Abstract
Uterine carcinosarcoma (UCS) has been proposed as a model for epithelial–mesenchymal transition (EMT), a process characterized by a functional change facilitating migration and metastasis in many types of cancer. L1CAM is an adhesion molecule that has been involved in EMT as a marker for mesenchymal phenotype. We examined expression of L1CAM in UCS in a cohort of 90 cases from four different centers. Slides were immunohistochemically stained for L1CAM and scored in four categories (0%, < 10%, 10–50%, and > 50%). A score of more than 10% was considered positive for L1CAM. The median age at presentation was 68.6 years, and half of the patients (53.3%) presented with FIGO stage 1 disease. Membranous L1CAM expression was positive in the epithelial component in 65.4% of cases. Remarkably, expression was negative in the mesenchymal component. In cases where both components were intermingled, expression limited to the epithelial component was confirmed by a double stain for L1CAM and keratin. Expression of L1CAM did not relate to overall or disease-free survival. Our findings suggest L1CAM is either not a marker for the mesenchymal phenotype in EMT, or UCS is not a good model for EMT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uterine carcinosarcoma (UCS) is a rare subtype of endometrial cancer (EC) with a poor prognosis. Approximately 60% of cases present with advanced disease, and recurrence occurs in approximately 50% of patients [1,2,3,4]. Accordingly, 5-year survival ranges from 33 to 39%. Histology is peculiar because it contains both an epithelial as well as a mesenchymal component [1, 5]. Various models have been proposed to explain this feature ranging from collision of two separate and original components to conversion of a common monoclonal neoplasm of epithelial (carcinomatous) origin [5,6,7,8]. Currently, most studies support the theory of conversion of an endometrial carcinoma into a cancer consisting of an epithelial and a mesenchymal component.
Because UCS contains both an epithelial and mesenchymal component, UCS has been suggested as a model for epithelial–mesenchymal transition (EMT) [5, 9,10,11,12,13,14]. EMT is a process that is characterized by a functional change in tumor cells that facilitates migration and metastasis [11, 15]. By loss of cell polarity and cell–cell junctions, and by reorganization of their cytoskeleton, tumor cells acquire the ability to migrate. This transformation is thought to be essential to metastasis in gynecologic cancers as well as other tumors [13, 16]. In a study on 76 cases of UCS, Castilla et al. found a different expression of epithelial and mesenchymal markers between the two components. Expression of E-cadherin for example was limited to the epithelial component.
A possible marker for a mesenchymal phenotype is L1 cell adhesion molecule (L1CAM), a transmembrane adhesion molecule important for embryonic development [17]. The extracellular domain interacts with other binding molecules and integrins expressed on either the same or other cells. The cytoplasmic tail mainly interacts with cytoskeletal proteins. Several studies support involvement of L1CAM in EMT [18,19,20,21]. Exposure of both endometrial cancer (EC) and breast cancer cell lines to transforming growth factor B1 (TGF-B1), a known inducer of EMT, results in increased expression of L1CAM [19, 21]. Huszar et al. found that increased expression of L1CAM relates to reduced membranous expression of E-cadherin. L1CAM could be a marker for a mesenchymal phenotype of EMT in UCS.
Expression of L1CAM previously described as immunohistochemical staining of more than 10% is absent in normal endometrium [22]. In addition, expression of L1CAM is related to metastasis and poor prognosis in many cancers, including EC [17, 22,23,24,25,26,27,28]. In early-stage EC with endometrioid histology, expression of L1CAM is related to unfavorable pathological findings, distant recurrence and poor survival [22, 23]. Correspondingly, in high grade EC and non-endometrioid EC (NEEC), L1CAM expression is related to unfavorable pathological findings such as advanced stage and lymphovascular space invasion (LVSI) as well as distant recurrence but not survival [26,27,28].
We hypothesize that L1CAM could be involved in EMT in UCS as a marker for the mesenchymal phenotype and may relate to metastasis. Therefore, we aimed to evaluate L1CAM expression in a large cohort of 90 UCS patients assembled in 4 oncologic centers participating in the European Network for Individualized Treatment of Endometrial Cancer (ENITEC) collaboration. Expression was evaluated separately in the epithelial and the mesenchymal component and related to patient and tumor characteristics and survival.
