Abstract
Objective
To evaluate the effects of online-supervised versus workplace corrective exercises on neck–shoulder pain (NSP), sick leave, posture, workability, and muscular activity among office workers with the upper crossed syndrome (UCS).
Methods
We performed a parallel-group randomized control trial at Shahid Beheshti University, Tehran, Iran, assigning 36 office workers to online-supervised, workplace, and control groups (mean (SD) age 38.91 ± 3.87, 38.58 ± 7.34, 37.00 ± 8.12). Inclusion criteria were alignment alteration (forward head (≥ 45°), rounding shoulder (≥ 52°), rounding back (≥ 42°), and pain intensity ≥ 3 in neck and shoulder. The two intervention groups performed 8-week exercise program, while the control group continued usual activities. Primary (NSP and sick leave) and secondary outcomes [postural angles, workability, and muscular activity were measured by VAS, outcome evaluation questionnaire (OEQ), photogrammetry, workability index, and EMG, respectively, at the baseline and an 8-week follow-up].
Results
ANCOVA results revealed improvements for the online-supervised group versus control for NSP (P = 0.007), postural angles (P = 0.000, P = 0.001, P = 0.005), workability (P = 0.048, P = 0.042), and upper trapezius activation (P = 0.024, P = 0.016), respectively. Using paired t tests, both intervention groups improved from baseline to follow-up for NSP (P = 0.000, P = 0.002), forward head posture (P = 0.000, P = 0.000), round shoulders (P = 0.001, P = 0.031), and round back (P = 0.034, P = 0.008), respectively. Related parameters of workability (P = 0.041, P = 0.038), upper trapezius (P = 0.005, P = 0.005, P = 0.022), and serratus anterior (P = 0.020, P = 0.015) changed only in the online-supervised group.
Conclusion
Online-supervised corrective exercise seems to improve a range of parameters related to work performance. These findings are highly applicable in light of the ongoing COVID pandemic; many workers have to work from home.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sedentary work is increasingly common in large parts of the world as the nature of work has been changed rapidly because of technology (Buckle and Devereux 2002; Caneiro et al. 2010). Some researchers have proposed that prolonged static postures—e.g., sitting in the same forward-leaned position in front of a computer all the day—may cause postural malalignment and be considered as a risk factor for work-related musculoskeletal disorders (WMSDs), leading to office workers’ complaints (Szeto et al. 2005; So et al. 2019). Janda believed that sustained awkward positions could very likely lead to transformation in the head, shoulder, and spinal curves, causing forward head posture, round shoulders, and round back, anteriorly tilt, and winged scapula (Morris et al. 2006; Zad and Patil 2021). Such conditions are postulated to result in constant pressure and degenerative changes in an individual's joints, and are simultaneously associated with musculoskeletal imbalance and pain (Barrett et al. 2016; Isper Garbin et al. 2017). Based on the literature, neck and shoulder impairments, headaches, chronic neck tension, and scapular dyskinesia could negatively influence workability and typical daily performance (Singla and Veqar 2017).
Furthermore, many studies have reported approximately 50.5% and 44.8% of the prevalence of shoulder and upper back pain among office workers (Madeleine et al. 1999; Kaliniene et al. 2016; Hasan et al. 2020). Computer users reported musculoskeletal discomforts symptoms 68% in the neck, 66% in the back, and 45% in the shoulder (Ardahan and Simsek 2016). In 2014, among Iranian office workers, Nejati et al. published a high prevalence of UCS symptoms containing forward head posture, round shoulders, and round back as 61.3, 48.7, and 78.3%, respectively (Nejati et al. 2014). Meanwhile, Noroozi et al. stated that office workers have a high prevalence of musculoskeletal disorders, since prolonged sitting and working with computers are some of the causes for these individuals to experience musculoskeletal disorders increasing the risks relatively (Noroozi et al. 2015). However, high-quality research based on prospective cohort studies found no association between the computer use and the risk of chronic neck and shoulder pain (Andersen et al. 2008). Thus, it is why only certain individuals are prone to develop UCS. It has been approved previously that increasing pain intensity, regardless of its cause, decreases the workability among sedentary and physical work demands (Bayattork et al. 2019). Due to musculoskeletal symptoms imposing indirect costs including sick leave, productivity loss, treatment costs, disability, early retirement, and work absenteeism in office workers, the issues such as lifestyle interventions, identification of the groups at the risk of disability, increased health promotion, and early prevention in the workplace could be assumed as great potential for increasing workability and reducing work absenteeism (Sundstrup et al. 2020). Other risk factors influencing the productivity and workability in the working environment may be related to personal, organizational, social, and environmental factors, including noise, lighting, temperature, and the like, often leading to economic losses (Lister et al. 1998; Welch et al. 2020).
Additionally, UCS is characterized by tightening upper trapezius and sternocleidomastoid following the deep cervical flexors and middle, lower trapezius, and serratus anterior muscles’ weakness (Page 2011a, b; Ohlendorf et al. 2017). It may cause alteration in scapula muscle activation, movement patterns, and some misalignments in the upper limb that simultaneously contribute to cervicothoracic and glenohumeral joint dysfunction (Culham and Peat 1993; Seidi et al. 2020). Acting as a bridge between the shoulder and cervical region, the scapula plays a significant role in providing mobility and stability for the neck and shoulders (Cools et al. 2014).
Previous studies also indicated the relationship between chronic NSP and scapular dyskinesis by altering dynamic scapular stability during the scapular orientation in the resting position and also reported that neck pain may alter postural behavior when performing prolonged sitting tasks, such as during computer use (Szeto et al. 2002; Cagnie et al. 2014). Furthermore, increased cervical and thoracic curves and a slouched posture are known to affect scapular orientation, shoulder muscle strength, and shoulder range of motion (Kebaetse et al. 1999; Finley and Lee 2003; Kibler 2003). Many studies have determined impaired muscle coordination in the neck muscles, cervical pain, and abnormal head position associated with high amounts of EMG activity in the neck flexors’ muscles, and have highlighted a direct correlation among upper trapezius muscle activity, neck angle, and perceived discomfort during the prolonged sitting tasks (Falla et al. 2004, Berolo et al. 2011; Pietropaoli et al. 2019; D’Anna et al. 2021). Brandt et al. reported a strong association between perceived NSP intensity and trapezius muscle tenderness among the office workers (Brandt et al. 2014).
