Abstract
This narrative review aims to present an overview of the COVID-19 pandemic’s effects on the landscape of pediatric infectious diseases. While COVID-19 generally results in mild symptoms and a favorable prognosis in children, the pandemic brought forth significant consequences. These included persistent symptoms among infected children (“long COVID”), a profound transformation in healthcare utilization (notably through the widespread adoption of telemedicine), and the implementation of optimization strategies within healthcare settings. Furthermore, the pandemic resulted in alterations in the circulation patterns of respiratory pathogens, including influenza, RSV, and Streptococcus pneumoniae. The possible reasons for those changes are discussed in this review. COVID-19 effect was not limited to respiratory infectious diseases, as other diseases, including urinary tract and gastrointestinal infections, have displayed decreased transmission rates, likely attributable to heightened hygiene measures and shifts in care-seeking behaviors. Finally, the disruption of routine childhood vaccination programs has resulted in reduced immunization coverage and an upsurge in vaccine hesitancy. In addition, the pandemic was associated with issues of antibiotic misuse and over-prescription.
Conclusion: In conclusion, the COVID-19 pandemic has left a profound and multifaceted impact on the landscape of pediatric infectious diseases, ranging from the emergence of “long COVID” in children to significant changes in healthcare delivery, altered circulation patterns of various pathogens, and concerning disruptions in vaccination programs and antibiotic usage.
What is Known: • COVID-19 usually presents with mild symptoms in children, although severe and late manifestations are possible. • The pandemic resulted in a dramatically increased use of health care services, as well as alterations in the circulation patterns of respiratory pathogens, decreased rates of other, non-respiratory, infections, disruption of routine childhood vaccination programs, and antibiotic misuse. | |
What is New: • Possible strategies to tackle future outbreaks are presented, including changes in health care services utilization, implementation of updated vaccine programs and antibiotic stewardship protocols. • The decline in RSV and influenza circulation during COVID-19 was probably not primarily related to NPI measures, and rather related to other, non-NPI measures implementation, including specific pathogen-host interactions on the level of the biological niche (the nasopharynx). |
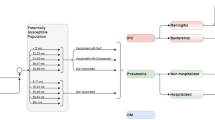
Graphical Abstract

Similar content being viewed by others
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- SARS‑CoV‑2:
-
Severe acute respiratory syndrome coronavirus 2
- MIS-C:
-
Multisystem inflammatory syndrome in children
- HPV:
-
Human papillomavirus
- LMIC:
-
Low-middle-income countries
- AMR:
-
Antimicrobial resistance
References
Lenharo M (2023) WHO declares end to COVID-19’s emergency phase. Nature. https://doi.org/10.1038/d41586-023-01559-z
Van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ et al (2020) Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 4:460–471. https://doi.org/10.1038/s41562-020-0884-z
Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S (2020) Epidemiology of COVID-19 among children in China. Pediatrics 145 https://doi.org/10.1542/peds.2020-0702