Methods
Study population
Four-micrometer formalin-fixed slides were assembled from four separate centers (Haukeland University hospital Bergen, Norway; University hospital Lleida, Spain; Leiden University Medical Center, The Netherlands; and University Medical Center Groningen, the Netherlands). Sufficient material from 88 primary tumors and 10 metastases was available. With an overlap of 8 cases, this added up to a total of 90 cases with UCS diagnosed between 1980 and 2012 to be included in this study. Data concerning age at diagnosis, International Federation of Gynecology and Obstetrics (FIGO) stage as well as patient and tumor characteristics concerning age at diagnosis, histology of both components (homologue or heterologue for the epithelial component), differentiation grade, LVSI, were delivered by each participating center. All material was revised at the University Medical Center Groningen by HH and MV blinded from findings at the primary center. For some cases, clinicopathological information was missing and could not be retrieved from the slides, for example, when information on lymphovascular space involvement was missing. Follow-up data was provided by each center in an anonymized dataset and completed until October 2014. Datasets were combined into a final password-protected database. Patient identity was protected by study-specific patient numbers. Informed consent was obtained according to local protocol in each participating center.
Histology
Slides, 4-μm formalin-fixed paraffin-embedded sections were immunohistochemically stained as described by Bosse et al. [23]. “Briefly, formalin fixed paraffin-embedded (FFPE) tissue blocks were cut into 4 μm slides and mounted on Starfrost slides. Antigen retrieval was achieved by microwave oven procedure in 10 mmol/L citrate buffer, pH 6. Sections were incubated overnight with primary monoclonal antibodies against L1CAM (CD171, clone 14.10, SIG-3911, Convance Inc., lot number D13KF03087, Biolegend, San Diego, USA) in a 1:500 dilution. Sections were incubated and stained for 30 min using a secondary antibody (Poly-HRP-GAM/R/R; DPV0110HRP; ImmunoLogic, Duiven, The Netherlands). The slides were counterstained with Mayer’s Haematoxylin, dehydrated and mounted. Omission of the primary antibody was used as a negative control and a highly L1CAM-expressing serous ovarian cancer as an external positive control.”
In eight cases, it was difficult to differentiate between L1CAM expression by the epithelial or mesenchymal components as both components were intermingled. Therefore, these selected cases were double stained for both L1CAM and cytokeratin-8 as expression of cytokeratin is limited to the epithelial component. Tissue sections were dewaxed in xylene and hydrated in a graded series of alcohol to tap water. Antigen retrieval was performed in 10 mM EDTA pH 8.0 in a microwave at 400 W for 15 min. Endogenous peroxidase was blocked by incubating sections for 30 min in 1% H2O2. Primary antibody against L1CAM (anti-CD171, Biolegend, Sig-3911-1000, San Diego, USA) was applied in a 1:500 dilution and left to incubate overnight at 4 °C. Subsequently, tissue sections were incubated with secondary antibody (RAM-HRP; Dako, Glostrop, Denmark) and tertiary antibody (GAR-HRP; Dako, Glostrop, Denmark), both diluted at 1:100, for 30 min each at room temperature. L1CAM staining was visualized with 3,3′-diaminobenzidine. After washing the sections in demineralized water, they were incubated with the antibody against cytokeratin-8 (CAM 5.2, BD Biosciences, #345779) diluted 1:5 for 1 h at room temperature. Sections were then incubated with secondary antibody (RAMbio; Dako) and tertiary antibody (streptavidin-AP; Dako), both diluted 1:300, for 30 min each at room temperature. Cytokeratin staining was visualized using Fast Blue BB/Napthhol-AS-MX-phosphate (Sigma, F3378) for 30 min at room temperature. Sections were rinsed with demineralized water and mounted with Kaiser’s glycerol gelatine (109242; Merck). Omission of the primary antibody was used as a negative control and tonsil tissue as a positive control.
