Abstract
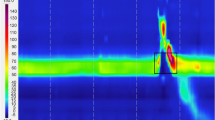
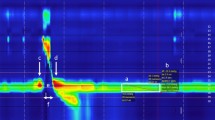
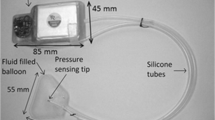
Resting pressure at the upper oesophageal sphincter (UOS) has been reported to be susceptible to factors such as emotional stress or respiration. This exploratory study investigated the potential for behavioural modulation of UOS resting pressure in healthy adults to increase our understanding of volitional control of UOS pressure, and the potential development of rehabilitation approaches. Six healthy adults were seen one hour daily for two weeks (10 days) and for one post-training session after a training break of two weeks. Manipulation of UOS resting pressure was practised during a protocol of alternating increased and decreased pressure. A high-resolution manometry contour plot was used as a biofeedback modality. Participants were asked to explore how to achieve warmer and cooler colours (pressure increase and decrease, respectively) at the UOS resting pressure band, without changing head position or manipulating activity of other muscles. Performance was analysed prior to training start and following daily training. Participants were able to increase resting pressure following one week of practice; however, there was no evidence for purposeful pressure decrease. The increased resting pressure achieved by participants indicates a capacity for purposeful pressure modulation given intensive biofeedback training. The lack of volitional reduction in pressure may be explained by sustained pressure generation due to the intrinsic muscular characteristics of the UOS and a flooring effect in healthy subjects, in whom physiology mandates a minimum degree of resting pressure to fulfil the barrier function. Distention caused by the presence of the intraluminal catheter cannot be ruled out.



Similar content being viewed by others
References
Lang IM. Development, anatomy, and physiology of the upper esophageal sphincter and pharyngoesophageal junction. In: Shaker R, Belafsky P, Postma G, Easterling C, editors. Principles of deglutition: A multidisciplinary text for swallowing and its disorders. New York: Springer; 2013. p. 235–255. https://doi.org/10.1007/978-1-4614-3794-9.
Nilsson ME, Isberg A, Schiratzki H. The location of the upper oesophageal sphincter and its behaviour during bolus propagation-a simultaneous cineradiographic and manometric investigation. Clin Otolaryngol Allied Sci. 1989;14(1):61–5.
Halum SL, Shemirani NL, Merati AL, Jaradeh S, Toohill RJ. Electromyography findings of the cricopharyngeus in association with ipsilateral pharyngeal and laryngeal muscles. Ann Otol Rhinol Laryngol. 2006;115(4):312–6. https://doi.org/10.1177/000348940611500411.
Singh S, Hamdy S. The upper oesophageal sphincter. Neurogastroenterol Motil. 2005;17:3–12. https://doi.org/10.1111/j.1365-2982.2005.00662.x.
Kahrilas PJ, Dodds WJ, Dent J, Haebrle B, Hogan WJ, Arndorfer RC. Effect of sleep, spontaneous gastroesophageal reflux, and a meal on upper esophageal sphincter pressure in normal human volunteers. Gastroenterology. 1987;92(2):466–71.
Eastwood PR, Katagiri S, Shepherd KL, Hillman DR. Modulation of upper and lower esophageal sphincter tone during sleep. Sleep Med. 2007;8(2):135–43. https://doi.org/10.1016/j.sleep.2006.08.016.
Perera L, Kern M, Hofmann C, Tatro L, Chai K, Kuribayashi S, Lawal A, Shaker R. Manometric evidence for a phonation-induced UES contractile reflex. Am J Physiol Gastrointest Liver Physiol. 2008;294(4):G885–891. https://doi.org/10.1152/ajpgi.00470.2007.
DiRe C, Shi G, Manka M, Kahrilas PJ. Manometric characteristics of the upper esophageal sphincter recorded with a microsleeve. Am J Gastroenterol. 2001;96(5):1383–9. https://doi.org/10.1111/j.1572-0241.2001.03793.x.
Cook IJ, Dent J, Shannon S, Collins SM. Measurement of upper esophageal sphincter pressure. Effect of acute emotional stress. Gastroenterology. 1987;93(3):526–32.
Shaker R, Ren J, Xie P, Lang IM, Bardan E, Sui Z. Characterization of the pharyngo-UES contractile reflex in humans. Am J Physiol. 1997;273(4 Pt 1):G854–858.
Lang IM, Shaker R. Anatomy and physiology of the upper esophageal sphincter. Am J Med. 1997;103(5A):50–5.
Miller AJ. The neuroscientific principles of swallowing and dysphagia. San Diego: Singular Publishing Group; 1999.
Ertekin C, Turman B, Tarlaci S, Celik M, Aydogdu I, Secil Y, Kiylioglu N. Cricopharyngeal sphincter muscle responses to transcranial magnetic stimulation in normal subjects and in patients with dysphagia. Clin Neurophysiol. 2001;112(1):86–94. https://doi.org/10.1016/S1388-2457(00)00504-6.
Ertekin C, Aydogdu I. Electromyography of human cricopharyngeal muscle of the upper esophageal sphincter. Muscle Nerve. 2002;26(6):729–39. https://doi.org/10.1002/mus.10267.
