Abstract
Introduction
For patients with a gallbladder in situ, choledocholithiasis is a common presenting symptom. Both two-session endoscopic retrograde cholangiopancreatography (ERCP) and subsequent cholecystectomy (CCY) and single-stage (simultaneous CCY/ERCP) have been described. We utilize an antegrade wire, rendezvous cannulation (AWRC) technique to facilitate ERCP during CCY. We hypothesized that AWRC would eliminate episodes of post-ERCP pancreatitis (PEP).
Methods
An IRB approved, retrospective review of patients who underwent ERCP via AWRC for choledocholithiasis during CCY was performed. Patient characteristics, pre/postoperative laboratory values, complications, and readmissions were reviewed. AWRC was conducted during laparoscopic or open CCY for evidence of choledocholithiasis with or without preoperative biliary pancreatitis or cholangitis. Following confirmatory intraoperative cholangiogram, a flexible tip guidewire was inserted antegrade into the cystic ductotomy, through the bile duct across the ampulla and retrieved in the duodenum with a duodenoscope. Standard ERCP maneuvers to clear the bile duct are then performed over the wire.
Results
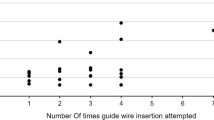
Thirty-seven patients (27 female, age 19–77, BMI 21–50 kg/m2) underwent intraoperative ERCP via AWRC technique during CCY. Seventeen underwent CCY for acute cholecystitis. Fifteen patients underwent transgastric ERCP in the setting of previous Roux-en-Y gastric bypass. Mean total operative time was 214 min. Mean ERCP time was 31 min. Thirty-three patients had biliary stents placed. There were no cannulations or injections of the pancreatic duct. There were no intraoperative complications associated with the ERCP and no patients developed PEP. Three patients developed a postoperative subhepatic abscess requiring drainage.
Conclusion
AWRC is a useful technique for safe and efficient bile duct cannulation for therapeutic ERCP in the setting of choledocholithiasis at the time of CCY. Despite supine (rather than the traditional prone) positioning, total ERCP times were short and we eliminated any manipulation of the pancreatic duct. No patients in our series developed PEP or post-sphincterotomy bleeding.


Similar content being viewed by others
References
Committee ASoP, Maple JT, Ikenberry SO et al (2011) The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc 74:731–744
Thaker AM, Mosko JD, Berzin TM (2015) Post-endoscopic retrograde cholangiopancreatography pancreatitis. Gastroenterol Rep (Oxf) 3:32–40
Cheng CL, Sherman S, Watkins JL et al (2006) Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol 101:139–147
Freeman ML, DiSario JA, Nelson DB et al (2001) Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc 54:425–434
Ding G, Cai W, Qin M (2014) Single-stage vs. two-stage management for concomitant gallstones and common bile duct stones: a prospective randomized trial with long-term follow-up. J Gastrointest Surg 18:947–951
Poulose BK, Arbogast PG, Holzman MD (2006) National analysis of in-hospital resource utilization in choledocholithiasis management using propensity scores. Surg Endosc 20:186–190
Reinders JS, Goud A, Timmer R et al (2010) Early laparoscopic cholecystectomy improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis. Gastroenterology 138:2315–2320
Wandling MW, Hungness ES, Pavey ES et al (2016) Nationwide Assessment of Trends in Choledocholithiasis Management in the United States from 1998 to 2013. JAMA Surg 151:1125–1130
Cavina E, Franceschi M, Sidoti F et al (1998) Laparo-endoscopic “rendezvous”: a new technique in the choledocholithiasis treatment. Hepatogastroenterology 45:1430–1435
Sahoo MR, Kumar AT, Patnaik A (2014) Randomised study on single stage laparo-endoscopic rendezvous (intra-operative ERCP) procedure versus two stage approach (Pre-operative ERCP followed by laparoscopic cholecystectomy) for the management of cholelithiasis with choledocholithiasis. J Minim Access Surg 10:139–143
Martinez J, Guerrero L, Byers P et al (2006) Endoscopic retrograde cholangiopancreatography and gastroduodenoscopy after Roux-en-Y gastric bypass. Surg Endosc 20:1548–1550
Banks PA, Bollen TL, Dervenis C et al (2013) Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut 62:102–111
Tenner S, Dubner H, Steinberg W (1994) Predicting gallstone pancreatitis with laboratory parameters: a meta-analysis. Am J Gastroenterol 89:1863–1866
Matull WR, Pereira SP, O’Donohue JW (2006) Biochemical markers of acute pancreatitis. J Clin Pathol 59:340–344
Manes G, Baratti C, Ardizzone S et al (2008) Over-the-catheter precut to gain access to the biliary duct during ERCP rendezvous. Surg Endosc 22:2323–2325
Haseeb A, Freeman ML (2019) Guidewire in the pancreatic duct: key to risk and rescue for post-ERCP pancreatitis. Gastrointest Endosc 89(2):309–310
Dumonceau JM, Andriulli A, Elmunzer BJ et al (2014) Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - updated June 2014. Endoscopy 46:799–815
Ricci C, Pagano N, Taffurelli G et al (2018) Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct calculi: a systematic review and network meta-analysis. JAMA Surg 153:e181167
Hanif F, Ahmed Z, Samie MA, Nassar AH (2010) Laparoscopic transcystic common bile duct exploration: the treatment of first choice for common bile duct stones. Surg Endosc 24(7):1552–1556
Zerey M, Haggerty S, Richardson W et al (2018) Laparoscopic common bile duct evaluation. Surg Endosc 32(6):2603–2612
Funding
Eric M. Pauli MD receives honoraria from CR Bard, Cook Biotech, and Boston Scientific, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Joshua S. Winder, Ryan M. Juza, Vamsi V. Alli, Ann M. Rogers, and Randy S. Haluck have no financial conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (WMV 238477 kb)
Rights and permissions
About this article
Cite this article
Winder, J.S., Juza, R.M., Alli, V.V. et al. Concomitant laparoscopic cholecystectomy and antegrade wire, rendezvous cannulation of the biliary tree may reduce post-ERCP pancreatitis events. Surg Endosc 34, 3216–3222 (2020). https://doi.org/10.1007/s00464-019-07074-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07074-5