Evaluation of immunohistochemistry
Evaluation of immunohistochemistry was performed by two independent investigators (MV and AP), blinded for clinical outcome data. Expression of L1CAM in either component was scored as the percentage of positive membranous staining and categorized into four groups: 0%, 0–10%, 10–50%, or > 50% as described by Meier et al. [29]. In conformity with previous publications, tumors with more than 10% expression of L1CAM were considered positive [23, 29]. There was no disagreement in evaluation of the mesenchymal component. There was disagreement in evaluation of 21 cases of the carcinomatous component mainly on a score of either 3 or 4. Disagreement was resolved by consensus. Location of L1CAM staining was scored as expression at the tumor center, tumor margin, or diffusely over the tumor.
Statistical analysis
All statistical analyses were done by using SPSS (version 23, IBM Statistics, Chicago USA). For analysis, age was dichotomized into 65 and below versus above 65 years as this is an important cutoff in treatment of endometrial cancer. Recurrence was classified as local, pelvic, or distant. Disease-free survival (DFS) was defined as time until any recurrence or death of disease and disease-specific survival (DSS) as time until death of disease. Associations between patient and tumor characteristics were compared using logistic regression analyses. For survival analysis, a relation between L1CAM expression and DFS, DSS, or distant recurrence was examined using Cox regression analyses. Patients without evidence of disease were censored at last date of follow-up.
Results
Population
Tissue from the primary tumor was available in 88 cases. In 10 cases, metastatic tissue was available. With an overlap of 8 cases (primary as well as metastatic tissue), this added up to a total of 90 cases to be evaluated. Not all tissue contained both components. The epithelial component was available in 81 cases and the mesenchymal component in 83 cases. Patient and tumor characteristics are shown in Table 1. The median age at diagnosis was 68.6 years (IQR 62.0–75.5). A small majority of cases presented with FIGO stage 1 disease (53.3%), most other cases presented with stage 3a or 3c disease (14.4 vs 12.2%). LVSI was observed in 53.8%, and non-endometrioid histology of the epithelial component was 56.5%.
Immunohistochemistry
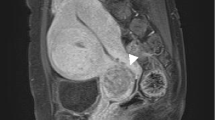
Figure 1 shows examples of L1CAM expression in both components. Expression was not limited to either the tumor center or margin.
Table 2 shows the results of L1CAM staining. The epithelial component was L1CAM positive in a majority of cases (65.4%). Remarkably, the mesenchymal component was determined as negative (< 10%) for L1cam in all cases. In 86.7%, no expression was found. In 13.3%, L1CAM expression was scored less than 10%. In some of these cases, both components were intermingled and therefore difficult to distinguish. To differentiate between L1CAM expression by either component, a double stain for L1CAM and keratin was performed in eight cases. In all eight cases, L1CAM expression was limited to cells expressing keratin. Figure 2 shows examples of double staining for L1CAM.
Examples of double stain for L1CAM (brown) and keratin (blue). a HE stain of case 8. This case was originally scores as L1CAM expression > 50% in the epithelial component and 0% in the mesenchymal component. b Double stain for L1CAM and keratin in case 8. c HE stain for case 9. This case was originally scores as L1CAM expression > 50% in the epithelial component and 0% in the mesenchymal component. d Double stain for L1CAM and keratin in case 9. e HE stain for case 14. This case was originally scored as L1CAM expression > 50% in the epithelial component and < 10% in the mesenchymal component. f Double stain for L1CAM and keratin in case 14. All figures are presented at × 10 magnification
Patient and tumor characteristics in relation to L1CAM expression
Table 3 shows patient and tumor characteristics stratified for L1CAM expression. Logistic regression showed no relation between patient or tumor characteristics and L1CAM expression. L1CAM expression survival in the overall cohort was poor with a median DFS of 2.83 years (95%CI 0.80–4.87) and DSS of 3.30 (1.10–5.50). Known prognostic variables related to DFS in univariate Cox regression analysis: FIGO stage (HR 1.67 95%CI 1.30–2.14), myometrial invasion (HR 1.80 95%CI 0.96–3.34), and differentiation grade (HR 3.81 95%CI 1.13–12.80). LVSI was not a significant predictor for DFS. Findings were similar for DSS. Expression of L1CAM did not relate to either DFS (HR 1.48 95%CI 0.74–3.00) or DSS (HR 1.48 95%CI 0.74–3.00). There was also no relation between L1CAM expression and distant recurrence (HR1.02 95%CI 0.45–2.30).
