Abstract
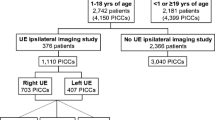
The risk factors associated with the probability of central venous access device (CVAD)-associated deep vein thrombosis (DVT) resolution have been hardly evaluated in children. Current guidelines suggest anticoagulation for a maximum of 3 months in patients with provoked DVT if the provoking factor is resolved. To know if the thrombus will resolve after anticoagulant therapy will help to choose whether to initiate and/or continue this treatment or not. We did a retrospective study of 85 pediatric patients (45 girls, 40 boys) with CVAD-associated DVT to examine the risk factors associated with lack of thrombus resolution in the first 6 months after diagnosis. Sixty-two children had their thrombosis resolved after a median of 50 days (p25-p75 25–97) since diagnosis. In multivariate analysis, variables significantly associated with no resolution were total occlusion (OR 12.50, 95% CI 2.99–52.14, p=.001), location in upper extremity, head, and neck veins (OR 17.70, 95% CI 1.64–191.43, p=.018); collateral circulation in the first 45 days after diagnosis (OR 33.55, 95% CI 2.42–464.71, p=.009); and having between 0 and 3 prothrombotic risk factors at diagnosis (OR 6.20, 95% CI 1.21–31.75, p=.029).
Conclusion: CVAD-associated DVT resolution in children in the first 6 months since diagnosis was significantly lower if the thrombosis was occlusive, if it was located in the upper extremity, head, and neck veins; if collateral circulation was seen on ultrasound in the first 45 days; and/or when the patient showed less prothrombotic risk factors at diagnosis.
What is Known: • The risk factors associated with central venous access device-associated deep vein thrombosis resolution have been hardly evaluated in children. • Current guidelines suggest anticoagulation for a maximum of 3 months in provoked vein thrombosis if the provoking factor is resolved. | |
What is New: • Thrombus resolution was lower if it was occlusive, located in the upper extremity veins, if collateral circulation was seen, and with less prothrombotic risk factors at diagnosis. • To know if the thrombus will resolve after anticoagulation will help to choose whether to initiate and/or continue it or not. |
Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- CVAD:
-
Central venous access device
- DVT:
-
Deep vein thrombosis
- LMWH:
-
Low-molecular-weight heparin
References
Raffini L, Huang YS, Witmer C, Feudtner C (2009) Dramatic increase in venous thromboembolism in children’s hospitals in the United States from 2001 to 2007. Pediatrics 124:1001–1008
Mahajerin A, Croteau SE (2017) Epidemiology and risk assessment of pediatric venous thromboembolism. Front Pediatr 5:68
Witmer CM, Takemoto CM (2017) Pediatric hospital acquired venous thromboembolism. Front Pediatr 5:198
Witmer C, Raffini L (2020) Treatment of venous thromboembolism in pediatric patients. Blood 135:335–343
Monagle P, Cuello CA, Augustine C et al (2018) American Society of Hematology 2018 Guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv 2:3292–3316
Menéndez JJ, Verdú C, Calderón B, Gómez-Zamora A, Schüffelmann C, de la Cruz JJ, de la Oliva P (2016) Incidence and risk factors of superficial and deep vein thrombosis associated with peripherally inserted central catheters in children. J Thromb Haemost 14:2158–2168
Polen E, Weintraub M, Stoffer C, Jaffe DH, Burger A, Revel-Vilk S (2015) Post-thrombotic syndrome after central venous catheter removal in childhood cancer survivors: a prospective cohort study. Pediatr Blood Cancer 62:285–290
Asouzu MA, Shroyer M, Graham JS, Wilkinson L, Galloway DP, Martin CA (2019) Development of venous thrombi in a pediatric population of intestinal failure. J Pediatr Surg 54:2145–2148
Setty BA, O’Brien SH, Kerlin BA (2012) Pediatric venous thromboembolism in the United States: a tertiary care complication of chronic diseases. Pediatr Blood Cancer 59:258–264
Goldenberg NA, Abshire T, Blatchford PJ et al (2015) Multicenter randomized controlled trial on duration of therapy for thrombosis in children and young adults (the Kids-DOTT trial): pilot/feasibility phase findings. J Thromb Haemost 13:1597–1605
Mahajerin A, Betensky M, Goldenberg NA (2019) Thrombosis in children: approach to anatomic risks, thrombophilia, prevention, and treatment. Hematol Oncol Clin North Am 33:439–453
Monagle P, Chan AKC, Goldenberg NA, Ichord RN, Journeycake JM, Nowak-Göttl U, Vesely SK (2012) Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141:e737S–e801S
