Abstract
Background
Endoscopic therapy for duodenal adenomas is becoming increasingly important. However, only a few studies have been published on the topic, mainly with retrospective data.
Methods
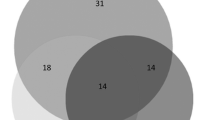
This prospective study was carried out to determine complication rates and associated risk factors during and after endoscopic therapy for duodenal adenomas. Between May 2011 and October 2012, 50 patients (with 61 duodenal adenomas) were included. Sixty-one duodenal adenomas were resected endoscopically. Complications (e.g., bleeding, pain, fever, pancreatitis, and perforation) were recorded. Associations between bleeding and other factors—sex, age, anticoagulation, location and size of adenomas, etiology, lesion morphology, resection type, and argon plasma coagulation (APC) for bleeding prophylaxis—were then investigated.
Results
Bleeding was the main complication. Major bleeding occurred in four cases (6.5 %) and minor bleeding in 11 (18 %). One occult perforation also occurred. There was a statistically significant association between bleeding and the size of the adenoma (P = 0.012). APC for bleeding prophylaxis showed a promising trend, with an odds ratio of 0.31, reducing the bleeding risk by two-thirds in this study. However, due to the small number of six patients that received bleeding prophylaxis with APC therapy, this result was not statistically significant (P = 0.31).
Conclusions
Bleeding is the main complication in endoscopic therapy for duodenal adenomas. The bleeding risk increases significantly with adenoma size. Prophylactic APC seems to reduce the bleeding rate—however, because of the relatively small number of patients treated with APC, this partial result was not statistically relevant. Due to the relevant rate of complications, endoscopic resection of duodenal adenomas is only recommended in an in-patient setting.



Similar content being viewed by others
Abbreviations
- APC:
-
Argon plasma coagulation
- EGD:
-
Esophagogastroduodenoscopy
- ER:
-
Endoscopic resection
- EUS:
-
Endoscopic ultrasound
- GEE:
-
General Estimating Equations
- FAP:
-
Familial adenomatous polyposis
- FICE:
-
Fuji Intelligent Chromo Endoscopy
- HGIN:
-
High-grade intraepithelial neoplasia
- INR:
-
International normalized ratio
- MAP:
-
MYH-associated polyposis
- NAD:
-
lesions Nonampullary duodenal lesions
- OTSC:
-
Over the scope clip
- PPPD:
-
Pylorus-preserving pancreatoduodenectomy
- PSD:
-
Pancreas-sparing duodenectomy
- SD:
-
Standard deviation
- Y:
-
Years
References
Sato T, Konishi K, Kimura H et al (1999) Adenoma and tiny carcinoma in adenoma of the papilla of Vater—p53 and PCNA. Hepatogastroenterology 46:1959–1962
Seifert E, Schulte F, Stolte M (1992) Adenoma and carcinoma of the duodenum and papilla of Vater: a clinicopathologic study. Am J Gastroenterol 87:37–42
Spigelman AD, Williams CB, Talbot IC et al (1989) Upper gastrointestinal cancer in patients with familial adenomatous polyposis. Lancet 2(8666):783–785
Standards of Practice Committee, Adler DG, Qureshi W, et al. (2006) The role of endoscopy in ampullary and duodenal adenomas. Gastrointest Endosc 64:849–54
Alexander S, Bourke MJ, Williams SJ et al (2009) EMR of large, sessile, sporadic nonampullary duodenal adenomas: technical aspects and long-term outcome (with videos). Gastrointest Endosc 69:66–73
Ahmad NA, Kochman ML, Long WB et al (2002) Efficacy, safety, and clinical outcomes of endoscopic mucosal resection: a study of 101 cases. Gastrointest Endosc 55:390–396
Oka S, Tanaka S, Nagata S et al (2003) Clinicopathologic features and endoscopic resection of early primary nonampullary duodenal carcinoma. J Clin Gastroenterol 37:381–386
Swan MP, Bourke MJ, Alexander S et al (2009) Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonoscopic polypectomy service. Gastrointest Endosc 70:1128–1136
Bourke MJ (2011) Endoscopic mucosal resection in the colon: a practical guide. Tech Gastrointest Endosc 13:35–49
Lépilliez V, Chemaly M, Ponchon T et al (2008) Endoscopic resection of sporadic duodenal adenomas: an efficient technique with a substantial risk of delayed bleeding. Endoscopy 40:806–810
Apel D, Jakobs R, Spiethoff A et al (2005) Follow-up after endoscopic snare resection of duodenal adenomas. Endoscopy 37:444–448
Jepsen JM, Persson M, Jakobsen NO et al (1994) Prospective study of prevalence and endoscopic and histopathologic characteristics of duodenal polyps in patients submitted to upper endoscopy. Scand J Gastroenterol 29:483–487
Bülow S, Björk J, Christensen IJ et al (2004) Duodenal adenomatosis in familial adenomatous polyposis. Gut 53:381–386
Jagelman DG, DeCosse JJ, Bussey HJ (1988) Upper gastrointestinal cancer in familial adenomatous polyposis. Lancet 1(8595):1149–1151
