article
Cite this article
Giulini, L., Razia, D. & Mittal, S.K. Redo fundoplication and early Roux-en-Y diversion for failed fundoplication: a 3-year single-center experience. Surg Endosc 36, 3094–3099 (2022). https://doi.org/10.1007/s00464-021-08610-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08610-y