Jarovsky D, de Freitas FG, Zampol RM, de Oliveira TA, Farias CGA, da Silva D, Cavalcante DTG, Nery SB, de Moraes JC, de Oliveira FI, Almeida FJ, Sáfadi MAP (2023) Characteristics and clinical outcomes of COVID-19 in children: a hospital-based surveillance study in Latin America’s hardest-hit city. IJID Reg 7:52–62. https://doi.org/10.1016/j.ijregi.2022.12.003
Nikolopoulou GB, Maltezou HC (2022) COVID-19 in children: where do we stand? Arch Med Res 53:1–8. https://doi.org/10.1016/j.arcmed.2021.07.002
Tagarro A, Epalza C, Santos M, Sanz-Santaeufemia FJ, Otheo E, Moraleda C, Calvo C (2020) Screening and severity of coronavirus disease 2019 (COVID-19) in children in Madrid. JAMA Pediatr, Spain. https://doi.org/10.1001/jamapediatrics.2020.1346
Zachariah P, Johnson CL, Halabi KC, Ahn D, Sen AI, Fischer A, Banker SL, Giordano M, Manice CS, Diamond R, Sewell TB, Schweickert AJ, Babineau JR, Carter RC, Fenster DB, Orange JS, McCann TA, Kernie SG, Saiman L, Columbia Pediatric C-MG (2020) Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a children’s hospital in New York City, New York. JAMA Pediatr 174:e202430. https://doi.org/10.1001/jamapediatrics.2020.2430
Zimmermann P, Curtis N (2020) Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J 39:355–368. https://doi.org/10.1097/INF.0000000000002660
Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, Perlini S, Rovida F, Baldanti F, Marseglia GL (2020) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr 174:882–889. https://doi.org/10.1001/jamapediatrics.2020.1467
Kim L, Whitaker M, O'Halloran A, Kambhampati A, Chai SJ, Reingold A, Armistead I, et al. (2020) Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed COVID-19 - COVID-NET, 14 States, March 1-July 25, 2020. MMWR Morb Mortal Wkly Rep 69:1081–1088. https://doi.org/10.15585/mmwr.mm6932e3
Mehta NS, Mytton OT, Mullins EWS, Fowler TA, Falconer CL, Murphy OB, Langenberg C, Jayatunga WJP, Eddy DH, Nguyen-Van-Tam JS (2020) SARS-CoV-2 (COVID-19): what do we know about children? A systematic review. Clin Infect Dis 71:2469–2479. https://doi.org/10.1093/cid/ciaa556
Nachega JB, Sam-Agudu NA, Machekano RN, Rabie H, van der Zalm MM, Redfern A, Dramowski A et al (2022) Assessment of clinical outcomes among children and adolescents hospitalized with COVID-19 in 6 sub-Saharan African countries. JAMA Pediatr 176:e216436. https://doi.org/10.1001/jamapediatrics.2021.6436
Ben-Shimol S, Livni G, Megged O, Greenberg D, Danino D, Youngster I, Shachor-Meyouhas Y et al (2021) COVID-19 in a subset of hospitalized children in Israel. J Pediatric Infect Dis Soc 10:757–765. https://doi.org/10.1093/jpids/piab035
Chow EJ, Englund JA (2022) Severe acute respiratory syndrome coronavirus 2 infections in children. Infect Dis Clin North Am 36:435–479. https://doi.org/10.1016/j.idc.2022.01.005
Yarden Bilavski H, Balanson S, Damouni Shalabi R, Dabaja-Younis H, Grisaru-Soen G, Youngster I, Glikman D, Ben Shimol S, Somech E, Tasher D, Stein M, Gottesmanm G, Livni G, Megged O (2021) Benign course and clinical features of COVID-19 in hospitalised febrile infants up to 60 days old. Acta Paediatr 110:2790–2795. https://doi.org/10.1111/apa.15993
Chua PEY, Shah SU, Gui H, Koh J, Somani J, Pang J (2021) Epidemiological and clinical characteristics of non-severe and severe pediatric and adult COVID-19 patients across different geographical regions in the early phase of pandemic: a systematic review and meta-analysis of observational studies. J Investig Med 69:1287–1296. https://doi.org/10.1136/jim-2021-001858
Lopez-Leon S, Wegman-Ostrosky T, Ayuzo Del Valle NC, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, Villapol S (2022) Long-COVID in children and adolescents: a systematic review and meta-analyses. Sci Rep 12:9950. https://doi.org/10.1038/s41598-022-13495-5
Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, Hollings S, Roebuck C, Gale CP, Mamas MA, Deanfield JE, de Belder MA, Luescher TF, Denwood T, Landray MJ, Emberson JR, Collins R, Morris EJA, Casadei B, Baigent C (2020) COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 396:381–389. https://doi.org/10.1016/S0140-6736(20)31356-8
Moynihan R, Johansson M, Maybee A, Lang E, Legare F (2020) COVID-19: an opportunity to reduce unnecessary healthcare. BMJ 370:m2752. https://doi.org/10.1136/bmj.m2752
Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, Jones M, Kitchener E, Fox M, Johansson M, Lang E, Duggan A, Scott I, Albarqouni L (2021) Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 11:e045343. https://doi.org/10.1136/bmjopen-2020-045343
Mogharab V, Ostovar M, Ruszkowski J, Hussain SZM, Shrestha R, Yaqoob U, Aryanpoor P et al (2022) Global burden of the COVID-19 associated patient-related delay in emergency healthcare: a panel of systematic review and meta-analyses. Global Health 18:58. https://doi.org/10.1186/s12992-022-00836-2
Khalil-Khan A, Khan MA (2023) The impact of COVID-19 on primary care: a scoping review. Cureus 15:e33241. https://doi.org/10.7759/cureus.33241
Pandita KK, Noor T, Sahoo SK (2022) COVID-19 pandemic: hospital preparedness in a tertiary care hospital in North East India. J Family Med Prim Care 11:2877–2883. https://doi.org/10.4103/jfmpc.jfmpc_1571_21
Serlachius A, Badawy SM, Thabrew H (2020) Psychosocial challenges and opportunities for youth with chronic health conditions during the COVID-19 pandemic. JMIR Pediatr Parent 3:e23057. https://doi.org/10.2196/23057
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, Chua A, Verma M, Shrestha P, Singh S, Perez T, Tan SM, Bartos M, Mabuchi S, Bonk M, McNab C, Werner GK, Panjabi R, Nordstrom A, Legido-Quigley H (2021) Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med 27:964–980. https://doi.org/10.1038/s41591-021-01381-y
Mann DM, Chen J, Chunara R, Testa PA, Nov O (2020) COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc 27:1132–1135. https://doi.org/10.1093/jamia/ocaa072
Arsenault C, Gage A, Kim MK, Kapoor NR, Akweongo P, Amponsah F, Aryal A et al (2022) COVID-19 and resilience of healthcare systems in ten countries. Nat Med 28:1314–1324. https://doi.org/10.1038/s41591-022-01750-1
Komori A, Mori H, Naito T (2022) The impact of the COVID-19 pandemic on other infections differs by their route of transmission: a retrospective, observational study in Japan. J Infect Chemother 28:1700–1703. https://doi.org/10.1016/j.jiac.2022.08.022
Toelen J, Ritz N, de Winter JP (2021) Changes in pediatric infections during the COVID-19 pandemic: ‘a quarantrend for coronials’? Eur J Pediatr 180:1965–1967. https://doi.org/10.1007/s00431-021-03986-4
Van Brusselen D, De Troeyer K, Ter Haar E, Vander Auwera A, Poschet K, Van Nuijs S, Bael A, Stobbelaar K, Verhulst S, Van Herendael B, Willems P, Vermeulen M, De Man J, Bossuyt N, Vanden Driessche K (2021) Bronchiolitis in COVID-19 times: a nearly absent disease? Eur J Pediatr 180:1969–1973. https://doi.org/10.1007/s00431-021-03968-6
Broberg EK, Waris M, Johansen K, Snacken R, Penttinen P, European Influenza Surveillance N (2018) Seasonality and geographical spread of respiratory syncytial virus epidemics in 15 European countries, 2010 to 2016. Euro Surveill 23 https://doi.org/10.2807/1560-7917.ES.2018.23.5.17-00284
Kenah E, Chao DL, Matrajt L, Halloran ME, Longini IM, Jr. (2011) The global transmission and control of influenza. PLoS One 6:e19515. https://doi.org/10.1371/journal.pone.0019515