Based on the previous findings, serratus anterior and lower trapezius provide stability for the scapula and maintain the appropriate scapular location to act as an essential shoulder stabilizer and balance the scapular rotation coupling forces (Johnson et al. 1994; Phadke et al. 2009; Weon et al. 2010). Consequently, altered stability of the scapula may create or sustain symptomatic mechanical dysfunction in the cervical spine and influence the neck pain’s recurrence (Helgadottir et al. 2011). Meanwhile, disturbances in scapular function could be found in both shoulder and neck pain due to the neuromuscular imbalance between the deep phasic and superficial tonic muscles. This phenomenon is worth considering for effective management of UCS among office workers (Page et al. 2010; Page 2011a, b). In this regard, Cools et al. suggested a basic rehabilitation approach focused on the office workers' functional demands, like correcting the function of axioscapular muscles and scapular alignment during the prolonged upper extremities activities (Cools et al. 2014). Hence, implementing posture-correction strategies early in the rehabilitation program, performing all interventions in a sitting or standing position with a correct posture, and maintaining an upright body position to retrain a neutral posture are considered different techniques for reducing chronic neck pain (Falla et al. 2007; Lee, Lee et al. 2017).
Although several studies investigated the efficiency of workplace interventions for rehabilitation or prevention of WMSDs as a global health issue, which influences both employers and employees, an effective intervention is still needed to be warranted (Skamagki et al. 2018; Grimani et al. 2019; Ting et al. 2019; Welch et al. 2020).
UCS symptoms may alter muscle activation patterns, which can be considered one of the most potent stimuli to central motor programming (Madeleine et al. 1999; Brandt et al. 2014; Gu et al. 2016). Furthermore, muscle activation alterations were observed in office workers suffering frequent pain in the shoulder and neck and poor postural stability, respectively (Jull et al. 2004; Andersen et al. 2011; Sterling 2011). In this population, postural malalignments and altered muscle activation are associated with work disability and sickness absence (Loghmani et al. 2013).
Due to lack of research on computer users suffering from UCS, it seems rational to evaluate associated various musculoskeletal symptoms, including forward head posture, round shoulders, and round back along with related muscles’ EMG influenced by UCS, and pain in neck and shoulder areas, as well as assessing the extent of workability and sick-leave variables in such populations. Although most research reported positive effects of supervised and un-supervised interventions in managing WMSDs, some studies underlined that supervised exercise programs are most likely to be beneficial in maintenance and adherence and, as a result, significantly influence diminishing consequential symptoms (Blangsted et al. 2008; Coury et al. 2009). Conversely, implementing exercise under supervision can be cost-effective and not always an available workplace resource; however, some individuals prefer to exercise when it fits into their daily working routine (Gram et al. 2014). Since many countries worldwide have applied social quarantine during the COVID-19 global pandemic, office workers were advised to work from home and follow the rules of social distance (Aegerter et al. 2021). Nevertheless, evidence-based guidelines for performing home exercise are lacking. The current study is the first randomized controlled trial with the purpose of comparing the effect of corrective exercises at the worksite versus home under direct supervision during the pandemic.
In more detail, it is hypothesized that performing corrective exercises diminishes UCS-related symptoms, including work parameters, postural malalignment, and imbalanced muscles in office workers with NSP. The primary objectives were to assess the effects of an 8-week online-supervised home-based versus workplace-based corrective exercises to decrease NSP and sick leave. The secondary objectives were to evaluate postural angles (forward head posture, round shoulders, and round back), workability, and the surface EMG of interest muscles (upper, middle, lower trapezius, sternocleidomastoid, and serratus anterior) among the computer users working at the offices with UCS.
Methods
Study design and participants
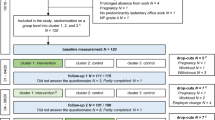
A parallel-group randomized controlled trial with testing at baseline and follow-up was approved by Ethics Committee on the Research at Shahid Beheshti University, Tehran, Iran (approval number: IR.SBU.REC.1399.036/2020.06.20). The trial was registered at IRCT (IRCT20200729048249N1/2020.10.05). The assessments were conducted at baseline and after 8 weeks of intervention in the Sport Sciences and Health Laboratory at Shahid Beheshti University, Tehran, Iran. The subjects signed an informed consent followed by the Declaration of Helsinki. They were randomly assigned to three groups; the intervention groups (online-supervised and workplace) and the control group. Figure 1 demonstrates the whole procedure according to CONSORT guidelines to ensure the transparent and standardized reporting of the trial (Grant et al. 2018). The study protocol has been published, and all detailed procedures have already been presented elsewhere (Yaghoubitajani et al. 2021).
The entire study procedure, including assessments, was clarified for 118 volunteers who were invited through invitation letters. Qualified office workers, including 23 females and 13 males, were performed the pre-test, and they were all able to meet the eligibility criteria with postural alterations (forward head posture ≥ 45°, round shoulders ≥ 52°, round back ≥ 42°) and pain intensity (≥ 3) in the neck and shoulder areas, measured by photogrammetry and VAS, respectively. Based on the above inclusion criteria, the individuals were excluded from the list of participants if they were pregnant, had a history of joint diseases in the spine, shoulder, pelvis, and fracture, had surgery during the past year, or had a bodyweight out of the normal range (18 ≥ BMI ≥ 25). The subjects were considered as dropouts if they missed three sequential sessions or the follow-up test. For their convenience, the subjects were permitted to leave the study at any stage of the research process.
Study outcomes and assessments
The main researcher measured the study outcomes at the baseline before randomization and after 8 weeks. The NSP and sick leave as the primary outcomes were measured by VAS and OEQ, respectively. The secondary outcomes, including postural alignment angles (forward head posture, round shoulders, and round back), workability (physical and mental), muscle activation, and timing of the interested muscles (upper, middle, lower trapezius, sternocleidomastoid, and serratus anterior), were assessed by photogrammetry, workability index questionnaire, and EMG, respectively. Demographic data were obtained, including age, weight, height, BMI, smoking behavior, marital status, and education level. The baseline and follow-up tests were conducted using assessment methods and testing equipment in the same setting.
