Abstract
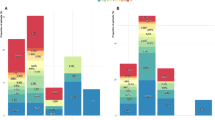
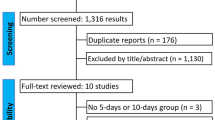
The optimal duration of antibiotic treatment for the most common bacterial meningitis etiologies in the pediatric population, namely Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis, is not well-established in the literature. Therefore, we aimed to perform an updated meta-analysis comparing shorter versus longer antibiotic treatment in children with meningitis. PubMed, EMBASE, and Cochrane databases were searched for randomized controlled trials (RCTs) that compared shorter (up to 7 days) versus longer (10 days or double the days of the equivalent short course) duration of antibiotic treatment in children with meningitis and reported the outcomes of treatment failure, death, neurologic sequelae, non-neurologic complications, hearing impairment, nosocomial infection, and relapse. Heterogeneity was examined with I2 statistics. RevMan 5.4.1 was used for statistical analysis and RoB-2 (Cochrane) for risk of bias assessment. Of 684 search results, 6 RCTs were included, with a cohort of 1333 children ages 3 weeks to 15.5 years, of whom 49.51% underwent a short antibiotic course. All RCTs included monotherapy with ceftriaxone, except one, which added vancomycin as well. No differences were found comparing the short and long duration of therapy concerning treatment failure, relapse, mortality, and neurologic complications at discharge and at follow-up.
Conclusion: Because no statistically significant differences were found between groups for the analyzed outcomes, the results of this meta-analysis support shorter therapy. However, generalizing these results to complicated meningitis and infections caused by other pathogens should be made with caution. (PROSPERO identifier: CRD42022369843).
What is Known: • Current recommendations on the duration of antibiotic therapy for bacterial meningitis are mostly based on clinical practice. • Defining an optimal duration of antibiotic therapy is essential for antimicrobial stewardship achievement, improving patient outcomes, and minimizing adverse effects. | |
What is New: • There are no differences between shorter versus longer antibiotic treatment duration in regard to treatment failure, relapse, mortality, neurologic complications, and hearing impairment at discharge and at follow-up. |





Similar content being viewed by others
Data availability
Because this meta-analysis was based on data extracted from previously published research, all the data and study materials are available in the public domain. The authors do not have access to patient-level data of the individual studies. Researchers with an interest in individual-level data from the studies included in this meta-analysis are encouraged to contact the corresponding author from each study for such requests.
Abbreviations
- AAP:
-
American Academy of Pediatrics
- CI:
-
Confidence Interval
- CPS:
-
Canadian Paediatric Society
- CSF:
-
Cerebrospinal Fluid
- GRADE:
-
Grading of Recommendations, Assessment, Development and Evaluation
- IDSA:
-
Infectious Diseases Society of America
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- RCT:
-
Randomized Controlled Trial
- RoB-2:
-
Cochrane’s Risk of Bias 2 software
- RR:
-
Risk Ratio
- WHO:
-
World Health Organization
References
Kim KS (2020) Investigating bacterial penetration of the blood–brain barrier for the pathogenesis, prevention, and therapy of bacterial meningitis. ACS Infect Dis 6(1):34–42
Doran KS, Fulde M, Gratz N, Kim BJ, Nau R, Prasadarao N et al (2016) Host–pathogen interactions in bacterial meningitis. Acta Neuropathol (Berl) 131(2):185–209
Prober CG (2008) Nelson’s textbook of pediatrics, 18th edition, 18th edn. Elsevier, New Delhi
World Health Organization (2021) Defeating meningitis by 2030: a global roadmap. Geneva. Licence: CC BY-NC-SA 3.0 IGO. Available from https://www.who.int/publications/i/item/9789240026407
Finberg RW, Moellering RC, Tally FP, Craig WA, Pankey GA, Dellinger EP et al (2004) The importance of bactericidal drugs: future directions in infectious disease. Clin Infect Dis 39(9):1314–1320
Friedland IR, Paris M, Ehrett S, Hickey S, Olsen K, McCracken GH (1993) Evaluation of antimicrobial regimens for treatment of experimental penicillin- and cephalosporin-resistant pneumococcal meningitis. Antimicrob Agents Chemother 37(8):1630–1636
Del Rio M, McCracken GH, Nelson JD, Chrane D, Shelton S (1982) Pharmacokinetics and cerebrospinal fluid bactericidal activity of ceftriaxone in the treatment of pediatric patients with bacterial meningitis. Antimicrob Agents Chemother 22(4):622–627
Society CP. Guidelines for the management of suspected and confirmed bacterial meningitis in Canadian children older than 2 months of age | Canadian Paediatric Society [Internet]. [cited 2022 Dec 23]. Available from: https://cps.ca/documents/position/management-of-bacterial-meningitis
American Academy of Pediatrics. Haemophilus influenzae infections. In: Red Book: 20 21–2024 Report of the Committee on Infectious Diseases. 32nd ed. Itasca, IL; p. 345
American Academy of Pediatrics. Meningococcal infections. In: Red Book: 2021–2024 Report of the Committee on Infectious Diseases. 32nd ed. Itasca, IL; 2021. p. 519
World Health Organization (2019) Defeating meningitis by 2030: a baseline situation analysis. Geneva. Available from https://www.who.int/immunization/research/BSA_20feb2019.pdf?ua=1
Dellit TH, Owens RC, McGowan JE, Gerding DN, Weinstein RA, Burke JP et al (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for Developing an Institutional Program to Enhance Antimicrobial Stewardship. Clin Infect Dis 44(2):159–177
