Abstract
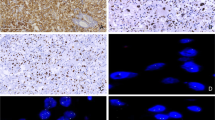
Vasculogenic mesenchymal lesions (VMLs) of germ cell tumor origin are thought to originate in postpubertal-type yolk sac tumor components and include a spectrum of lesions from teratoma with vasculogenic stroma (TVS), to low and high-grade vasculogenic mesenchymal tumors (VMTs). VMLs exhibit rudimentary to well-developed neoplastic vessels within primitive mesenchyme, being considered a neoplastic reiteration of embryonic vasculogenesis in the splanchnic mesoderm of the yolk sac. They occur in patients with primary mediastinal germ cell tumors after chemotherapy, and a subset progresses to “somatic-type” sarcomas [including angiosarcoma (AS)], with high-grade VMTs likely portending a higher risk. Recently, we encountered a low-grade VMT that progressed to metastatic AS during follow-up. In this case, both the low-grade VMT and the subsequent AS demonstrated p53 overexpression, suggesting that p53 alterations may precede histopathologic transformation. To test this hypothesis, we evaluated neoplasms representing the entire spectrum of VMLs using p53 immunohistochemistry (IHC; clone DO-7, Dako). Overexpression was defined as nuclear positivity in > 80% of neoplastic cells. Because the distinction between high-grade VMT and AS can be subjective in some cases, they were grouped together in a single category. Thirty-nine VMLs were assessed: 16 high-grade VMT/AS, 19 low-grade VMT, and 4 TVS. Patient age ranged from 19 to 46 years (mean, 30 years; male = 97%). Four high-grade VMT/AS and one low-grade VMT showed p53 overexpression (5/39 VMLs, 13%; 4/16 high-grade VMT/AS, 25%). These tumors included 1 unequivocal AS and 1 high-grade VMT/AS with progression to rhabdomyosarcoma. The only low-grade VMT with p53 overexpression demonstrated progression to AS. Another high-grade VMT that progressed to sarcoma demonstrated p53 overexpression in the sarcoma component, but it was excluded because the VMT was not represented in the material available at the time of the study. Lesions with intratumoral grade heterogeneity (classified based the highest grade), demonstrated more pronounced p53 overexpression in the high-grade components. P53 overexpression is associated with disease progression in a subset of VMTs and may precede morphologic transformation to sarcoma. Routine evaluation of VMTs with p53 IHC seems justified, with overexpressors likely requiring an close clinical surveillance.






Similar content being viewed by others
Data availability
Not applicable.
Change history
27 April 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00428-024-03808-6
References
Levy DR, Agaram NP, Kao CS, Franks SE, Kesler KA, Stram AR, Einhorn LH, Bangs CD, Ulbright TM (2021) Vasculogenic Mesenchymal Tumor: A Clinicopathologic and Molecular Study of 55 Cases of a Distinctive Neoplasm Originating From Mediastinal Yolk Sac Tumor and an Occasional Precursor to Angiosarcoma. Am J Surg Pathol 45:463–476. https://doi.org/10.1097/PAS.0000000000001615
Zhanxian S, Yuchen H, Jinzhi W, Lei Z (2023) Mediastinal high-grade vasculogenic mesenchymal tumour with seminoma: a case report and literature review. Diagn Pathol 18:56. https://doi.org/10.1186/s13000-023-01333-9
Kouchi Y, Komatsu S, Harada S, Shinomiya Y, Ikeda JI, Kishimoto T (2023) Ovarian Malignant Mixed Germ Cell Tumor Composed Mainly of a Polyembryoma Pattern With Vasculogenic Mesenchymal Tumor Components. Int J Gynecol Pathol 42:78–82. https://doi.org/10.1097/PGP.0000000000000867