Vasen HF, Bülow S, Myrhøj T et al (1997) Decision analysis in the management of duodenal adenomatosis in familial adenomatous polyposis. Gut 40:716–719
Offerhaus GJ, Giardiello FM, Krush AJ et al (1992) The risk of upper gastrointestinal cancer in familial adenomatous polyposis. Gastroenterology 102:1980–1982
van Heumen BW, Nieuwenhuis MH, van Goor H et al (2012) Surgical management for advanced duodenal adenomatosis and duodenal cancer in Dutch patients with familial adenomatous polyposis: a nationwide retrospective cohort study. Surgery 151:681–690
Birkmeyer JD, Siewers AE, Finlayson EV et al (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346:1128–1137
Farnell MB, Sakorafas GH, Sarr MG et al (2000) Villous tumors of the duodenum: reappraisal of local vs. extended resection. J Gastrointest Surg 4:13–23
Krukowski ZH, Ewen SW, Davidson AI et al (1988) Operative management of tubulovillous neoplasms of the duodenum and ampulla. Br J Surg 75:150–153
de Castro SM, van Eijck CH, Rutten JP et al (2008) Pancreas-preserving total duodenectomy versus standard pancreatoduodenectomy for patients with familial adenomatous polyposis and polyps in the duodenum. Br J Surg 95:1380–1386
Mackey R, Walsh RM, Chung R et al (2005) Pancreas-sparing duodenectomy is effective management for familial adenomatous polyposis. J Gastrointest Surg 9:1088–1093
Lepistö A, Kiviluoto T, Halttunen J et al (2009) Surveillance and treatment of duodenal adenomatosis in familial adenomatous polyposis. Endoscopy 41:504–509
Gallagher MC, Shankar A, Groves CJ et al (2004) Pylorus-preserving pancreaticoduodenectomy for advanced duodenal disease in familial adenomatous polyposis. Br J Surg 91:1157–1164
Ponchon T (2001) Endoscopic mucosal resection. J Clin Gastroenterol 32:6–10
Haubrich WS, Johnson RB, Foroozan P (1973) Endoscopic removal of a duodenal adenoma. Gastrointest Endosc 19:201
Abbass R, Rigaux J, Al-Kawas FH (2010) Nonampullary duodenal polyps: characteristics and endoscopic management. Gastrointest Endosc 71:754–759
Kedia P, Brensinger C, Ginsberg G (2010) Endoscopic predictors of successful endoluminal eradication in sporadic duodenal adenomas and its acute complications. Gastrointest Endosc 72:1297–1301
Sohn JW, Jeon SW, Cho CM et al (2010) Endoscopic resection of duodenal neoplasms: a single-center study. Surg Endosc 24:3195–3200
Jaganmohan S, Lynch PM, Raju RP et al (2012) Endoscopic management of duodenal adenomas in familial adenomatous polyposis—a single-center experience. Dig Dis Sci 57:732–737
Saurin JC, Chavaillon A, Napoléon B et al (2003) Long-term follow-up of patients with endoscopic treatment of sporadic adenomas of the papilla of Vater. Endoscopy 35:402–406
Catalano MF, Linder JD, Chak A et al (2004) Endoscopic management of adenoma of the major duodenal papilla. Gastrointest Endosc 59:225-2
Kim HK, Chung WC, Lee BI et al (2010) Efficacy and long-term outcome of endoscopic treatment of sporadic nonampullary duodenal adenoma. Gut Liver 4:373–377
König J, Kaiser A, Opfermann P, et al (2014) Acute complications after endoscopic resection of duodenal adenomas. Z Gastroenterol 52:187–192
Fanning SB, Bourke MJ, Williams SJ et al (2012) Giant laterally spreading tumors of the duodenum: endoscopic resection outcomes, limitations, and caveats. Gastrointest Endosc 75:805–812
Binmoeller KF, Shah JN, Bhat YM et al (2013) “Underwater” EMR of sporadic laterally spreading nonampullary duodenal adenomas (with video). Gastrointest Endosc 78:496–502
Shiba M, Higuchi K, Kadouchi K et al (2005) Risk factors for bleeding after endoscopic mucosal resection. World J Gastroenterol 11:7335–7339
Lienert A, Bagshaw PF (2007) Treatment of duodenal adenomas with endoscopic argon plasma coagulation. ANZ J Surg 77:371–373
Manner H, May A, Rabenstein T et al (2007) Prospective evaluation of a new high-power argon plasma coagulation system (hp-APC) in therapeutic gastrointestinal endoscopy. Scand J Gastroenterol 42:397–405
Moss A, Bourke MJ, Williams SJ et al (2011) Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 140:1909–1918
Acknowledgments
We are grateful to Prof. Manfred Berres for statistical support and to Michael Robertson for revising the manuscript.
Disclosure
Financial support and potential competing interests: Andrea May, Jürgen Pohl, and Christian Ell have received speakers’ honoraria from Fujifilm, Inc. Insa Aschmoneit-Messer and Johannes Richl have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aschmoneit-Messer, I., Richl, J., Pohl, J. et al. Prospective study of acute complication rates and associated risk factors in endoscopic therapy for duodenal adenomas. Surg Endosc 29, 1823–1830 (2015). https://doi.org/10.1007/s00464-014-3871-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3871-5