Abstract
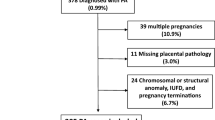
Associations between specific placental histological abnormalities and obstetric outcomes are reported. However, most data are based either on high-risk cases or relate to case–control studies selected from those with abnormal placental histology findings, with the unavoidable biases that these approaches entail. This study reports the frequency of the several common, objective and predefined histological abnormalities of the placenta as identified by pathologists blinded to all clinical information. A total 1,153 women were recruited from an unselected population delivering at 34–43 weeks. Histological findings in common obstetric outcome groups were compared to those of the unselected population, and odds ratios and predictive values were calculated. Normal histological findings were present in 72.1% of pregnancies with normal outcomes and in 79.1%, 66.6%, 80%, and 74.8% of pregnancies affected by pre-eclampsia (PET), pregnancy-induced hypertension (PIH), gestational diabetes (GDM), and small for gestational age (SGA), respectively. Chronic placental underperfusion was seen more frequently in PIH (odds ratio (OR) 2) and SGA (OR 1.4), while villitis of unknown aetiology was observed more commonly in cases with PIH (OR 3.2). Fetal thrombotic vasculopathy was twice as common in cases with GDM whilst massive perivillous fibrin deposition was much more frequent in those with PET (OR 20.2) and SGA (OR 8.9). Chorangiomata were 13 times more common in pregnancies with PET. However, in all cases, positive predictive values were low, with the majority of cases with histological abnormalities being associated with normal outcome. At term, specific placental histological lesions are significantly more common in complicated pregnancies, but the clinical significance of such lesions in a specific case remains uncertain, since the majority will be identified from clinically uncomplicated normal pregnancies.

Similar content being viewed by others
References
Langston C, Kaplan C, Macpherson T, Manci E, Peevy K, Clark B, Murtagh C, Cox S, Glenn G (1997) Practice guideline for examination of the placenta: developed by the Placental Pathology Practice Guideline Development Task Force of the College of American Pathologists. Arch Pathol Lab Med 121:449–476
Hargitai B, Marton T, Cox PM (2004) Best practice no 178. Examination of the human placenta. J Clin Pathol 57:785–792
Khong TY, Gordijn SJ (2003) Quality of placental pathology reports. Pediatr Dev Pathol 6:54–58
Sibai B, Dekker G, Kupferminc M (2005) Pre-eclampsia. Lancet 365:785–799
Macintosh MC, Fleming KM, Bailey JA, Doyle P, Modder J, Acolet D, Golightly S, Miller A (2006) Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: population based study. BMJ 333:177
Garite TJ, Clark R, Thorp JA (2004) Intrauterine growth restriction increases morbidity and mortality among premature neonates. Am J Obstet Gynecol 191:481–487
Zhang P, Schmidt M, Cook L (2006) Maternal vasculopathy and histologic diagnosis of preeclampsia: poor correlation of histologic changes and clinical manifestation. Am J Obstet Gynecol 194:1050–1056
Roberts DJ, Post MD (2008) The placenta in pre-eclampsia and intrauterine growth restriction. J Clin Pathol 61:1254–1260
Daskalakis G, Marinopoulos S, Krielesi V, Papapanagiotou A, Papantoniou N, Mesogitis S, Antsaklis A (2008) Placental pathology in women with gestational diabetes. Acta Obstet Gynecol Scand 87:403–407
Brosens IA, Robertson WB, Dixon HG (1972) The role of the spiral arteries in the pathogenesis of preeclampsia. Obstet Gynecol Annu 1:177–191
Salafia CM, Pezzullo JC, Ghidini A, Lopez-Zeno JA, Whittington SS (1998) Clinical correlations of patterns of placental pathology in preterm pre-eclampsia. Placenta 19:67–72
Sebire NJ, Goldin RD, Regan L (2005) Term preeclampsia is associated with minimal histopathological placental features regardless of clinical severity. J Obstet Gynaecol 25:117–118
Shanklin DR, Sibai BM (1989) Ultrastructural aspects of preeclampsia. I. Placental bed and uterine boundary vessels. Am J Obstet Gynecol 161:735–741
Oliveira LH, Xavier CC, Lanaa M (2002) [Changes in placental morphology of small for gestational age newborns]. J Pediatr (Rio J) 78:397–402
Altemania M, Gonzattia R (2003) [Villitis of unknown etiology in placentas of pregnancies with hypertensive disorders and of small-for-gestational-age infants]. Rev Assoc Med Bras 49:67–71
Pathak S, Hook E, Hackett G, Murdoch E, Sebire NJ, Jessop F, Lees C (2010) Cord coiling, umbilical cord insertion and placental shape in an unselected cohort delivering at term: relationship with common obstetric outcomes. Placenta 31:963–968
Pathak S, Sebire NJ, Hook L, Hackett G, Murdoch E, Jessop F, Lees C (2011) Relationship between placental morphology and histological findings in an unselected population near term. Virchows Arch 459:11–20
Fox H, Sebire NJ (2007) Pathology of the Placenta. W.B.Saunders, London
Davey DA, Macgillivray I (1988) The classification and definition of the hypertensive disorders of pregnancy. Am J Obstet Gynecol 158:892–898
Brown MA, Lindheimer MD, De Swiet M, Van Assche A, Moutquin JM (2001) The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 20:IX–XIV
WHO (2006) World Health Organisation/International Diabetes Federation, definition and diagnosis of diabetes mellitus and intermediate hyperglycemia
http://Www.Healthforallchildren.Co.Uk/. Four-in-one (decimal) growth charts (birth-20 yrs). London: Child Growth Foundation 1996/1
Sebire NJ, Goldin RD, Regan L (2001) Histological chorioamnionitis in relation to clinical presentation at 14–40 weeks of gestation. J Obstet Gynaecol 21:242–245
Fox H (1969) Pathology of the placenta in maternal diabetes mellitus. Obstet Gynecol 34:792–798
Jones CJ, Fox H (1976) Placental changes in gestational diabetes. An ultrastructural study. Obstet Gynecol 48:274–280
Funding
The study was supported by grants from Cambridge Fetal Care and Addenbrooke's Charitable Trust.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Rights and permissions
About this article
Cite this article
Pathak, S., Lees, C.C., Hackett, G. et al. Frequency and clinical significance of placental histological lesions in an unselected population at or near term. Virchows Arch 459, 565–572 (2011). https://doi.org/10.1007/s00428-011-1157-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-011-1157-z