Data were collected on the paper questionnaires using a 10-cm VAS scale; the subjects rated their NSP intensity, ranging from zero (“no pain”) to ten (“worst pain”). The sick leave was assessed by a single item extracted from OEQ of the validated outcome. The response categories ranged from 0 to 31 days, inserting the number of absence working days due to NSP within the past month (Keefe et al. 1992; Hallman et al. 2019). Self-reported sick leave demonstrates good test–retest reliability and sufficient convergent validity against records (Miraglia and Johns 2016). The photogrammetric method was applied for the postural angles’ assessments by identifying anatomical landmarks of the tragus, acromion process of the scapula, spinous process of C-7 and T-12 through removable colored dots to be laterally visible (Karimian et al. 2019). Workability was evaluated by self-report using a single validated item from the Workability Index questionnaire. The scores ranged from 0 to 10 (0 = completely unable to work, 10 = workability at its best), indicating a cut-off point score of ≤ 7, implying the poor workability (Gram et al. 2012; Hallman et al. 2019).
The EMG recordings were made through the standard procedure to normalize the recommended range in work-related disorder studies for activation and timing of upper, middle, and lower trapezius, sternocleidomastoid, and serratus anterior muscles. Careful skin preparation followed based on SENIAM and previously published guidelines concerning the skin impedance (≤ 10 kΩ) and bipolar Ag/AgCl (SKINTACT, Austria) surface electrodes’ application (Johnston et al. 2008). The ME-6000 Megawin (MegaWin, Finland) was used for data collection, and all EMG signals were amplified (gain, 1000), passed through a 10–500 Hz band-width filter, and sampled at 1000 Hz processed through the Matlab software (Seidi et al. 2020). The maximal voluntary isometric test (MVIC) was performed and normalized the EMG data. After training and a short warm-up, the subjects implemented three MVICs holdings for 5 s against the manual static resistance. The duration was controlled by a stopwatch considering 30 s rest time between each repetition and 2 min for subsequent muscle testing. Those subjects who reported pain during the test were excluded to minimize the impact of pain on the assessment. After five minutes of resting, the subjects performed bilateral arm elevation five times in the scapular plane over concentric, isometric, and eccentric phases, which lasted 3 s as well as 3 s of rest between each phase. After rectifying and smoothing, the root mean square (RMS) was calculated at the time constant of 50 ms for 3 s from the middle of three trials out of five. The RMS mean was divided using MVIC value, and was multiplied by 100 to calculate the muscle activity percentage (Arshadi et al. 2019). The muscle activation onset/offset was calculated based on concentric/eccentric phases from the point that the level of muscle activity reached three standard deviations above/below the rest of the muscle activity and then was analyzed based on the middle deltoid onset/offset timing (De Mey et al. 2012).
Randomization
The computer-generated block randomization was performed in a 1:1:1 allocation ratio through the website https://www.sealedenvelope.com. The main investigator performed the enrollment, generated the random allocation sequence, and assigned the subjects to the groups. The random allocation sequence was implemented by concealed, sequentially numbered, sealed, and opaque envelopes by putting a card inside, indicating that the allocated group to each subject was randomly executed. A university assistant professor supervised all procedures, including the sequence generation process and allocation concealment mechanism, to ensure that the assignment schedule was unpredictable.
Intervention
Intervention groups performed 8-week corrective exercises three times/week, lasting about 50–60 min pertaining to typical 5-min warm-up and cool-down. Each exercise was individualized based on demographic characteristics, pain intensity, and overload principles. The pain intensity up to five (VAS) was allowed to have ten max. repetition, only if the pain decreased immediately after completing the exercise. The subjects who experienced the higher pain levels could modify the exercise accordingly.
The online-supervised group performed the program under direct remote supervision in their home environment using desktop videoconferencing software (https://meet.jit.si/). To do so, a laptop monitored by a qualified corrective exercises expert was utilized to ensure the progress movement pattern and the control load progression. The workplace group who performed the program in their worksite was provided a diary with detailed written and pictorial descriptions. In addition to telephone interviews, the expert's weekly presence was accentuated to evaluate the progress, safety, and performance constantly.
The exercise program was prescribed concerning spontaneous postural alterations, muscle activation, movement pattern, and lack of scapula stabilization for the individuals with UCS suffering from NSP. A detailed pictorial description of the interventions, along with the list of the given corrective exercises to both interventional groups, is available elsewhere (Yaghoubitajani et al. 2021).
Sample size and statistical analysis
The G × Power software (Version 3.0.10, Germany) was used to calculate the sample size regarding the effect size reported for the corrective exercises compared with the control group without any intervention in a similar study, totally (n = 33). To avoid potential dropout during the study, a total of 45 subjects were considered adequate to compensate for the potential loss to follow-up; however, we achieved only 36 subjects due to recruitment difficulties related to the COVID pandemic, i.e., we assigned 12 subjects to each group (Yaghoubitajani et al. 2021). The analyses were conducted using IBM SPSS version 20 for Windows (SPSS Inc., Chicago, IL, USA). Variables' distribution was examined by the Shapiro–Wilk (P ≥ 0.05). Paired t test and one-way ANCOVA were used for within-group and between-group comparisons. The follow-up values were used as the outcome while controlling the baseline values. The M ± SD and the significance levels at P ≤ 0.05 were applied for data demonstration. The partial η2 method was utilized to determine the effect size of the differences' magnitude as small (0.01 ≤ η2 < 0.06), medium (0.06 ≤ η2 < 0.14), or large (η2 ≥ 0.14) (Richardson 2011). For the minimum clinically important differences, the formula of (MCID = SD × 0.5) was used (Norman et al. 2003).
Results
The assessments were implemented among 36 subjects, and the study outcomes were analyzed for the original assigned three groups. Table 1 demonstrates baseline demographic and lifestyle characteristics. All variables had normal distribution based on Shapiro–Wilk test (P ≥ 0.05).
Within-group comparison using paired t tests demonstrated significant differences in both online-supervised and workplace groups for NSP (P = 0.000, P = 0.002), forward head posture (P = 0.000, P = 0.000), round shoulders (P = 0.001, P = 0.031), and round back (P = 0.034, P = 0.008), respectively. The online-supervised group differed in physical and mental workability variables (P = 0.041, P = 0.038). Also, in this group, the upper trapezius improved in Max., Ave. activation (P = 0.005, P = 0.005), and offset timing (P = 0.022). Serratus anterior indicated Max. and Ave. activation changes (P = 0.020, P = 0.015), respectively.