Olsen SJ, Winn AK, Budd AP, Prill MM, Steel J, Midgley CM, Kniss K, et al. (2021) Changes in influenza and other respiratory virus activity during the COVID-19 pandemic - United States, 2020–2021. MMWR Morb Mortal Wkly Rep 70:1013–1019. https://doi.org/10.15585/mmwr.mm7029a1
Danino D, Ben-Shimol S, van der Beek BA, Givon-Lavi N, Avni YS, Greenberg D, Weinberger DM, Dagan R (2022) Decline in pneumococcal disease in young children during the coronavirus disease 2019 (COVID-19) pandemic in israel associated with suppression of seasonal respiratory viruses, despite persistent pneumococcal carriage: a prospective cohort study. Clin Infect Dis 75:e1154–e1164. https://doi.org/10.1093/cid/ciab1014
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, Pastore YPA, Mu K, Rossi L, Sun K, Viboud C, Xiong X, Yu H, Halloran ME, Longini IM Jr, Vespignani A (2020) The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 368:395–400. https://doi.org/10.1126/science.aba9757
Heymann DL, Shindo N, Scientific WHO, Technical advisory group for infectious H, (2020) COVID-19: what is next for public health? Lancet 395:542–545. https://doi.org/10.1016/S0140-6736(20)30374-3
Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, Wesolowski A, Santillana M, Zhang C, Du X, Yu H, Tatem AJ (2020) Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 585:410–413. https://doi.org/10.1038/s41586-020-2293-x
Xiao J, Shiu EYC, Gao H, Wong JY, Fong MW, Ryu S, Cowling BJ (2020) Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-personal protective and environmental measures. Emerg Infect Dis 26:967–975. https://doi.org/10.3201/eid2605.190994
Dadras O, Alinaghi SAS, Karimi A, MohsseniPour M, Barzegary A, Vahedi F, Pashaei Z, Mirzapour P, Fakhfouri A, Zargari G, Saeidi S, Mojdeganlou H, Badri H, Qaderi K, Behnezhad F, Mehraeen E (2021) Effects of COVID-19 prevention procedures on other common infections: a systematic review. Eur J Med Res 26:67. https://doi.org/10.1186/s40001-021-00539-1
Khataee H, Scheuring I, Czirok A, Neufeld Z (2021) Effects of social distancing on the spreading of COVID-19 inferred from mobile phone data. Sci Rep 11:1661. https://doi.org/10.1038/s41598-021-81308-2
Chen X, Huang H, Ju J, Sun R, Zhang J (2022) Impact of vaccination on the COVID-19 pandemic in U.S. states. Sci Rep 12:1554. https://doi.org/10.1038/s41598-022-05498-z
Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC (2022) Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis 22:1293–1302. https://doi.org/10.1016/S1473-3099(22)00320-6
Chow EJ, Uyeki TM, Chu HY (2023) The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol 21:195–210. https://doi.org/10.1038/s41579-022-00807-9
Rubin R (2021) Influenza’s unprecedented low profile during COVID-19 pandemic leaves experts wondering what this flu season has in store. JAMA 326:899–900. https://doi.org/10.1001/jama.2021.14131
Jiang ML, Xu YP, Wu H, Zhu RN, Sun Y, Chen DM, Wang F, Zhou YT, Guo Q, Wu A, Qian Y, Zhou HY, Zhao LQ (2023) Changes in endemic patterns of respiratory syncytial virus infection in pediatric patients under the pressure of nonpharmaceutical interventions for COVID-19 in Beijing, China. J Med Virol 95:e28411. https://doi.org/10.1002/jmv.28411
Mosscrop LG, Williams TC, Tregoning JS (2022) Respiratory syncytial virus after the SARS-CoV-2 pandemic - what next? Nat Rev Immunol 22:589–590. https://doi.org/10.1038/s41577-022-00764-7
Kozlowski PA, Mantis NJ, Frey A (2022) Editorial: mucosal vaccination: strategies to induce and evaluate mucosal immunity. Front Immunol 13:905150. https://doi.org/10.3389/fimmu.2022.905150
