Abstract
Background
Laparoscopy-assisted gastrectomy (LAG) is a complex and time-consuming procedure, which is increasingly used for early gastric cancer (EGC). We provide a multidimensional analysis of the learning curve in LAG.
Methods
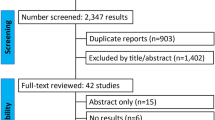
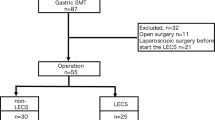
Cumulative sum method was used to analyze outcomes of 109 patients undergoing LAG for EGC by one surgeon over a two year period; the influence of patient selection was evaluated. Target failure rate was set at 10%, with failure defined as open conversion, mortality, major morbidity, residual tumor, or inappropriate lymphadenectomy.
Results
There were 19 failures-fourteen performance and five oncologic. The learning curve, which displayed a slight rising trend and three phases was achieved after 40 cases with selected patients; it was broken, however, by the introduction of advanced procedures and unselected patients.
Conclusions
Advanced procedures and broad indications in LAG should be delayed until a learning curve is completed under the target failure rate.




Similar content being viewed by others
References
Buchmann P, Dincler S (2005) Learning curve–calculation and value in laparoscopic surgery. Ther Umsch 62(2): 69–75
Diggle P (1990) Time series: a biostatistical introduction Oxford University Press, London
Dincler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P (2003) Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectu 46(10): 1371–1378
Forbes TL (2005) A cumulative analysis of an individual surgeon’s early experience with elective open abdominal arotic aneurysm repair. Am J Surg 189(4): 469–473
Grunkemeier GL, Wu YX, Furnary AP (2003) Cumulative sum techniques for assessing surgical results. Ann Thorac Surg 76(3): 63–667
Hayashi H, Ochiai T, Shimada H, Gunji Y (2005) Prospective randomized study of open versus laparoscopy-assisted distal gastrectomy with extraperigastric lymph node dissection for early gastric cancer. Surg Endosc 19:1172–6
Hermanek P, Wiebelt H, Staimmer D, Riedl S. (1995) Prognostic factors of rectum carcinoma: experience of the German Multicentre Study SGCRC. German Study Group Colo-Rectal Carcinoma Tumori 81(3 Suppl):60–4
Japanese Cancer Association (2004) Gastric cancer treatment guideline 2nd ed. Kanehara, Tokyo
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4: 146–148
Kitano S, Shiraish N (2004) Current status of laparoscopic gastrectomy for cancer in Japan. Surg Endosc 18: 182–185
Lim TO, Soraya A, Ding LM, Morad Z (2002) Assessing doctors’ competence: application of CUSUM technique in monitoring doctors’ performance. Int J Qual Health Care 14(3): 251–258
Maruyama K, Sasako M, Kinoshita T, Sano T, Katai H, Hada M, Schmit-Matthiesen A, Dalh O (1998) Should systemic lymph node dissection be recommended for gastric cancer?. Eur J Cancer 34: 1480–1483
Noshiro H, Nagai E, Shimizu S, Uchiyama A, Tanaka M (2005) Laaroscopically assisted distal gastrectomy with standard radical lymph node dissection for gastric cancer. Surg Endosc 19:1592–6
Novick RJ, Stitt LW (1999) The learning curve of an academic cardiac surgeon: Use of the CUSUM method. J Card Surg 14: 312–320
Oka M, Maeda Y, Ueno T, Iizuka N, Abe T, Yamamoto K, Ogura Y, Masaki Y, Suzuki T (1995) A hemidouble stapling method to creat the Billroth-I anastomosis using a detachable device. J Am Coll Surg 181:366–368
Rosin D, Brasesco O, Rosenthal RJ (2001) Laparoscopy for gastric tumors. Surg Oncol Clin N Am 10: 511–529
Sayegh ME, Sano T, Dexter S, Katai H, Fukagawa T, Sasako M (2004) TNM and Japanese staging systems for gastric cancer: how do they coexist? Gastric Cancer 7(3): 140–148
Shimizu S, Uchiyama A, Mizumoto K, Morisaki T, Nakamura K, Shimura H, Tanaka M (2000) Laparoscopically assisted distal gastrectomy for early gastric cancer: is it superior to open surgery?. Surg Endosc 14: 27–31
Williams SM, Parry BR, Schlup MMT (1992) Quality control: An application of the CUSUM. BMJ 304: 1359–1361
Yano H, Monden T, Kinuta M, Nakano Y, Tono T, Matsui S, Iwazawa T, Kanoh T, Katsushima S (2001) The usefulness of laparoscopy-assisted distal gastrectomy in comparison with that of open distal gastrectomy for early gastric cancer. Gastric cancer 4: 93–97
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Calculation of CUSUM Boundary Lines [9, 14, 19]
-
p0 = target failure rate = 0.10
-
p1 = alternative failure rate at which one wishes to be alerted if failure rate rose to this level = 0.20
-
α = type I (false alarm) error rate — probability of incorrectly rejecting the target p0 in favor of the alternative p1 (0.05 for 95% “alarm” line, 0.20 for 80% “alert” line).
-
β = type II (false reassurance) error rate — probability of incorrectly rejecting the alternative p1 in favor of the target p0 = 0.20.
-
a = ln([1 − β]/α)
-
b = ln([1 − α]/β)
-
P = ln(p1/p0)
-
Q = ln([1 − p0)/(1 − p1])
-
s = Q/(P + Q)
-
n = number of operations (horizontal axis)
-
X = accumulated number of failures after n operations (vertical axis)
-
Lower (“reassurance”) boundary line: X0 = ns − b/(P + Q)
-
Upper (“alert” or “alarm”) boundary line: X1 = ns − a/(P + Q)
Rights and permissions
About this article
Cite this article
Jin, SH., Kim, DY., Kim, H. et al. Multidimensional learning curve in laparoscopy-assisted gastrectomy for early gastric cancer. Surg Endosc 21, 28–33 (2007). https://doi.org/10.1007/s00464-005-0634-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0634-3