Using ANCOVA for comparing between-groups, the results revealed significant differences in the online-supervised group NSP (P = 0.007) in pairwise comparisons with the control group. Significant differences were observed in postural angles, including forward head posture (P = 0.000) comparing control with online-supervised and workplace groups, round shoulders (P = 0.001) between control and online-supervised groups, and round back (P = 0.005) between control and workplace groups. In addition, comparing between control and online-supervised groups, physical and mental workability (P = 0.048, P = 0.042), and upper trapezius muscle Max., Ave. activation (P = 0.024, P = 0.016) differed significantly. The sick leave and other variables were not the cases in all three groups (P ≥ 0.05). Tables 2 and 3 display within-group and between-group significant differences along with the magnitude effect sizes in study outcomes' improvement at the follow-up, and the MCIDs changes in the intervention groups, respectively.
Discussion
The present study found that online-supervised corrective exercises seem to be effective in improving a range of parameters related to work performance, since significant differences occurred in the two intervention groups.
These findings are highly relevant in light of the ongoing COVID pandemic, where many workers have to work from home.
The findings confirmed that performing 8-week corrective exercises significantly affected the NSP among the subjects in the two intervention groups. This is in line with the previous findings, showing that corrective exercises improve neck pain (Sheikhhoseini et al. 2018; Mehri et al. 2020). Some studies reported that prolonged sitting or improper neck and shoulder posture during work might be associated with NSP among office workers (Falla al. 2007; Lee et al. 2017). Neck pain is associated with the ability to maintain an upright posture, as reported previously, and there could be a relationship between the correction of forward head posture, round shoulders, and pain (Lynch et al. 2010). In this regard, Lee et al. suggested that maintaining an upright body position and implementing posture-correction strategies in different sitting positions can prevent musculoskeletal pain (Cools et al. 2014; Lee et al. 2017). Hence, all the subjects were initially informed about the UCS consequences; hence, their postural awareness was repeatedly developed throughout the study days, and frequent corrections to an upright neutral postural position were recommended focusing on the control system in postural re-education programs such as memory joggers, to ensure that those behaviors become kinds of habit (Abdollahzade et al. 2017).
Furthermore, muscle strengthening or endurance exercises are recommended for an incorrect posture leading to pain through increased load on the cervical spine and changing the muscle’s length (Gram et al. 2012). Meanwhile, training and rehabilitation of power and endurance of the deep neck flexors have been previously proved to be beneficial for restoring neuromuscular imbalance and cervical stabilization, where the present study highlighted relevant exercises (Falla et al. 2007; Lee et al. 2018). Considering that the scapula plays an important role in NSP and is the keystone of the UCS, the current study primarily focused on the function of the scapula muscles to restore and balance the scapula stabilizers. This phenomenon could be due to activating the neck muscles and reducing the compensatory movements of the muscles involved in the area (Cagnie et al. 2014; Cools al. 2014; Kang et al. 2021).
Our findings significantly affected the postural angles. Since the alteration in the resting scapular position may occur with the abnormal cervical and thoracic spine alignment, the forward head posture can result in round shoulders, which may cause enhancing thoracic kyphotic posture, respectively (Kwon et al. 2015; Lee et al. 2015). Based on the literature, there might be a relationship among the forward head posture, round shoulders, and round back; however, the studies revealed an improvement in response to training programs' exercises (Singla and Veqar 2017; Sheikhhoseini et al. 2018). It is supposed that the involved muscles in the UCS may be shortened or lengthened when they are remained in the improper posture for a long time, occurring adaptive lengthening or shortening over time leading to poor posture. The traditional approach has focused on improving malalignments by stretching the shortened and strengthening the weakened muscles. However, using stretching exercises, some studies reported no changes in the muscle length, but indicated improved tolerance to stretching (Magnusson 1998; Sahrmann et al. 2017).
In contrast, the functional approach states that the interactions among all central and peripheral nervous systems, muscular and skeletal structures are the cause of WMSDs (Hamill et al. 1999). Thus, the initial strategy containing posture, muscle activation, and movement pattern intervention is recommended to be more effective (Hodges, Van Dieën et al. 2019). It seems that focusing simultaneously on the neural and muscular components for improving postural malalignments brings about the best results if the intervention is applied at least six weeks with an average of three times a week and a duration of 15–60 min (Bayattork et al. 2020).
The upper trapezius significantly improved in the current study, while no alterations were found in other muscles. The results are to some extent in line with the previous findings of Arshadi et al., conducted among healthy men with the UCS. They reported in their experiment that an 8-week corrective exercise exhibits significant differences in EMG activity of sternocleidomastoid, upper trapezius, serratus anterior; though middle and lower trapezius activity revealed no changes (Arshadi et al. 2019).
Meanwhile, Seidi et al. detected significant differences in the middle, lower trapezius, and serratus anterior activation levels. The young males with no pain performed a comprehensive corrective exercise program; nevertheless, the muscle activation timing indicated no specific differences. In the current study, upper trapezius offset timing varied in the online-supervised group (Seidi et al. 2020). Concerning the muscle activation timing, Cools et al. supported the theory that the individuals with pain may have delayed onset of middle and lower trapezius muscle activity, and injured individuals show abnormal muscle recruitment patterns in the same muscles. The timing of muscle activation is an essential factor in coordination with the scapula and arm movement (Cools et al. 2003).
Due to the presence of a neuromuscular imbalance in the UCS needing sensory–motor function, muscle adaptation to resistance training could happen before the development of hypertrophy, influencing more motor units, learning to use active motor units more effectively, and reducing the inhibitory inputs of alpha motor neurons (Hakkinen 1994).
In our study, the upper trapezius was the only muscle that displayed activation levels decrease. This outcome was in line with the findings of the studies that evaluated the upper trapezius activity among the office workers. It is worth noting that the muscle activation can be occurred by the neural adaptations associated with short-term exercise or may be connected with reduced pain levels rather than a direct result of the exercise program (Lidegaard et al. 2013; Villanueva et al. 2020). In this regard, Andersen et al. described these phenomena in their “wheel of pain reduction” and concluded that specific strength after exercise relieves pain and maximizes the activity, particularly in painful trapezius muscles. Increasing shoulder abduction strength in women with trapezius myalgia and reducing relative workload may indirectly decrease pain (Andersen et al. 2009). Consequently, the diminished upper trapezius activation levels prove this issue as the only trapezius muscle part, which is often overactive in the subjects with UCS. Then, its lesser activation might lead to pain relief (Kwon et al. 2015).