Atchison CM, Arlikar S, Amankwah E, Ayala I, Barrett L, Branchford BR, Streiff M, Takemoto C, Goldenberg NA (2014) Development of a new risk score for hospital-associated venous thromboembolism in noncritically ill children: findings from a large single-institutional case-control study. J Pediatr 165:793–798
Arlikar SJ, Atchison CM, Amankwah EK, Ayala IA, Barrett LA, Branchford BR, Streiff M, Takemoto C, Goldenberg NA (2015) Development of a new risk score for hospital-associated venous thromboembolism in critically-ill children not undergoing cardiothoracic surgery. Thromb Res 136:717–722
Connelly CR, Laird A, Barton JS, Fischer PE, Krishnaswami S, Schreiber MA, Zonies DH, Watters JM (2016) A clinical tool for the prediction of venous thromboembolism in pediatric trauma patients. JAMA Surg 151:50–57
Jaffray J, Mahajerin A, Young G, Goldenberg N, Ji L, Sposto R, Stillings A, Krava E, Branchford B (2018) A multi-institutional registry of pediatric hospital-acquired thrombosis cases: the Children’s Hospital-Acquired Thrombosis. Thromb Res 161:67–72
Kenet G, Cohen O, Bajorat T, Nowak-Göttl U (2019) Insights into neonatal thrombosis. Thromb Res 181S1:S33–S36
González-Hernández J, Daoud Y, Styers J, Journeycake JM, Channabasappa N, Piper HG (2016) Central venous thrombosis in children with intestinal failure on long-term parenteral nutrition. J Pediatr Surg 51:790–793
Jones S, Butt W, Monagle P, Cain T, Newall F (2019) The natural history of asymptomatic central venous catheter–related thrombosis in critically ill children. Blood 133:857–866
Jaffray J, Goldenberg N (2020) Current approaches in the treatment of catheter-related deep venous thrombosis in children. Expert Rev Hematol 13:607–617
Smith R, Jones S, Newall F (2017) Six weeks versus 3 months of anticoagulant treatment for pediatric central venous catheter-related venous thromboembolism. J Pediatr Hematol Oncol 39:518–523
Tarango C, Schulman S, Betensky M, Goldenberg NA (2018) Duration of anticoagulant therapy in pediatric venous thromboembolism: current approaches and updates from randomized controlled trials. Expert Rev Hematol 11:37–44
Revel-Vilk S, Sharathkumar A, Massicotte P, Marzinotto V, Daneman A, Dix D, Chan A (2004) Natural history of arterial and venous thrombosis in children treated with low molecular weight heparin: a longitudinal study by ultrasound. J Thromb Haemost 2:42–46
Avila ML, Pullenayegum E, Williams S, Yue N, Krol P, Brandão LR (2016) Postthrombotic syndrome and other outcomes of lower extremity deep vein thrombosis in children. Blood 128:1862–1869
Manlhiot C, Brandão LR, Schwartz SM, Sivarajan VB, Williams S, Collins TH, McCrindle BW (2016) Management and outcomes of patients with occlusive thrombosis after pediatric cardiac surgery. J Pediatr 169:146–153
Fan JL, Roberts LE, Scheurer ME, Yee DL, Shah MD, Lee-Kim YJ (2017) Association of outcomes and anti-Xa levels in the treatment of pediatric venous thromboembolism. Pediatr Blood Cancer 64:e26629
Kuhle S, Koloshuk B, Marzinotto V, Bauman M, Massicotte P, Andrew M, Chan A, Abdolell M, Mitchell L (2003) A cross-sectional study evaluating post-thrombotic syndrome in children. Thromb Res 111:227–233
Neshat-Vahid S, Pierce R, Hersey D, Raffini LJ, Faustino EV (2016) Association of thrombophilia and catheter-associated thrombosis in children: a systematic review and meta-analysis. J Thromb Haemost 14:1749–1758
Author information
Authors and Affiliations
Contributions
Dr. García-Boyano, Dr. Caballero-Caballero, and Dr. Climent Alcalá conceptualized and designed the study, collected data, and drafted the initial manuscript. Dr. García Fernández de Villalta, Dr. Gutiérrez Alvariño, and Dr. Blanco Bañares made substantial contributions to the conception of the work and to the acquisition of data and reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was authorized by the Ethics Committee of our institution.
Consent to participate
Not applicable (retrospective study).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
García-Boyano, M., Caballero-Caballero, J.M., García Fernández de Villalta, M. et al. Risk factors determining central venous access device-associated deep vein thrombosis resolution in children: a retrospective study. Eur J Pediatr 180, 1907–1914 (2021). https://doi.org/10.1007/s00431-021-03985-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-03985-5