Discussion
L1CAM is frequently expressed in UCS, but expression in UCS is limited to the epithelial component. Expression does not relate to patient characteristics, recurrence, or survival.
Expression of L1CAM in UCS is in accordance with other studies on L1CAM expression in aggressive histologic subtypes of EC such as non-endometrioid EC. These studies describe an L1CAM expression of more than 55% and no relation with survival [22, 23, 27]. We also find a high percentage of L1Cam positive tumors and no relation between L1CAM expression and survival. A strong relation between expression and survival is therefore unlikely. An explanation for the absence of a relation could be the already poor survival in cohorts of NEEC and the high expression of L1CAM in NEEC as compared to EEC as suggested by van der Putten et al. [27]. Remarkably, L1CAM expression is not expressed in the mesenchymal component. Our working hypothesis was that L1CAM expression could act as a marker for a mesenchymal component in UCS. Several other studies describe increased expression of L1CAM after induction of EMT. In endometrial cancer cell lines, TGF-B1 induces expression of L1CAM and EMT [19, 21]. Exposure to TGF-B1 results in increased expression of L1CAM through upregulation of the EMT transcription factor Slug. In turn, expression of L1Cam relates to cell migration and invasion [21]. TGF-B1-induced L1CAM expression is related to decreased expression of E-cadherin, and E-cadherin expression is limited to the epithelial component in UCS [10, 19]. Considering our findings, L1CAM is either not a marker for the mesenchymal phenotype in EMT, or UCS is not a good model for EMT.
However, this does not exclude a relevant contribution of L1CAM expression in an early stage of EMT where cancer cells gain motility and invasive properties. This could be by direct function as an adhesion molecule or indirect by acting as a signaling molecule [17, 20]. At a later stage, motility and invasive properties may become less relevant when tumor cells form a secondary tumor.
A strength of this study is a large cohort of 90 UCS cases made possible through an international collaboration. The resulting population covers well the diversity of this type of cancer as can be seen in Table 1. Another strength is the stepwise approach with a double stain for cases where histology proved difficult. A limitation is the retrospective nature of the study.
In conclusion, we describe a large cohort of 90 cases with UCS where the majority of tumors stained positive for L1CAM but where expression is limited to the epithelial component. L1CAM could be involved in development of UCS and EMT at an early stage but is not a marker for the mesenchymal phenotype. Our study provides further insight into the possible mechanism of EMT and metastasis. Expression of L1CAM did not relate to unfavorable patient and tumor characteristics, recurrence, or survival.