Russell MW, Mestecky J (2022) Mucosal immunity: the missing link in comprehending SARS-CoV-2 infection and transmission. Front Immunol 13:957107. https://doi.org/10.3389/fimmu.2022.957107
Russell MW, Moldoveanu Z, Ogra PL, Mestecky J (2020) Mucosal immunity in COVID-19: a neglected but critical aspect of SARS-CoV-2 infection. Front Immunol 11:611337. https://doi.org/10.3389/fimmu.2020.611337
Lamers MM, Haagmans BL (2022) SARS-CoV-2 pathogenesis. Nat Rev Microbiol 20:270–284. https://doi.org/10.1038/s41579-022-00713-0
Kim HM, Lee EJ, Lee NJ, Woo SH, Kim JM, Rhee JE, Kim EJ (2021) Impact of coronavirus disease 2019 on respiratory surveillance and explanation of high detection rate of human rhinovirus during the pandemic in the Republic of Korea. Influenza Other Respir Viruses 15:721–731. https://doi.org/10.1111/irv.12894
Dagan R, van der Beek BA, Ben-Shimol S, Greenberg D, Shemer-Avni Y, Weinberger DM, Danino D (2023) The COVID-19 pandemic as an opportunity for unravelling the causative association between respiratory viruses and pneumococcus-associated disease in young children: a prospective study. EBioMedicine 90:104493. https://doi.org/10.1016/j.ebiom.2023.104493
Rybak A, Levy C, Angoulvant F, Auvrignon A, Gembara P, Danis K, Vaux S, Levy-Bruhl D, van der Werf S, Bechet S, Bonacorsi S, Assad Z, Lazzati A, Michel M, Kaguelidou F, Faye A, Cohen R, Varon E, Ouldali N (2022) Association of nonpharmaceutical interventions during the COVID-19 pandemic with invasive pneumococcal disease, pneumococcal carriage, and respiratory viral infections among children in France. JAMA Netw Open 5:e2218959. https://doi.org/10.1001/jamanetworkopen.2022.18959
McCullers JA (2006) Insights into the interaction between influenza virus and pneumococcus. Clin Microbiol Rev 19:571–582. https://doi.org/10.1128/CMR.00058-05
Kandeel A, Fahim M, Deghedy O, Roshdy WH, Khalifa MK, Shesheny RE, Kandeil A, Naguib A, Afifi S, Mohsen A, Abdelghaffar K (2023) Resurgence of influenza and respiratory syncytial virus in Egypt following two years of decline during the COVID-19 pandemic: outpatient clinic survey of infants and children, October 2022. BMC Public Health 23:1067. https://doi.org/10.1186/s12889-023-15880-9
Abu-Raya B, Vineta Paramo M, Reicherz F, Lavoie PM (2023) Why has the epidemiology of RSV changed during the COVID-19 pandemic? EClinicalMedicine 61:102089. https://doi.org/10.1016/j.eclinm.2023.102089
Cohen R, Ashman M, Taha MK, Varon E, Angoulvant F, Levy C, Rybak A, Ouldali N, Guiso N, Grimprel E (2021) Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now 51:418–423. https://doi.org/10.1016/j.idnow.2021.05.004
Treggiari D, Piubelli C, Formenti F, Silva R, Perandin F (2022) Resurgence of respiratory virus after relaxation of COVID-19 containment measures: a real-world data study from a regional hospital of Italy. Int J Microbiol 2022:4915678. https://doi.org/10.1155/2022/4915678
Bertran M, Amin-Chowdhury Z, Sheppard CL, Eletu S, Zamarreno DV, Ramsay ME, Litt D, Fry NK, Ladhani SN (2022) Increased incidence of invasive pneumococcal disease among children after COVID-19 pandemic, England. Emerg Infect Dis 28:1669–1672. https://doi.org/10.3201/eid2808.220304
Farahat RA, Shaheen N, Kundu M, Shaheen A, Abdelaal A (2022) The resurfacing of hand, foot, and mouth disease: are we on the verge of another epidemic? Ann Med Surg (Lond) 81:104419. https://doi.org/10.1016/j.amsu.2022.104419
