Abstract
Introduction
Recent data suggest a wide range of conversion (4.9–20%) from laparoscopic (LC) to open cholecystectomy (OC) despite increasing surgeon familiarity and superior equipment. Previously identified risk factors for conversion include increased age, male gender, diabetes, and emergent surgeries. Recent studies also suggest that formal minimally invasive surgical training (MIST) reduces conversion rates. We sought to determine conversion rates in our population, a rural academic medical center, and identify any significant risks for conversion.
Methods
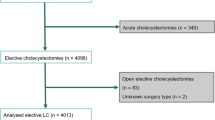
We conducted a single-center retrospective review of 2810 cholecystectomies performed over a seven-year period (2009–2016).
Results
Our study included 837 (29.8%) males and 1973 (70.2%) females with a mean age of 49.2 years. Forty-two percent of cases were done by surgeons with MIST. A total of 139 (4.95%) cases were converted to OC. Univariate predictors of conversion to OC included male gender, age ≥65, urgent and emergent admissions, and MIST of the surgeon. In multivariate modeling, which included significant univariate predictors of conversion, independent predictors of conversion to OC included urgent or emergent admission, male gender, and age ≥65. MIST status was no longer a significant predictor.
Conclusion
Our conversion rate from LC to OC falls within the lower range of recently published rates. This is likely multifactorial, and reflects increasing familiarity of the laparoscopic technique, improved quality of laparoscopic equipment, and/or prior knowledge of preoperative risk factors for conversion. Our results, consistent with previous literature, show a reduced conversion rate among surgeons with MIST. This finding, albeit not significant on multivariate analysis, may offer insight into a potential alterable preoperative risk factor for conversion and warrants further research. Further knowledge about the impact MIST has on conversion may provide a feasible preoperative approach to reducing conversion to OC, thereby reducing costs and overall patient morbidity.
Similar content being viewed by others
References
Goldman L (2011) Goldman’s cecil medicine (ed 24). Elsevier Saunders, Philadelphia
Reynolds W Jr (2001) The first laparoscopic cholecystectomy. JSLS 5(1):89–94
Blum CA, Adams DB (2011) Who did the first laparoscopic cholecystectomy? J Minim Access Surg 7(3):165–168. doi:10.4103/0972-9941.83506
Sirinek KR, Willis R, Schwesinger WH (2016) Who will be able to perform open biliary surgery in 2025? J Am Coll Surg 223(1):110–115. doi:10.1016/j.jamcollsurg.2016.02.019
Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Saverio Di, Gioacchino L, Giulia M, Ceresoli M, Corbella D, Sartellia M, Sugrue M, Ansaloni L (2015) Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg 18:196–204. doi:10.1016/j.ijsu.2015.04.083
Abelson JS, Afaneh C, Rich BS, Dakin G, Zarnegar R, Fahey TJ 3rd, Pomp A (2015) Advanced laparoscopic fellowship training decreases conversion rates during laparoscopic cholecystectomy for acute biliary diseases: a retrospective cohort study. Int J Surg 13:221–226. doi:10.1016/j.ijsu.2014.12.016
Licciardello A, Arena M, Nicosia A, Di Stefano B, Cali G, Arena G, Minutolo V (2014) Preoperative risk factors for conversion from laparoscopic to open cholecystectomy. Eur Rev Med Pharmacol Sci 18(2 Suppl):60–68
Sakpal SV, Bindra SS, Chamberlain RS (2010) Laparoscopic cholecystectomy conversion rates two decades later. JSLS 14(4):476–483. doi:10.4293/108680810X12924466008240
To KB, Cherry-Bukowiec JR, Englesbe MJ, Terjimanian MN, Shijie C, Campbell DA Jr, Napolitano LM (2013) Emergent versus elective cholecystectomy: conversion rates and outcomes. Surg Infect (Larchmt) 14(6):512–519. doi:10.1089/sur.2012.160
Yajima H, Kanai H, Son K, Yoshida K, Yanaga K (2014) Reasons and risk factors for intraoperative conversion from laparoscopic to open cholecystectomy. Surg Today 44(1):80–83
Philip Rothman J, Burcharth J, Pommergaard HC, Viereck S, Rosenberg J (2016) preoperative risk factors for conversion of laparoscopic cholecystectomy to open surgery—a systematic review and meta-analysis of observational studies. Dig Surg 33(5):414–423. doi:10.1159/000445505
Yang TF, Guo L, Wang Q (2014) Evaluation of preoperative risk factor for converting laparoscopic to open cholecystectomy: a meta-analysis. Hepatogastroenterology 61(132):958–965
Wrenn SM, Callas PW, Abu-Jaish W (2016) Histopathological examination of specimen following cholecystectomy: are we accepting resect and discard? Surg Endosc. doi:10.1007/s00464-016-5002-y
Acknowledgements
Aggregate patient data were provided by the Jeffords Institute for Quality at the University of Vermont Medical Center. We greatly appreciate the assistance from Jeffords Institute, particularly Dr. Allison Holm (Senior Research Specialist) and Mia Nowlan (Measurement Analyst). The authors would also like to thank Charles Maclean MD for his insight and suggested revisions throughout the drafting of this manuscript.
Author information
Authors and Affiliations
Contributions
Author contributions
SC is the primary author of manuscript text and major contributor to study design, and preformed data collection, review of literature, and statistical analysis. PC provided critical statistical analysis and support and assisted with manuscript revisions. SW assisted with the procurement of data and study design, as well as provided critical revisions to the manuscript. WA-J (senior author) is the principal investigator for the study, designed the idea for the study, and assisted with manuscript drafting and revision.
Corresponding authors
Ethics declarations
Disclosures
Mr. Steven J. Coffin, and Drs. Sean M. Wrenn, Peter W. Callas, and Wasef Abu-Jaish have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Coffin, S.J., Wrenn, S.M., Callas, P.W. et al. Three decades later: investigating the rate of and risks for conversion from laparoscopic to open cholecystectomy. Surg Endosc 32, 923–929 (2018). https://doi.org/10.1007/s00464-017-5767-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5767-7