During this research, the applied intervention improved mental and physical workability in the online-supervised group, which was consistent with the study of Gram et al. However, no statistical differences were found for the sick leave as a fundamental problem when the individuals are going to work with pain (Gram et al. 2012). Musculoskeletal pain may negatively affect workability and physical activity, making significant differences in sedentary behavior, productivity, and work absenteeism associated with NSP (Foley et al. 2016, Hallman et al. 2019).
Limitations
The current study’s intervention duration can be considered a limitation, since UCS influencing scapular muscles’ activation may need more time to achieve the appropriate recruitment, timing, and firing rates. Although postural alignment and pain improvements occur sooner, the upper trapezius has started to change. Thus, more comprehensive studies are required to manage the UCS as a sensory–motor disorder due to neuromuscular adaptation. Another limitation of the current study was a relatively small sample size, which was selected to recruit the subjects in COVID-19 conditions. Although the study had sufficient statistical capability to show apparent differences between corrective exercises and the control conditions, it was not powerful enough to compare the two active interventions. However, the main finding of the present study—i.e., that online-supervised corrective exercises are effective—remains relevant to similar types of subjects with UCS. Eventually, a lack of blinding in the study design could be assumed as another unachievable limitation with the exercise interventions.
Conclusion
Implementing an 8-week corrective exercises program resulted in clinically desired significant improvements in most study outcomes. The findings in the online-supervised group revealed significant changes, which confirm that the supervised intervention could be more effective than the un-supervised intervention. However, it seems very difficult to compare the consequences of the current study with those of others. The reason is that previous research with similar titles evaluated the effects of various exercises on different study populations with different outcome measures, which makes it challenging to interpret the results. In the present study, the magnitude of the effect sizes in intervention groups indicated that prescribed corrective exercises positively affect NSP, forward head posture, round shoulders, round back, workability, and restored upper trapezius muscle activity. Based on the findings, it is suggested to perform the training under direct supervision rather than alone and without any supervision. Furthermore, WMSDs impose indirect costs, including productivity loss, treatment costs, and disability. Hence, managing the UCS is highly recommended among office workers, particularly the computer users with NSP, to increase health conditions and early prevention in the workplace, which in turn could significantly increase workability. However, it is worth noting this issue when the individuals go to work when experiencing pain.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. The researchers interested in using the final dataset for scientific purposes may contact the corresponding author.
References
Abdollahzade Z, Shadmehr A, Malmir K, Ghotbi N (2017) Effects of 4 week postural corrective exercise on correcting forward head posture. J Mod Rehabilit 11(2):85–92
Aegerter AM, Deforth M, Sjøgaard G, Johnston V, Volken T, Luomajoki H, Dratva J, Dressel H, Distler O, Melloh M (2021) No evidence for a decrease in physical activity among swiss office workers during Covid-19: a longitudinal study. Front Psychol. https://doi.org/10.3389/fpsyg.2021.620307
Andersen LL, Andersen JL, Suetta C, Kjær M, Søgaard K, Sjøgaard G (2009) Effect of contrasting physical exercise interventions on rapid force capacity of chronically painful muscles. J Appl Physiol 107(5):1413–1419. https://doi.org/10.1152/japplphysiol.00555.2009
Andersen LL, Hansen K, Mortensen OS, Zebis MK (2011) Prevalence and anatomical location of muscle tenderness in adults with nonspecific neck/shoulder pain. BMC Musculoskelet Disord 12(1):1–8. https://doi.org/10.1186/1471-2474-12-169
Andersen JH, Harhoff M, Grimstrup S, Vilstrup I, Lassen CF, Brandt LP, Kryger AI, Overgaard E, Hansen KD, Mikkelsen S (2008) Computer mouse use predicts acute pain but not prolonged or chronic pain in the neck and shoulder. Occup Environ Med 65(2):126–131. https://doi.org/10.1136/oem.2007.033506
Ardahan M, Simsek H (2016) Analyzing musculoskeletal system discomforts and risk factors in computer-using office workers. Pak J Med Sci 32(6):1425. https://doi.org/10.12669/pjms.326.11436
Arshadi R, Ghasemi GA, Samadi H (2019) Effects of an 8-week selective corrective exercises program on electromyography activity of scapular and neck muscles in persons with upper crossed syndrome: randomized controlled trial. Phys Ther Sport 37:113–119. https://doi.org/10.1016/j.ptsp.2019.03.008
Barrett E, O’Keeffe M, O’Sullivan K, Lewis J, McCreesh K (2016) Is thoracic spine posture associated with shoulder pain, range of motion and function? A systematic review. Man Ther 26:38–46. https://doi.org/10.1016/j.math.2016.07.008
Bayattork M, Jakobsen MD, Sundstrup E, Seidi F, Bay H, Andersen LL (2019) Musculoskeletal pain in multiple body sites and work ability in the general working population: cross-sectional study among 10,000 wage earners. Scand J Pain 19(1):131–137. https://doi.org/10.1515/sjpain-2018-0304
Bayattork M, Sköld MB, Sundstrup E, Andersen LL (2020) Exercise interventions to improve postural malalignments in head, neck, and trunk among adolescents, adults, and older people: systematic review of randomized controlled trials. J Exerc Rehabilit 16(1):36. https://doi.org/10.12965/jer.2040034.017
Berolo S, Wells RP, Amick BC III (2011) Musculoskeletal symptoms among mobile hand-held device users and their relationship to device use: a preliminary study in a Canadian university population. Appl Ergon 42(2):371–378. https://doi.org/10.1016/j.apergo.2010.08.010