References
Cantrell LA, Blank SV, Duska LR (2015) Uterine carcinosarcoma: a review of the literature. Gynecol Oncol 137:581–588
Vorgias G, Fotiou S (2010) The role of lymphadenectomy in uterine carcinosarcomas (malignant mixed mullerian tumours): a critical literature review. Arch Gynecol Obstet 282:659–664
Versluis MAC, Pielsticker C, van der Aa MA, de Bruyn M, Hollema H, Nijman HW (2018) Lymphadenectomy and adjuvant therapy improve survival with uterine carcinosarcoma: a large retrospective cohort study. Oncology:1–9
Boll D, Verhoeven RH, van der Aa MA, Pauwels P, Karim-Kos HE, Coebergh JW, van Doorn HC (2012) Incidence and survival trends of uncommon corpus uteri malignancies in the Netherlands, 1989-2008. Int J Gynecol Cancer 22:599–606
Matias-Guiu X, Prat J (2013) Molecular pathology of endometrial carcinoma. Histopathology 62:111–123
de Jong RA, Nijman HW, Wijbrandi TF, Reyners AK, Boezen HM, Hollema H (2011) Molecular markers and clinical behavior of uterine carcinosarcomas: focus on the epithelial tumor component. Mod Pathol
McCluggage WGRS (2009) Mesenchymal uterine tumors and adenomyosis. In: Robboy SJ, Mutter GL, Prat J, Bentley RC, Russell P, Anderson MC (eds) Pathology of the female reproductive tract, 2nd edn. Churchill Livingstone Elsevier, Amsterdam, pp 427–456
McCluggage WG (2002) Malignant biphasic uterine tumours: carcinosarcomas or metaplastic carcinomas? J Clin Pathol 55:321–325
Guarino M, Rubino B, Ballabio G (2007) The role of epithelial-mesenchymal transition in cancer pathology. Pathology 39:305–318
Castilla MA, Moreno-Bueno G, Romero-Perez L, Van De Vijver K, Biscuola M, Lopez-Garcia MA, Prat J, Matias-Guiu X, Cano A, Oliva E, Palacios J (2011) Micro-RNA signature of the epithelial-mesenchymal transition in endometrial carcinosarcoma. J Pathol 223:72–80
Chaffer CL, Weinberg RA (2011) A perspective on cancer cell metastasis. Science 331:1559–1564
Hugo H, Ackland ML, Blick T, Lawrence MG, Clements JA, Williams ED, Thompson EW (2007) Epithelial-mesenchymal and mesenchymal-epithelial transitions in carcinoma progression. J Cell Physiol 213:374–383
Stewart CJ, McCluggage WG (2013) Epithelial-mesenchymal transition in carcinomas of the female genital tract. Histopathology 62:31–43
Piulats JM, Guerra E, Gil-Martin M, Roman-Canal B, Gatius S, Sanz-Pamplona R, Velasco A, Vidal A, Matias-Guiu X (2017) Molecular approaches for classifying endometrial carcinoma. Gynecol Oncol 145:200–207
Thiery JP, Acloque H, Huang RY, Nieto MA (2009) Epithelial-mesenchymal transitions in development and disease. Cell 139:871–890
Colas E, Pedrola N, Devis L, Ertekin T, Campoy I, Martinez E, Llaurado M, Rigau M, Olivan M, Garcia M, Cabrera S, Gil-Moreno A, Xercavins J, Castellvi J, Garcia A, Ramon y Cajal S, Moreno-Bueno G, Dolcet X, Alameda F, Palacios J, Prat J, Doll A, Matias-Guiu X, Abal M, Reventos J (2012) The EMT signaling pathways in endometrial carcinoma. Clin Transl Oncol 14:715–720
Altevogt P, Doberstein K, Fogel M (2016) L1CAM in human cancer. Int J Cancer 138:1565–1576
Doberstein K, Harter PN, Haberkorn U, Bretz NP, Arnold B, Carretero R, Moldenhauer G, Mittelbronn M, Altevogt P (2015) Antibody therapy to human L1CAM in a transgenic mouse model blocks local tumor growth but induces EMT. Int J Cancer 136:E326–E339
Huszar M, Pfeifer M, Schirmer U, Kiefel H, Konecny GE, Ben-Arie A, Edler L, Munch M, Muller-Holzner E, Jerabek-Klestil S, Abdel-Azim S, Marth C, Zeimet AG, Altevogt P, Fogel M (2010) Up-regulation of L1CAM is linked to loss of hormone receptors and E-cadherin in aggressive subtypes of endometrial carcinomas. J Pathol 220:551–561
Kiefel H, Bondong S, Hazin J, Ridinger J, Schirmer U, Riedle S, Altevogt P (2012) L1CAM: a major driver for tumor cell invasion and motility. Cell Adhes Migr 6:374–384