Binns E, Koenraads M, Hristeva L, Flamant A, Baier-Grabner S, Loi M, Lempainen J, Osterheld E, Ramly B, Chakakala-Chaziya J, Enaganthi N, Simo Nebot S, Buonsenso D (2022) Influenza and respiratory syncytial virus during the COVID-19 pandemic: time for a new paradigm? Pediatr Pulmonol 57:38–42. https://doi.org/10.1002/ppul.25719
Dagan R, Danino D, Weinberger DM (2022) The pneumococcus-respiratory virus connection-unexpected lessons from the COVID-19 pandemic. JAMA Netw Open 5:e2218966. https://doi.org/10.1001/jamanetworkopen.2022.18966
Gilligan P (2022) Impact of COVID-19 on infectious diseases and public health. American Society for Microbiology
McBride DL (2021) Social Distancing for COVID-19 Decreased infectious diseases in children. J Pediatr Nurs 58:100–101. https://doi.org/10.1016/j.pedn.2021.02.018
Plantener E, Nanthan KR, Deding U, Damkjær M, Marmolin ES, Hansen LH, Petersen JJH, Pinilla R, Coia JE, Wolff DL, Song Z, Chen M (2023) Impact of COVID-19 restrictions on acute gastroenteritis in children: a regional, Danish, register-based study. Children 10:816
Kuitunen I, Artama M, Haapanen M, Renko M (2022) Urinary tract infections decreased in Finnish children during the COVID-19 pandemic. Eur J Pediatr 181:1979–1984. https://doi.org/10.1007/s00431-022-04389-9
Cesca L, Conversano E, Vianello FA, Martelli L, Gualeni C, Bassani F, Brugnara M, Rubin G, Parolin M, Anselmi M, Marchiori M, Vergine G, Miorin E, Vidal E, Milocco C, Orsi C, Puccio G, Peruzzi L, Montini G, Dall’Amico R, on the behalf of the Italian Society of Pediatric N (2022) How COVID-19 changed the epidemiology of febrile urinary tract infections in children in the emergency department during the first outbreak. BMC Pediatr 22:550. https://doi.org/10.1186/s12887-022-03516-7
Hatoun J, Correa ET, Donahue SMA, Vernacchio L (2020) Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics 146 https://doi.org/10.1542/peds.2020-006460
Cobo-Vazquez E, Aguilera-Alonso D, Carrasco-Colom J, Calvo C, Saavedra-Lozano J, Ped GASnWG (2023) Increasing incidence and severity of invasive group A streptococcal disease in Spanish children in 2019–2022. Lancet Reg Health Eur 27:100597. https://doi.org/10.1016/j.lanepe.2023.100597
Cohen PR, Rybak A, Werner A, Bechet S, Desandes R, Hassid F, Andre JM, Gelbert N, Thiebault G, Kochert F, Cahn-Sellem F, Vie Le Sage F, Angoulvant PF, Ouldali N, Frandji B, Levy C (2022) Trends in pediatric ambulatory community acquired infections before and during COVID-19 pandemic: a prospective multicentric surveillance study in France. Lancet Reg Health Eur 22:100497. https://doi.org/10.1016/j.lanepe.2022.100497
Lamagni T, Guy R, Chand M, Henderson KL, Chalker V, Lewis J, Saliba V, Elliot AJ, Smith GE, Rushton S, Sheridan EA, Ramsay M, Johnson AP (2018) Resurgence of scarlet fever in England, 2014–16: a population-based surveillance study. Lancet Infect Dis 18:180–187. https://doi.org/10.1016/S1473-3099(17)30693-X
Chen Q, Allot A, Lu Z (2020) Keep up with the latest coronavirus research. Nature 579:193. https://doi.org/10.1038/d41586-020-00694-1
Subbiah V (2023) The next generation of evidence-based medicine. Nat Med 29:49–58. https://doi.org/10.1038/s41591-022-02160-z
Teixeira da Silva JA, Tsigaris P, Erfanmanesh M (2021) Publishing volumes in major databases related to COVID-19. Scientometrics 126:831–842. https://doi.org/10.1007/s11192-020-03675-3
Raynaud M, Goutaudier V, Louis K, Al-Awadhi S, Dubourg Q, Truchot A, Brousse R, Saleh N, Giarraputo A, Debiais C, Demir Z, Certain A, Tacafred F, Cortes-Garcia E, Yanes S, Dagobert J, Naser S, Robin B, Bailly E, Jouven X, Reese PP, Loupy A (2021) Impact of the COVID-19 pandemic on publication dynamics and non-COVID-19 research production. BMC Med Res Methodol 21:255. https://doi.org/10.1186/s12874-021-01404-9