Blangsted AK, Søgaard K, Hansen EA, Hannerz H, Sjøgaard G (2008) One-year randomized controlled trial with different physical-activity programs to reduce musculoskeletal symptoms in the neck and shoulders among office workers. Scand J Work, Environ Health. https://doi.org/10.5271/sjweh.1192
Brandt M, Sundstrup E, Jakobsen MD, Jay K, Colado JC, Wang Y, Zebis MK, Andersen LL (2014) Association between neck/shoulder pain and trapezius muscle tenderness in office workers. Pain Res Treat. https://doi.org/10.1155/2014/352735
Buckle PW, Devereux JJ (2002) The nature of work-related neck and upper limb musculoskeletal disorders. Appl Ergon 33(3):207–217. https://doi.org/10.1016/s0003-6870(02)00014-5
Cagnie B, Struyf F, Cools A, Castelein B, Danneels L, O’leary S (2014) The relevance of scapular dysfunction in neck pain: a brief commentary. J Orthop Sports Phys Ther 44(6):435–439. https://doi.org/10.2519/jospt.2014.5038
Caneiro JP, O’Sullivan P, Burnett A, Barach A, O’Neil D, Tveit O, Olafsdottir K (2010) The influence of different sitting postures on head/neck posture and muscle activity. Man Ther 15(1):54–60. https://doi.org/10.1016/j.math.2009.06.002
Cools AM, Struyf F, De Mey K, Maenhout A, Castelein B, Cagnie B (2014) Rehabilitation of scapular dyskinesis: from the office worker to the elite overhead athlete. Br J Sports Med 48(8):692–697. https://doi.org/10.1136/bjsports-2013-092148
Cools AM, Witvrouw EE, Declercq GA, Danneels LA, Cambier DC (2003) Scapular muscle recruitment patterns: trapezius muscle latency with and without impingement symptoms. Am J Sports Med 31(4):542–549. https://doi.org/10.1177/03635465030310041101
Coury HJ, Moreira RF, Dias NB (2009) Evaluation of the effectiveness of workplace exercise in controlling neck, shoulder and low back pain: a systematic review. Braz J Phys Ther 13:461–479. https://doi.org/10.1590/S1413-35552009000600002
Culham E, Peat M (1993) Functional anatomy of the shoulder complex. J Orthop Sports Phys Ther 18(1):342–350. https://doi.org/10.2519/jospt.1993.18.1.342
D’Anna C, Schmid M, Conforto S (2021) Linking head and neck posture with muscular activity and perceived discomfort during prolonged smartphone texting. Int J Ind Ergon 83:103134. https://doi.org/10.1016/j.ergon.2021.103134
De Mey K, Danneels L, Cagnie B, Cools AM (2012) Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: effect of a 6-week training program on muscle recruitment and functional outcome. Am J Sports Med 40(8):1906–1915. https://doi.org/10.1177/0363546512453297
Falla DL, Jull GA, Hodges PW (2004) Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine 29(19):2108–2114. https://doi.org/10.1097/01.brs.0000141170.89317.0e
Falla D, Jull G, Russell T, Vicenzino B, Hodges P (2007) Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther 87(4):408–417. https://doi.org/10.2522/ptj.20060009
Finley MA, Lee RY (2003) Effect of sitting posture on 3-dimensional scapular kinematics measured by skin-mounted electromagnetic tracking sensors. Arch Phys Med Rehabilit 84(4):563–568. https://doi.org/10.1053/apmr.2003.50087
Foley B, Engelen L, Gale J, Bauman A, Mackey M (2016) Sedentary behavior and musculoskeletal discomfort are reduced when office workers trial an activity-based work environment. J Occup Environ Med 58(9):924–931. https://doi.org/10.1097/JOM.0000000000000828
Gram B, Andersen C, Zebis MK, Bredahl T, Pedersen MT, Mortensen OS, Jensen RH, Andersen LL, Sjøgaard G (2014) Effect of training supervision on effectiveness of strength training for reducing neck/shoulder pain and headache in office workers: cluster randomized controlled trial. BioMed Res Int. https://doi.org/10.1155/2014/693013
Gram B, Holtermann A, Bültmann U, Sjøgaard G, Søgaard K (2012) Does an exercise intervention improving aerobic capacity among construction workers also improve musculoskeletal pain, work ability, productivity, perceived physical exertion, and sick leave?: a randomized controlled trial. J Occup Environ Med 54(12):1520–1526. https://doi.org/10.1097/JOM.0b013e318266484a
Grant S, Mayo-Wilson E, Montgomery P, Macdonald G, Michie S, Hopewell S, Moher D (2018) CONSORT-SPI 2018 explanation and elaboration: guidance for reporting social and psychological intervention trials. Trials 19(1):1–18. https://doi.org/10.1186/s13063-018-2735-z
Grimani A, Aboagye E, Kwak L (2019) The effectiveness of workplace nutrition and physical activity interventions in improving productivity, work performance and workability: a systematic review. BMC Pub Health 19(1):1–12. https://doi.org/10.1186/s12889-019-8033-1
Gu S-Y, Hwangbo G, Lee J-H (2016) Relationship between position sense and reposition errors according to the degree of upper crossed syndrome. J Phys Ther Sci 28(2):438–441. https://doi.org/10.1589/jpts.28.438
Hakkinen K (1994) Neuromuscular adaptation during strength training, ageing, detraining, and immobilization. Crit Rev Phys Rehabilit Med 14:161–198
Hallman DM, Holtermann A, Dencker-Larsen S, Jørgensen MB, Rasmussen CDN (2019) Are trajectories of neck–shoulder pain associated with sick leave and work ability in workers? A 1-year prospective study. BMJ Open 9(3):e022006. https://doi.org/10.1136/bmjopen-2018-022006
Hamill J, van Emmerik RE, Heiderscheit BC, Li L (1999) A dynamical systems approach to lower extremity running injuries. Clin Biomech 14(5):297–308. https://doi.org/10.1016/s0268-0033(98)90092-4
Hasan NH, Zulkifly SS, Ali NM (2020) The risks of work-related musculoskeletal disorders among business service center workers. J Occup Saf Health 17(No2):21
Helgadottir H, Kristjansson E, Einarsson E, Karduna A, Jonsson H Jr (2011) Altered activity of the serratus anterior during unilateral arm elevation in patients with cervical disorders. J Electromyogr Kinesiol 21(6):947–953. https://doi.org/10.1016/j.jelekin.2011.07.007
Hodges PW, Van DJH, Cholewicki J (2019) Time to reflect on the role of motor control in low back pain. J Orthop Sports Phys Ther 49(6):367–369. https://doi.org/10.2519/jospt.2019.0104