Kiefel H, Bondong S, Pfeifer M, Schirmer U, Erbe-Hoffmann N, Schafer H, Sebens S, Altevogt P (2012) EMT-associated up-regulation of L1CAM provides insights into L1CAM-mediated integrin signalling and NF-kappaB activation. Carcinogenesis 33:1919–1929
Zeimet AG, Reimer D, Huszar M, Winterhoff B, Puistola U, Azim SA, Muller-Holzner E, Ben-Arie A, van Kempen LC, Petru E, Jahn S, Geels YP, Massuger LF, Amant F, Polterauer S, Lappi-Blanco E, Bulten J, Meuter A, Tanouye S, Oppelt P, Stroh-Weigert M, Reinthaller A, Mariani A, Hackl W, Netzer M, Schirmer U, Vergote I, Altevogt P, Marth C, Fogel M (2013) L1CAM in early-stage type I endometrial cancer: results of a large multicenter evaluation. J Natl Cancer Inst 105:1142–1150
Bosse T, Nout RA, Stelloo E, Dreef E, Nijman HW, Jurgenliemk-Schulz IM, Jobsen JJ, Creutzberg CL, Smit VT (2014) L1 cell adhesion molecule is a strong predictor for distant recurrence and overall survival in early stage endometrial cancer: pooled PORTEC trial results. Eur J Cancer 50:2602–2610
Dellinger TH, Smith DD, Ouyang C, Warden CD, Williams JC, Han ES (2016) L1CAM is an independent predictor of poor survival in endometrial cancer—an analysis of The Cancer Genome Atlas (TCGA). Gynecol Oncol 141:336–340
Fogel M, Gutwein P, Mechtersheimer S, Riedle S, Stoeck A, Smirnov A, Edler L, Ben-Arie A, Huszar M, Altevogt P (2003) L1 expression as a predictor of progression and survival in patients with uterine and ovarian carcinomas. Lancet 362:869–875
Fadare O, Roma AA, Desouki MM, Gwin K, Hanley KZ, Jarboe EA, Liang SX, Quick CM, Zheng W, Hecht JL, Parkash V, Wang XJ (2018) The significance of L1CAM expression in clear cell carcinoma of the endometrium. Histopathology 72:532–538
van der Putten LJ, Visser NC, van de Vijver K, Santacana M, Bronsert P, Bulten J, Hirschfeld M, Colas E, Gil-Moreno A, Garcia A, Mancebo G, Alameda F, Trovik J, Kopperud RK, Huvila J, Schrauwen S, Koskas M, Walker F, Weinberger V, Minar L, Jandakova E, Snijders MP, van den Berg-van Erp S, Matias-Guiu X, Salvesen HB, Amant F, Massuger LF, Pijnenborg JM (2016) L1CAM expression in endometrial carcinomas: an ENITEC collaboration study. Br J Cancer 115:716–724
van Gool IC, Eggink FA, Freeman-Mills L, Stelloo E, Marchi E, de Bruyn M, Palles C, Nout RA, de Kroon CD, Osse EM, Klenerman P, Creutzberg CL, Tomlinson IP, Smit VT, Nijman HW, Bosse T, Church DN (2015) POLE proofreading mutations elicit an antitumor immune response in endometrial cancer. Clin Cancer Res 21:3347–3355
Meier F, Busch S, Gast D, Goppert A, Altevogt P, Maczey E, Riedle S, Garbe C, Schittek B (2006) The adhesion molecule L1 (CD171) promotes melanoma progression. Int J Cancer 119:549–555
Acknowledgements
The authors thank all participating centers.
Author information
Authors and Affiliations
Contributions
All authors have made a substantial contribution to conception and execution of the study including acquisitions of data, processing of material, analysis and interpretation of data, as well as writing of the manuscript. All authors approve of publication.
Corresponding author
Ethics declarations
The experiments reported here were carried out in agreements with the Declaration of Helsinki principles and in agreement with local legislation at each participating center.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Versluis, M., Plat, A., de Bruyn, M. et al. L1CAM expression in uterine carcinosarcoma is limited to the epithelial component and may be involved in epithelial–mesenchymal transition. Virchows Arch 473, 591–598 (2018). https://doi.org/10.1007/s00428-018-2444-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-018-2444-8