Riccaboni M, Verginer L (2022) The impact of the COVID-19 pandemic on scientific research in the life sciences. PLoS One 17:e0263001. https://doi.org/10.1371/journal.pone.0263001
Sohrabi C, Mathew G, Franchi T, Kerwan A, Griffin M, Soleil CDMJ, Ali SA, Agha M, Agha R (2021) Impact of the coronavirus (COVID-19) pandemic on scientific research and implications for clinical academic training - a review. Int J Surg 86:57–63. https://doi.org/10.1016/j.ijsu.2020.12.008
Heaton PM (2020) The COVID-19 vaccine-development multiverse. N Engl J Med 383:1986–1988. https://doi.org/10.1056/NEJMe2025111
Luxi N, Giovanazzi A, Capuano A, Crisafulli S, Cutroneo PM, Fantini MP, Ferrajolo C, Moretti U, Poluzzi E, Raschi E, Ravaldi C, Reno C, Tuccori M, Vannacci A, Zanoni G, Trifiro G, Ccg I (2021) COVID-19 Vaccination in pregnancy, paediatrics, immunocompromised patients, and persons with history of allergy or prior SARS-CoV-2 infection: overview of current recommendations and pre- and post-marketing evidence for vaccine efficacy and safety. Drug Saf 44:1247–1269. https://doi.org/10.1007/s40264-021-01131-6
Folegatti PM, Bittaye M, Flaxman A, Lopez FR, Bellamy D, Kupke A, Mair C et al (2020) Safety and immunogenicity of a candidate Middle East respiratory syndrome coronavirus viral-vectored vaccine: a dose-escalation, open-label, non-randomised, uncontrolled, phase 1 trial. Lancet Infect Dis 20:816–826. https://doi.org/10.1016/S1473-3099(20)30160-2
Martin JE, Louder MK, Holman LA, Gordon IJ, Enama ME, Larkin BD, Andrews CA, Vogel L, Koup RA, Roederer M, Bailer RT, Gomez PL, Nason M, Mascola JR, Nabel GJ, Graham BS, Team VRCS (2008) A SARS DNA vaccine induces neutralizing antibody and cellular immune responses in healthy adults in a Phase I clinical trial. Vaccine 26:6338–6343. https://doi.org/10.1016/j.vaccine.2008.09.026
Kumar A, Blum J, Le Thanh T, Havelange N, Magini D, Yoon IK (2022) The mRNA vaccine development landscape for infectious diseases. Nat Rev Drug Discov 21:333–334. https://doi.org/10.1038/d41573-022-00035-z
Barbier AJ, Jiang AY, Zhang P, Wooster R, Anderson DG (2022) The clinical progress of mRNA vaccines and immunotherapies. Nat Biotechnol 40:840–854. https://doi.org/10.1038/s41587-022-01294-2
Deng Z, Tian Y, Song J, An G, Yang P (2022) mRNA vaccines: the dawn of a new era of cancer immunotherapy. Front Immunol 13:887125. https://doi.org/10.3389/fimmu.2022.887125
Miao L, Zhang Y, Huang L (2021) mRNA vaccine for cancer immunotherapy. Mol Cancer 20:41. https://doi.org/10.1186/s12943-021-01335-5
Summan A, Nandi A, Shet A, Laxminarayan R (2023) The effect of the COVID-19 pandemic on routine childhood immunization coverage and timeliness in India: retrospective analysis of the National Family Health Survey of 2019–2021 data. Lancet Reg Health Southeast Asia 8:100099. https://doi.org/10.1016/j.lansea.2022.100099
Lavie M, Lavie I, Laskov I, Cohen A, Grisaru D, Grisaru-Soen G, Michaan N (2023) Impact of COVID-19 pandemic on human papillomavirus vaccine uptake in Israel. J Low Genit Tract Dis 27:168–172. https://doi.org/10.1097/LGT.0000000000000729
Raut A, Huy NT (2022) Impediments to child education, health and development during the COVID-19 pandemic in India. Lancet Reg Health Southeast Asia 1:100005. https://doi.org/10.1016/j.lansea.2022.04.001
Hotez PJ (2021) Mounting antiscience aggression in the United States. PLoS Biol 19:e3001369. https://doi.org/10.1371/journal.pbio.3001369