Isper Garbin AJ, Soares GB, Arcieri RM, Saliba Garbin CA, Siqueira CE (2017) Musculoskeletal disorders and perception of working conditions: a survey of Brazilian dentists in São Paulo. Int J Occup Med Environ Health. https://doi.org/10.13075/ijomeh.1896.00724
Johnson G, Bogduk N, Nowitzke A, House D (1994) Anatomy and actions of the trapezius muscle. Clin Biomech 9(1):44–50. https://doi.org/10.1016/0268-0033(94)90057-4
Johnston V, Jull G, Souvlis T, Jimmieson NL (2008) Neck movement and muscle activity characteristics in female office workers with neck pain. Spine 33(5):555–563. https://doi.org/10.1097/BRS.0b013e3181657d0d
Jull G, Kristjansson E, DallAlba P (2004) Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther 9(2):89–94. https://doi.org/10.1016/S1356-689X(03)00086-9
Kaliniene G, Ustinaviciene R, Skemiene L, Vaiciulis V, Vasilavicius P (2016) Associations between musculoskeletal pain and work-related factors among public service sector computer workers in Kaunas County, Lithuania. BMC Musculoskelet Disord 17(1):1–12. https://doi.org/10.1186/s12891-016-1281-7
Kang NY, Im SC, Kim K (2021) Effects of a combination of scapular stabilization and thoracic extension exercises for office workers with forward head posture on the craniovertebral angle, respiration, pain, and disability: a randomized-controlled trial. Turk J Phys Med Rehabilit 67(3):291. https://doi.org/10.5606/tftrd.2021.6397
Karimian R, Rahnama N, Ghasemi G, Lenjannejadian S (2019) Photogrammetric analysis of upper cross syndrome among teachers and the effects of national academy of sports medicine exercises with ergonomic intervention on the syndrome. J Res Health Sci 19(3):e00450
Kebaetse M, McClure P, Pratt NA (1999) Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Medicine Rehabilit 80(8):945–950. https://doi.org/10.1016/s0003-9993(99)90088-6
Keefe FJ, Linton SJ, Lefebvre JC (1992) The Outcome evaluation questionnaire: description and initial findings. Cogn Behav Ther 21(1):19–33. https://doi.org/10.1080/16506079209455886
Kibler WB (2003) Rehabilitation of rotator cuff tendinopathy. Clin Sports Med 22(4):837–847. https://doi.org/10.1016/s0278-5919(03)00048-6
Kwon JW, Son SM, Lee NK (2015) Changes in upper-extremity muscle activities due to head position in subjects with a forward head posture and rounded shoulders. J Phys Ther Sci 27(6):1739–1742. https://doi.org/10.1589/jpts.27.1739
Lee J-H, Cynn H-S, Yi C-H, Kwon O-Y, Yoon T-L (2015) Predictor variables for forward scapular posture including posterior shoulder tightness. J Bodyw Mov Ther 19(2):253–260. https://doi.org/10.1016/j.jbmt.2014.04.010
Lee S, Lee Y, Chung Y (2017) Effect of changes in head postures during use of laptops on muscle activity of the neck and trunk. Phys Ther Rehabilit Sci 6(1):33–38. https://doi.org/10.14474/ptrs.2017.6.1.33
Lee J, Kim D, Yu K, Cho Y, You JH (2018) Comparison of isometric cervical flexor and isometric cervical extensor system exercises on patients with neuromuscular imbalance and cervical crossed syndrome associated forward head posture. Bio-Med Mater Eng 29(3):289–298. https://doi.org/10.3233/BME-181728
Lidegaard M, Jensen RB, Andersen CH, Zebis MK, Colado JC, Wang Y, Heilskov-Hansen T, Andersen LL (2013) Effect of brief daily resistance training on occupational neck/shoulder muscle activity in office workers with chronic pain: randomized controlled trial. BioMed Res Int. https://doi.org/10.1155/2013/262386
Lister D, Jenicek E, Preissner P (1998) Productivity and indoor environmental conditions research: an annotated bibliography for facility engineers. Final report Army Construction Engineering Research Lab, Champaign
Loghmani A, Golshiri P, Zamani A, Kheirmand M, Jafari N (2013) Musculoskeletal symptoms and job satisfaction among office-workers: a cross-sectional study from Iran. Acta Med Acad 42(1):46–54. https://doi.org/10.5644/ama2006-124.70
Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D (2010) The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br J Sports Med 44(5):376–381. https://doi.org/10.1136/bjsm.2009.066837
Madeleine P, Lundager B, Voigt M, Arendt-Nielsen L (1999) Shoulder muscle co-ordination during chronic and acute experimental neck-shoulder pain. An occupational pain study. Eur J Appl Physiol Occup Physiol 79(2):127–140. https://doi.org/10.1007/s004210050486
Magnusson SP (1998) Passive properties of human skeletal muscle during stretch maneuvers. Scand J Med Sci Sports 8(2):65–77. https://doi.org/10.1111/j.1600-0838.1998.tb00171.x
Mehri A, Letafatkar A, Khosrokiani Z (2020) Effects of corrective exercises on posture, pain, and muscle activation of patients with chronic neck pain exposed to anterior-posterior perturbation. J Manip Physiol Ther 43(4):311–324. https://doi.org/10.1016/j.jmpt.2018.11.032
Miraglia M, Johns G (2016) Going to work ill: a meta-analysis of the correlates of presenteeism and a dual-path model. J Occup Health Psychol 21(3):261. https://doi.org/10.1037/ocp0000015
Morris CE, Greenman PE, Bullock MI, Basmajian JV, Kobesova A (2006) Vladimir Janda, MD, DSc: tribute to a master of rehabilitation. Spine 31(9):1060–1064. https://doi.org/10.1097/01.brs.0000214879.93102.4e
Nejati P, Lotfian S, Moezy A, Moezy A, Nejati M (2014) The relationship of forward head posture and rounded shoulders with neck pain in Iranian office workers. Med J Islam Repub Iran 28:26
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. https://doi.org/10.1097/01.MLR.0000062554.74615.4C
Noroozi MV, Hajibabaei M, Saki A, Memari Z (2015) Prevalence of musculoskeletal disorders among office workers. Jundishapur J Health Sci. https://doi.org/10.5812/jjhs.27157
Ohlendorf D, Erbe C, Nowak J, Hauck I, Hermanns I, Ditchen D, Ellegast R, Groneberg DA (2017) Constrained posture in dentistry–a kinematic analysis of dentists. BMC Musculoskelet Disord 18(1):1–15. https://doi.org/10.1186/s12891-017-1650-x
Page P (2011a) Cervicogenic headaches: an evidence-led approach to clinical management. Int J Sports Phys Ther 6(3):254
Page P (2011b) Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther 6(1):51