Nativ-Zeltzer N, Belafsky PC, Bayoumi A, Kuhn MA. Volitional control of the upper esophageal sphincter with high-resolution manometry driven biofeedback. Laryngoscope Investig Otolaryngol. 2019;4(2):264–8. https://doi.org/10.1002/lio2.255.
Peng L, Patel A, Kushnir V, Gyawali CP. Assessment of upper esophageal sphincter function on high-resolution manometry: identification of predictors of globus symptoms. J Clin Gastroenterol. 2015;49(2):95–100. https://doi.org/10.1097/MCG.0000000000000078.
Schindler A, Mozzanica F, Alfonsi E, Ginocchio D, Rieder E, Lenglinger J, Schoppmann SF, Scharitzer M, Pokieser P, Kuribayashi S, Kawamura O, Kusano M, Zelenik K. Upper esophageal sphincter dysfunction: Diverticula-globus pharyngeus. Ann N Y Acad Sci. 2013;1300(1):250–60. https://doi.org/10.1111/nyas.12251.
Tokashiki R, Funato N, Suzuki M. Globus sensation and increased upper esophageal sphincter pressure with distal esophageal acid perfusion. Eur Arch Otorhinolaryngol. 2010;267(5):737–41. https://doi.org/10.1007/s00405-009-1134-1.
Kiebles JL, Kwiatek MA, Pandolfino JE, Kahrilas PJ, Keefer L. Do patients with globus sensation respond to hypnotically assisted relaxation therapy? A case series report. Dis Esophagus. 2010;23(7):545–53. https://doi.org/10.1111/j.1442-2050.2010.01064.x.
Lamvik K, Jones R, Sauer S, Erfmann K, Huckabee ML. The capacity for volitional control of pharyngeal swallowing in healthy adults. Physiol Behav. 2015;152(Pt A):257–63. https://doi.org/10.1016/j.physbeh.2015.09.026.
Knigge MA, Thibeault S, McCulloch TM. Implementation of high-resolution manometry in the clinical practice of speech language pathology. Dysphagia. 2014;29(1):2–16. https://doi.org/10.1007/s00455-013-9494-5.
Guiu Hernandez E, Gozdzikowska K, Apperley O, Huckabee M-L. Effect of topical nasal anesthetic on swallowing in healthy adults: a double-blind, high-resolution manometry study. Laryngoscope. 2017;128(6):1335–9. https://doi.org/10.1002/lary.26996.
Nelson LA. The role of biofeedback in stroke rehabilitation: past and future directions. Top Stroke Rehabil. 2007;14(4):59–66. https://doi.org/10.1310/tsr1404-59.
Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–40. https://doi.org/10.1002/1098-240X(200008)23:4<334:AID-NUR9>3.0.CO;2-G.
Neergaard MA, Olesen F, Andersen RS, Sondergaard J. Qualitative description—the poor cousin of health research? BMC Med Res Methodol. 2009;9(1):52. https://doi.org/10.1186/1471-2288-9-52.
Lamvik K, Guiu Hernandez E, Jones R, Huckabee ML. Characterization and correction of pressure drift in the ManoScan™ high-resolution manometry system: in vitro and in vivo. Neurogastroenterol Motil. 2016;28(5):732–42. https://doi.org/10.1111/nmo.12770.
Core Team R. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2016.
Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–8. https://doi.org/10.1037/0033-2909.86.2.420.
Portney LG, Watkins MP. Foundations of clinical research. Applications to practice. 3rd ed. London: Pearson Education; 2009.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using {lme4}. J Stat Softw. 2015;67:1–48. https://doi.org/10.18637/jss.v067.i01.
Jungheim M, Miller S, Kühn D, Schwemmle C, Schneider JP, Ochs M, Ptok M. Physiology of the upper esophageal sphincter. HNO. 2014;62(6):457–68. https://doi.org/10.1007/s00106-014-2846-0.
Given Imaging (2016) ManoScanTM user manual: Modular cart system A120, A200, A300, and A400 (DOC1963-04)
Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. Br Med J. 2000;320(7227):114–6. https://doi.org/10.1136/bmj.320.7227.114.
Jungheim M, Miller S, Kühn D, Schwemmle C, Schneider JP, Ochs M, Ptok M. Anatomy of the upper esophageal sphincter. HNO. 2014;62(5):385–94. https://doi.org/10.1007/s00106-014-2845-1.
Jungheim M, Schubert C, Miller S, Ptok M. Normwerte für die Hochauflösungsmanometrie von Pharynx und oberem Ösophagussphinkter (Normative data of pharyngeal and upper esophageal sphincter high resolution manometry). Laryngorhinootologie. 2015;94(09):601–8. https://doi.org/10.1055/s-0034-1395532.
Acknowledgements
Reliability data were extracted by Susanne Ebert.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Winiker, K., Gozdzikowska, K., Guiu Hernandez, E. et al. Potential for Volitional Control of Resting Pressure at the Upper Oesophageal Sphincter in Healthy Individuals. Dysphagia 36, 374–383 (2021). https://doi.org/10.1007/s00455-020-10146-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10146-7