Fujii H, Yamada Y, Yamamura K, Ishida Y, Tsujimura M, Matsumoto K, Tanaka S, Date H, Nishikawa T, Yoshida Y, Kashima J, Yatabe Y, Ogawa S, Marx A, Ulbright TM, Haga H (2023) A case of vasculogenic mesenchymal tumor in the mediastinum: whole-exome sequencing reveals origin from pre-existing germ cell tumor. Virchows Arch 482:923–927. https://doi.org/10.1007/s00428-023-03529-2
Levine AJ, Momand J, Finlay CA (1991) The p53 tumour suppressor gene. Nature 351:453–456. https://doi.org/10.1038/351453a0
Gorgoulis VG, Vassiliou LV, Karakaidos P, Zacharatos P, Kotsinas A, Liloglou T, Venere M, Ditullio RA Jr, Kastrinakis NG, Levy B, Kletsas D, Yoneta A, Herlyn M, Kittas C, Halazonetis TD (2005) Activation of the DNA damage checkpoint and genomic instability in human precancerous lesions. Nature 434:907–913. https://doi.org/10.1038/nature03485
Bartek J, Bartkova J, Vojtesek B, Staskova Z, Lukas J, Rejthar A, Kovarik J, Midgley CA, Gannon JV, Lane DP (1991) Aberrant expression of the p53 oncoprotein is a common feature of a wide spectrum of human malignancies. Oncogene 6:1699–1703
Italiano A, Chen CL, Thomas R, Breen M, Bonnet F, Sevenet N, Longy M, Maki RG, Coindre JM, Antonescu CR (2012) Alterations of the p53 and PIK3CA/AKT/mTOR pathways in angiosarcomas: a pattern distinct from other sarcomas with complex genomics. Cancer 118:5878–5887. https://doi.org/10.1002/cncr.27614
Thoenen E, Curl A, Iwakuma T (2019) TP53 in bone and soft tissue sarcomas. Pharmacol Ther 202:149–164. https://doi.org/10.1016/j.pharmthera.2019.06.010
Wyvekens N, Sholl LM, Yang Y, Tran I, Vasudevaraja V, Dickson BC, Al-Obaidy KI, Baniak N, Collins K, Gordetsky JB, Idrees MT, Kao CS, Maclean F, Matoso A, Ulbright TM, Wobker SE, Fletcher CDM, Hirsch MS, Hornick JL, Snuderl M, Acosta AM (2022) Molecular correlates of male germ cell tumors with overgrowth of components resembling somatic malignancies. Mod Pathol 35:1966–1973. https://doi.org/10.1038/s41379-022-01136-1
Bacon JVW, Giannatempo P, Cataldo G, Fazli L, Saxena N, Ozgun G, Soleimani M, Chi K, Nichols C, Necchi A, Wyatt AW, Kollmannsberger CK, Nappi L (2022) TP53 Alterations Are Associated With Poor Survival in Patients With Primary Mediastinal Nonseminoma Germ Cell Tumors. Oncologist 27:e912–e915. https://doi.org/10.1093/oncolo/oyac197
Author information
Authors and Affiliations
Contributions
Concept: Andres M. Acosta and Thomas M. Ulbright; Design and coordination: Andres M. Acosta and Reem Youssef; Review of histologic slides and immunohistochemistry results: Reem Youssef, Thomas M. Ulbright and Andres M. Acosta; Manuscript draft (including figures and tables): Reem Youssef and Andres M. Acosta; Manuscript editing and intellectual input: All authors.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no financial or intellectual conflicts of interest pertaining to the contests of this manuscript.
Additional information
This study has been accepted for presentation at the 113th Annual Meeting of the United States and Canadian Academy of Pathology (USCAP) in Baltimore, being subject to embargo until 3/25/2024 at 9:30 am.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The added data in Table 1 has been removed.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Youssef, R., Ulbright, T.M. & Acosta, A.M. P53 Overexpression May Represent an Early Marker of Clinicopathologic Progression in Vasculogenic Mesenchymal Lesions of Germ Cell Tumor Origin. Virchows Arch (2024). https://doi.org/10.1007/s00428-024-03786-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00428-024-03786-9