Page P, Frank CC, Lardner R (2010) Assessment and treatment of muscle imbalance: the Janda approach. Human kinetics, Champaign
Phadke V, Camargo P, Ludewig P (2009) Scapular and rotator cuff muscle activity during arm elevation: a review of normal function and alterations with shoulder impingement. Braz J Phys Ther 13(1):1–9. https://doi.org/10.1590/S1413-35552009005000012
Pietropaoli D, Ortu E, Giannoni M, Cattaneo R, Mummolo A, Monaco A (2019) Alterations in surface electromyography are associated with subjective masticatory muscle pain. Pain Res Manag. https://doi.org/10.1155/2019/6256179
Richardson JT (2011) Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev 6(2):135–147. https://doi.org/10.1016/j.edurev.2010.12.001
Sahrmann S, Azevedo DC, Van Dillen L (2017) Diagnosis and treatment of movement system impairment syndromes. Braz J Phys Ther 21(6):391–399. https://doi.org/10.1016/j.bjpt.2017.08.001
Seidi F, Bayattork M, Minoonejad H, Andersen LL, Page P (2020) Comprehensive corrective exercise program improves alignment, muscle activation and movement pattern of men with upper crossed syndrome: randomized controlled trial. Sci Rep 10(1):1–11. https://doi.org/10.1038/s41598-020-77571-4
Sheikhhoseini R, Shahrbanian S, Sayyadi P, O’Sullivan K (2018) Effectiveness of therapeutic exercise on forward head posture: a systematic review and meta-analysis. J Manip Physiol Ther 41(6):530–539. https://doi.org/10.1016/j.jmpt.2018.02.002
Singla D, Veqar Z (2017) Association between forward head, rounded shoulders, and increased thoracic kyphosis: a review of the literature. J Chiropract Med 16(3):220–229. https://doi.org/10.1016/j.jcm.2017.03.004
Skamagki G, King A, Duncan M, Wåhlin C (2018) A systematic review on workplace interventions to manage chronic musculoskeletal conditions. Physiother Res Int 23(4):e1738. https://doi.org/10.1002/pri.1738
So BC, Szeto GP, Lau RW, Dai J, Tsang SM (2019) Effects of ergomotor intervention on improving occupational health in workers with work-related neck-shoulder pain. Int J Environ Res Pub Health 16(24):5005. https://doi.org/10.3390/ijerph16245005
Sterling M (2011) Whiplash-associated disorder: musculoskeletal pain and related clinical findings. J Man Manip Ther 19(4):194–200. https://doi.org/10.1179/106698111X13129729551949
Sundstrup E, Seeberg KGV, Bengtsen E, Andersen LL (2020) A systematic review of workplace interventions to rehabilitate musculoskeletal disorders among employees with physical demanding work. J Occup Rehabilit 30(4):588–612. https://doi.org/10.1007/s10926-020-09879-x
Szeto GP, Straker L, Raine S (2002) A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl Ergon 33(1):75–84. https://doi.org/10.1016/s0003-6870(01)00043-6
Szeto GP, Straker LM, O’Sullivan PB (2005) A comparison of symptomatic and asymptomatic office workers performing monotonous keyboard work—1: neck and shoulder muscle recruitment patterns. Man Ther 10(4):270–280. https://doi.org/10.1016/j.math.2005.01.005
Ting JZR, Chen X, Johnston V (2019) Workplace-based exercise intervention improves work ability in office workers: a cluster randomised controlled trial. Int J Environ Res Pub Health 16(15):2633. https://doi.org/10.3390/ijerph16152633
Villanueva A, Rabal-Pelay J, Berzosa C, Gutiérrez H, Cimarras-Otal C, Lacarcel–Tejero B, Bataller–Cervero AV (2020) Effect of a long exercise program in the reduction of musculoskeletal discomfort in office workers. Int J Environ Res Pub Health 17(23):9042. https://doi.org/10.3390/ijerph17239042
Welch A, Healy G, Straker L, Comans T, O’Leary S, Melloh M, Sjøgaard G, Pereira M, Chen X, Johnston V (2020) Process evaluation of a workplace-based health promotion and exercise cluster-randomised trial to increase productivity and reduce neck pain in office workers: a RE-AIM approach. BMC Pub Health 20(1):1–15. https://doi.org/10.1186/s12889-020-8208-9
Weon J-H, Oh J-S, Cynn H-S, Kim Y-W, Kwon O-Y, Yi C-H (2010) Influence of forward head posture on scapular upward rotators during isometric shoulder flexion. J Bodyw Mov Ther 14(4):367–374. https://doi.org/10.1016/j.jbmt.2009.06.006
Yaghoubitajani Z, Gheitasi M, Bayattork M, Andersen LL (2021) Online supervised versus workplace corrective exercises for upper crossed syndrome: a protocol for a randomized controlled trial. Trials 22(1):907. https://doi.org/10.1186/s13063-021-05875-5
Zad SS, Patil P (2021) Effectiveness of Janda’s approach in upper cross syndrome in medical students. Ann Rom Soc Cell Biol 25(6):17385–17399
Acknowledgements
We would like to thank the authors' team members for their contributions to the success of this trial.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
ZY and MG: contributed to the study conception and design. ZY: performed clinical examination and data collection. MG and MB: participated in the methodologically development and design of the statistical analysis. ZY: wrote the first draft of the manuscript. LLA: contributed to the comments and suggestions that greatly improved the manuscript. Finally, all the authors revised it critically for important intellectual content, agreed with the content, contributed to the current study’s refinement, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors Zohreh Yaghoubitajani (ZY), Mehdi Gheitasi (MG), Mohammad Bayattork (MB), and Lars Louis Andersen (LLA) declare that they have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by Ethics Committee on the Research at Shahid Beheshti University, Tehran, Iran (approval number: IR.SBU.REC.1399.036 / 2020.06.20).
Consent to publish
Not applicable.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all the individual subjects for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yaghoubitajani, Z., Gheitasi, M., Bayattork, M. et al. Corrective exercises administered online vs at the workplace for pain and function in the office workers with upper crossed syndrome: randomized controlled trial. Int Arch Occup Environ Health 95, 1703–1718 (2022). https://doi.org/10.1007/s00420-022-01859-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-022-01859-3