Karafillakis E, Van Damme P, Hendrickx G, Larson HJ (2022) COVID-19 in Europe: new challenges for addressing vaccine hesitancy. Lancet 399:699–701. https://doi.org/10.1016/S0140-6736(22)00150-7
Wilkinson E (2022) Is anti-vaccine sentiment affecting routine childhood immunisations? BMJ 376:o360. https://doi.org/10.1136/bmj.o360
Patel M, Lee AD, Redd SB, Clemmons NS, McNall RJ, Cohn AC, Gastanaduy PA (2019) Increase in measles cases - United States, January 1-April 26, 2019. MMWR Morb Mortal Wkly Rep 68:402–404. https://doi.org/10.15585/mmwr.mm6817e1
SeyedAlinaghi S, Karimi A, Mojdeganlou H, Alilou S, Mirghaderi SP, Noori T, Shamsabadi A, Dadras O, Vahedi F, Mohammadi P, Shojaei A, Mahdiabadi S, Janfaza N, Keshavarzpoor Lonbar A, Mehraeen E, Sabatier JM (2022) Impact of COVID-19 pandemic on routine vaccination coverage of children and adolescents: a systematic review. Health Sci Rep 5:e00516. https://doi.org/10.1002/hsr2.516
Neves FPG, Mestrovic T, Pinto TCA (2023) Editorial: drug resistance in maternal and paediatric bacterial and fungal infections: is COVID-19 changing the landscape. Front Microbiol 14:1177669. https://doi.org/10.3389/fmicb.2023.1177669
Fontana C, Favaro M, Minelli S, Bossa MC, Altieri A (2021) Co-infections observed in SARS-CoV-2 positive patients using a rapid diagnostic test. Sci Rep 11:16355. https://doi.org/10.1038/s41598-021-95772-3
Dutcher L, Li Y, Lee G, Grundmeier R, Hamilton KW, Gerber JS (2022) COVID-19 and antibiotic prescribing in pediatric primary care. Pediatrics 149 https://doi.org/10.1542/peds.2021-053079
Kronman MP, Gerber JS, Grundmeier RW, Zhou C, Robinson JD, Heritage J, Stout J, Burges D, Hedrick B, Warren L, Shalowitz M, Shone LP, Steffes J, Wright M, Fiks AG, Mangione-Smith R (2020) Reducing antibiotic prescribing in primary care for respiratory illness. Pediatrics 146 https://doi.org/10.1542/peds.2020-0038
Wittman SR, Martin JM, Mehrotra A, Ray KN (2023) Antibiotic receipt during outpatient visits for COVID-19 in the US, From 2020 to 2022. JAMA Health Forum 4:e225429. https://doi.org/10.1001/jamahealthforum.2022.5429
Malik SS, Mundra S (2022) Increasing consumption of antibiotics during the COVID-19 pandemic: implications for patient health and emerging anti-microbial resistance. Antibiotics (Basel) 12. https://doi.org/10.3390/antibiotics12010045
Kariyawasam RM, Julien DA, Jelinski DC, Larose SL, Rennert-May E, Conly JM, Dingle TC, Chen JZ, Tyrrell GJ, Ronksley PE, Barkema HW (2022) Antimicrobial resistance (AMR) in COVID-19 patients: a systematic review and meta-analysis (November 2019-June 2021). Antimicrob Resist Infect Control 11:45. https://doi.org/10.1186/s13756-022-01085-z
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Contributions
Moshe Shmueli, Idan Lender, and Shalom Ben-Shimol have all contributed equally to the conception and design of the review, drafted and revised the manuscript and approve its publication.
Corresponding author
Ethics declarations
Conflict of interest
Shalom Ben-Shimol has received within the last 35 months grants by Pfizer. He serves as scientific consultant and on the review board of Pfizer and MSD, and belongs to the speaker bureau of Pfizer, MSD, and GSK. The other authors do not report any conflict of interest.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shmueli, M., Lendner, I. & Ben-Shimol, S. Effect of the COVID-19 pandemic on the pediatric infectious disease landscape. Eur J Pediatr 183, 1001–1009 (2024). https://doi.org/10.1007/s00431-023-05210-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05210-x