Lin T, Chrane D, Nelson J, McCracken G (1985) Seven days of ceftriaxone therapy is as effective as ten days’ treatment for bacterial meningitis. JAMA 253(24):3559–3563
Martin E, Hohl P, Guggi T, Kayser F, Fernex M (1990) Short course single daily ceftriaxone monotherapy for acute bacterial meningitis in children: results of a Swiss multicenter study. Part I: clinical results. Infection 18(2):70–77
Molyneux E, Nizami S, Saha S, Huu K, Azam M, Bhutta Z et al (2011) 5 versus 10 days of treatment with ceftriaxone for bacterial meningitis in children: a double-blind randomised equivalence study. Lancet Lond Engl 377(9780):1837–1845
Kavaliotis J, Manios S, Kansouzidou A, Danielidis V (1989) Treatment of childhood bacterial meningitis with ceftriaxone once daily: open, prospective, randomized, comparative study of short-course versus standard-length therapy. Chemotherapy 35(4):296–303
Singhi P, Kaushal M, Singhi S, Ray P (2002) Seven days vs. 10 days ceftriaxone therapy in bacterial meningitis. J Trop Pediatr 48(5):273–279
Vaswani N, Gupta N, Yadav R, Nadda A (2021) Seven versus ten days antibiotics course for acute pyogenic meningitis in children: a randomized controlled trial. Indian J Pediatr 88(3):246–251
Roine I, Ledermann W, Foncea LM, Banfi A, Cohen J, Peltola H (2000) Randomized trial of four vs. seven days of ceftriaxone treatment for bacterial meningitis in children with rapid initial recovery. Pediatr Infect Dis J 19(3):219–22
Chandran A, Herbert H, Misurski D, Santosham M (2011) Long-term sequelae of childhood bacterial meningitis: an underappreciated problem. Pediatr Infect Dis J 30(1). Available from: https://journals.lww.com/pidj/Fulltext/2011/01000/Long_term_Sequelae_of_Childhood_Bacterial.4.aspx
Karageorgopoulos DE, Valkimadi PE, Kapaskelis A, Rafailidis PI, Falagas ME (2009) Short versus long duration of antibiotic therapy for bacterial meningitis: a meta-analysis of randomised controlled trials in children. Arch Dis Child 94(8):607–614
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 28(366):l4898
Schünemann H, Brożek J, Guyatt G, Oxman A (2013) GRADE handbook for grading quality of evidence and strength of recommendations. Available from: https://guidelinedevelopment.org/handbook.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29(372):n71
Review Manager (RevMan). Version 5.4.1. The Cochrane Collaboration, (2020). Available at revman.cochrane.org
Page M, Higgins J, Sterne J (2022). Chapter 13: Assessing risk of bias due to missing results in a synthesis [Internet]. [cited 2022 Dec 23]. Available from: https://training.cochrane.org/handbook/current/chapter-13
Mathur N, Kharod P, Kumar S (2015) Evaluation of duration of antibiotic therapy in neonatal bacterial meningitis: a randomized controlled trial. J Trop Pediatr 61(2):119–125
O’Neill P, Heath ClarkW Jr, Shann F, Henry David A, Hilton-Jones D, Squier MV et al (1993) MENINGITIS: How long to treat bacterial meningitis. Lancet 341(8844):530
Eisen DP, Hamilton E, Bodilsen J, Køster-Rasmussen R, Stockdale AJ, Miner J et al (2022) Longer than 2 hours to antibiotics is associated with doubling of mortality in a multinational community-acquired bacterial meningitis cohort. Sci Rep 12(1):672
Chaudhuri A, Martin PM, Kennedy PGE, Andrew Seaton R, Portegies P, Bojar M et al (2008) EFNS guideline on the management of community-acquired bacterial meningitis: report of an EFNS Task Force on acute bacterial meningitis in older children and adults. Eur J Neurol 15(7):649–659
Haque M, Sartelli M, McKimm J, Abu Bakar MB (2018) Health care-associated infections: an overview. Infect Drug Resist 11:2321–2333
Nadeem SF et al (2018) Antimicrobial resistance: more than 70 years of war between humans and bacteria. Crit Rev Microbiol 46:578–599
Butler JC et al (1996) The continued emergence of drug-resistant Streptococcus pneumoniae in the United States: an update from the Centers for Disease Control and Prevention’s Pneumococcal Sentinel Surveillance System. J Infect Dis 174:986–993
Glimåker M, Johansson B, Grindborg Ö, Bottai M, Lindquist L, Sjölin J (2015) Adult bacterial meningitis: earlier treatment and improved outcome following guideline revision promoting prompt lumbar puncture. Clin Infect Dis Off Publ Infect Dis Soc Am 60(8):1162–1169
Køster-Rasmussen R, Korshin A, Meyer CN (2008) Antibiotic treatment delay and outcome in acute bacterial meningitis. J Infect 57(6):449–454
Vasilopoulou VA, Karanika M, Theodoridou K, Katsioulis AT, Theodoridou MN, Hadjichristodoulou CS (2011) Prognostic factors related to sequelae in childhood bacterial meningitis: data from a Greek meningitis registry. BMC Infect Dis 11(1):214
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Maria Carrijo Cunha Camara, Renan Yuji Ura Sudo and Sofia Vezzani Kieling. The first draft of the manuscript was written by Renan Yuji Ura Sudo, Maria Carrijo Cunha Camara, Sofia Vezzani Kieling, Isabela Reis Marques, and Yasmin Luz Lima de Mesquita. All authors critically reviewed previous versions of the manuscript. All authors read and approved the final manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sudo, R.Y.U., Câmara, M.C.C., Kieling, S.V. et al. Shorter versus longer duration of antibiotic treatment in children with bacterial meningitis: a systematic review and meta-analysis. Eur J Pediatr 183, 61–71 (2024). https://doi.org/10.1007/s00431-023-05275-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05275-8